Pulmonary rehabilitation (PR) programs improve exercise capacity in patients with chronic obstructive pulmonary disease (COPD) and interstitial lung disease (ILD),1,2 but few studies compare results between both pathologies.
It is not yet obvious whether gains in 6-min walk distance (6MWD) accomplished by patients with ILD are comparable to those with COPD, because existing studies have yielded conflicting results.3 There are studies that reported similar improvement in exercise tolerance and quality of life in patients with COPD and non-obstructive lung disease.4,5 However, the duration of benefit may be shorter lived than that seen after PR among patients with COPD.6 Also, the type and severity of ILD may also influence outcomes of PR. A recent systematic review and meta-analysis on the impact of pulmonary rehabilitation in patients with idiopathic pulmonary fibrosis showed a growing body of evidence of its benefit in exercise tolerance and quality of life.7
The aim of our study was to evaluate the effect of PR on exercise capacity using 6-min walk test (6MWT) within and between COPD and ILD patients.
Outcomes were the change in 6MWD and maximum heart rate (HRmax), and the comparison of these changes between groups according to dyspnea level classified by modified Medical Research Council scale (mMRC).
This study was performed at Pulmonary Rehabilitation Unit, Hospital Pulido Valente, Pulmonology Department of Centro Hospitalar Universitário Lisboa Norte, Lisboa, Portugal.
COPD and ILD patients with mMRC of 2 and above who had completed an outpatient PR program at least 8-weeks long during 2016 were retrospectively selected and analyzed.
The PR program was designed individually, according to the limitations of each patient. It included therapeutic exercise, daily life activities training, breathing control techniques, individualized self-management education and, if indicated, airways clearance and adaptation to long-term oxygen therapy.
Using SPSS statistics, Chi-squared and Mann–Whitney tests were carried out for comparison of qualitative and quantitative variables, respectively.
Eighty-one patients were included in the study: n=50 patients with COPD with median (P25;P75) post-bronchodilator forced expired volume in 1 second (FEV1) of 44% predicted (34;59); n=31 patients with ILD with median (P25;P75) total lung capacity (TLC) of 68% predicted (53;82).
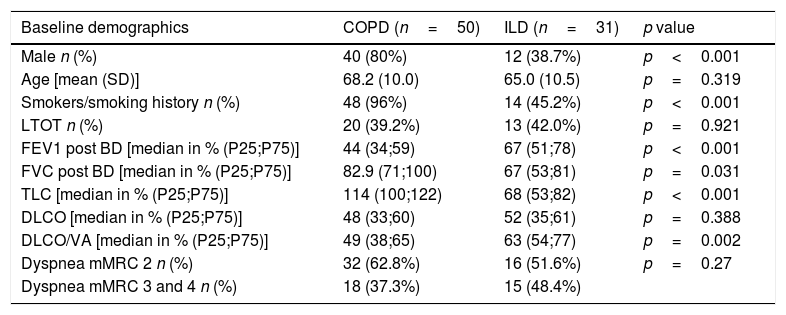
Table 1 represents the main features of the patients studied. We highlight the statistically significantly higher number of male patients and active or former smokers among COPD patients. As expected, there was a lower post bronchodilator FEV1 among COPD patients, and a lower TLC in ILD patients.
Baseline demographics (n=81).
| Baseline demographics | COPD (n=50) | ILD (n=31) | p value |
|---|---|---|---|
| Male n (%) | 40 (80%) | 12 (38.7%) | p<0.001 |
| Age [mean (SD)] | 68.2 (10.0) | 65.0 (10.5) | p=0.319 |
| Smokers/smoking history n (%) | 48 (96%) | 14 (45.2%) | p<0.001 |
| LTOT n (%) | 20 (39.2%) | 13 (42.0%) | p=0.921 |
| FEV1 post BD [median in % (P25;P75)] | 44 (34;59) | 67 (51;78) | p<0.001 |
| FVC post BD [median in % (P25;P75)] | 82.9 (71;100) | 67 (53;81) | p=0.031 |
| TLC [median in % (P25;P75)] | 114 (100;122) | 68 (53;82) | p<0.001 |
| DLCO [median in % (P25;P75)] | 48 (33;60) | 52 (35;61) | p=0.388 |
| DLCO/VA [median in % (P25;P75)] | 49 (38;65) | 63 (54;77) | p=0.002 |
| Dyspnea mMRC 2 n (%) | 32 (62.8%) | 16 (51.6%) | p=0.27 |
| Dyspnea mMRC 3 and 4 n (%) | 18 (37.3%) | 15 (48.4%) |
SD, standard deviation; BD, bronchodilator; DLCO, diffusing capacity for carbon monoxide; FEV1, forced expired capacity in 1 second; FVC, forced vital capacity; LTOT, long-term oxygen therapy; mMRC, modified Medical Research Council dyspnea scale; TLC, total lung capacity; VA, alveolar volume.
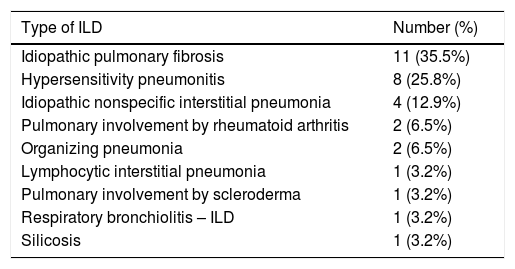
Based on Table 2 most ILD patients had IPF (35.5%) and hypersensitivity pneumonitis (25.8%).
Type of ILD (n=31).
| Type of ILD | Number (%) |
|---|---|
| Idiopathic pulmonary fibrosis | 11 (35.5%) |
| Hypersensitivity pneumonitis | 8 (25.8%) |
| Idiopathic nonspecific interstitial pneumonia | 4 (12.9%) |
| Pulmonary involvement by rheumatoid arthritis | 2 (6.5%) |
| Organizing pneumonia | 2 (6.5%) |
| Lymphocytic interstitial pneumonia | 1 (3.2%) |
| Pulmonary involvement by scleroderma | 1 (3.2%) |
| Respiratory bronchiolitis – ILD | 1 (3.2%) |
| Silicosis | 1 (3.2%) |
ILD, interstitial lung disease.
Forty-eight patients showed a clinically significant increase in 6MWD (≥30m) at the end of the program with no statistically significant difference between groups (52% of patients with COPD vs 71% patients with ILD; p=0.091). COPD patients increased the distance by a mean of 54.3m, and patients with ILD by a mean of 49.3m.
Forty-three patients had a reduction in HRmax in 6MWT at the end of the program (−14bpm±13) with no statistically significant difference between groups (COPD 58% vs ILD 45%; p=0.260).
Furthermore, forty patients decreased the 6MWT level of dyspnea according to modified Borg score at the end of the program, with a median of 0 (−2;0). There was also no statistically significant difference between number of patients that improved dyspnea between groups (COPD 48% vs ILD 52%; p=0.384). Muscle fatigue (modified Borg score) at 6MWT also diminished in twenty-nine patients with a median of 0 (−1;1). Similarly, there was no statistically significant difference between groups (COPD 40% vs ILD 29%; p=0.187).
No statistically significant difference was found for primary outcomes (6MWD and HRmax) when comparing both disease groups with the same dyspnea level: for COPD vs ILD patients with mMRC 2: 6MWD p=0.072 and HRmax p=0.540; for COPD vs ILD patients with mMRC 3 or 4: 6MWD p=0.247 and HRmax p=0.247.
According to dyspnea level, the mean increased distance in COPD group with mMRC 2 was 71.7m and in ILD group with mMRC 2 was 66.4m (p=0.810); in COPD group with mMRC 3 and 4 was 23.4m and in ILD group with mMRC 3 and 4 was 31.1m (p=0.656).
This study shows that functional exercise capacity, physiological heart rate response to exercise training, dyspnea and muscle fatigue have similar improvements in COPD and ILD patients; this shows the benefits of PR in both diseases and supports some published literature.4,5 Since these diseases are so distinct, we decided to find a feature in common so we could compare them. Dyspnea is one of the most important symptoms in both diseases and one of the main reasons for referring these patients for to PR.
To the best of our knowledge this is the first comparison of PR results in these diseases according to the same level of dyspnea.
Additionally, we think it is important to point out the percentage of IPF patients on the ILD group (35.5%), which is not negligible, reinforcing the increasing body of evidence of pulmonary rehabilitation benefits in these patients.7
Our results support the use of pulmonary rehabilitation with comparable benefits across distinct chronic respiratory diseases.
Conflicts of interestThe authors have no conflicts of interest to declare.