Between 2020 and 2022, the COVID-19 pandemic markedly altered global patterns of respiratory illnesses, as evidenced by a significant decline in hospitalization rates for influenza from 6.1% to 0.3%.1 Concurrent with the easing of COVID-19 control measures in China in 2022, there has been a notable increase in respiratory infection cases among children in Northern China during the autumn and winter months. This trend has attracted significant attention by the World Health Organization due to its potential implications for public health.2
The China Influenza Surveillance Weekly Report has noted a significant increase in the Influenza-Like Illness percentage (ILI%) among sentinel hospitals in the northern provinces. Current figures indicate an ILI% of 7.4%, a marked increase from the 2.5%, 3.0%, and 2.0% reported during the same period in the years 2020-2022, respectively.3 Globally, the annual incidence rate of influenza among children typically ranges from 20% to 30%.4 During the 2017-2018 influenza season, recorded incidence rates for children aged 0-4 and 5-14 in Beijing were 18.7%5 and 21.7%,6 respectively. Notably, the past month has seen a dramatic rise in the detection rate of the influenza virus among children aged 0-14 in Beijing's medical institutions, now exceeding 48%. Additionally, the outpatient volume for respiratory infections has tripled in comparison to the previous year, with over 90% of these cases being cluster infections within educational and childcare settings.
In recent times, China is encountering an increasingly intricate scenario in respiratory illnesses, characterized by a predominant disease co-existing with multiple infections. The National Institute of Respiratory Diseases' latest data indicates a shift in the dominant influenza strain this season. Notably, the A(H3N2) subtype's prevalence has risen substantially compared to the previous two years.1 The National Influenza Center's surveillance report highlights that in March, influenza viruses emerged as the primary pathogens, showing a positive detection rate of 55%. By May 2023, COVID-19′s positivity rate peaked at 40%, then decreased to 19% by August 2023, while influenza rates stood at 2.7%. December 2023′s data reveals a continued upward trend in influenza virus detection across southern and northern provinces, at 12.7%, with COVID-19 cases accounting for 4%. Remarkably, Mycoplasma infections constitute 20%-30% of respiratory infections in children.3 In certain pediatric hospitals, over 80% of pneumonia cases in children test positive for Mycoplasma, and 30-40% of these are mixed infections, predominantly involving Mycoplasma pneumoniae combined with influenza virus or respiratory syncytial virus.
Such mixed infections notably exacerbate the risk of adverse outcomes in children. A UK study involving 6,965 COVID-19 patients undergoing multi-pathogen respiratory testing revealed that hospitalized individuals with co-infections had a significantly higher likelihood of requiring mechanical ventilation (increased risk by 4.14 times, 95% CI: 2.00-8.49) and experiencing in-hospital mortality (increased risk by 2.35 times, 95% CI: 1.07-5.12). Additionally, the risk of severe clinical manifestations in children, such as high fever seizures, respiratory failure, and myocardial injury, also saw a significant rise.7
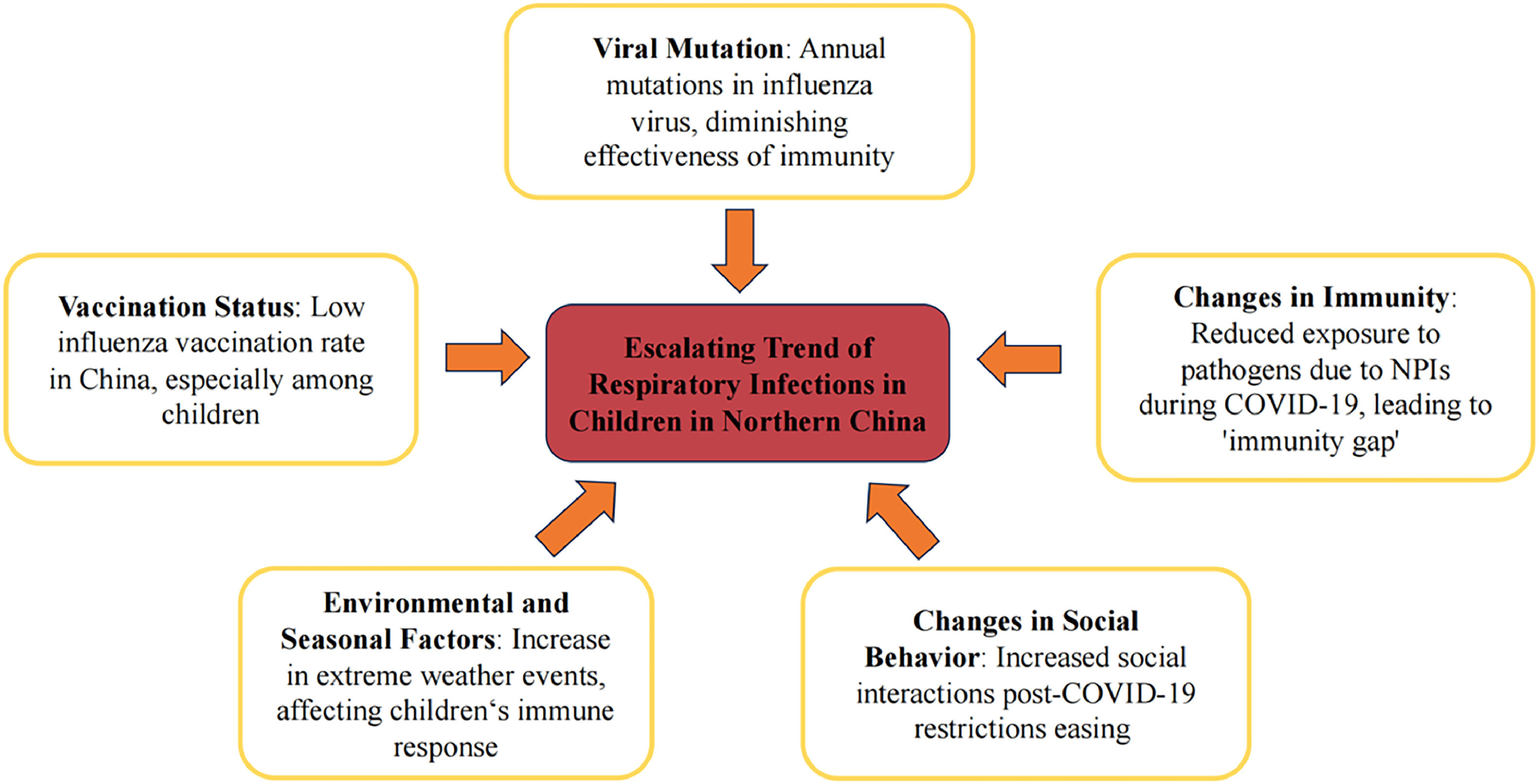
The recent upsurge in respiratory infections among children in Northern China can be attributed to a complex interplay of factors, as illustrated in Fig. 1. These include: 1. Viral Mutation: The influenza virus is known for its high variability, with frequent mutations potentially reducing the effectiveness of immunity acquired from previous strains. This constant evolution plays a crucial role in the fluctuating incidence rates. 2. Changes in Immunity: The strict non-pharmaceutical interventions (NPIs) implemented during the COVID-19 pandemic, such as mask-wearing and social distancing, have markedly reduced young children's exposure to respiratory pathogens. This decreased exposure may have hindered the development of mucosal immunity in their respiratory tracts, thus creating a vulnerable 'immunity gap' population and heightening susceptibility among children.83. Vaccination Status: In China, the influenza vaccination rate remains low due to factors such as limited public awareness, inadequate vaccine supply, a narrow range of vaccine options, and restricted coverage of free vaccination policies. The average annual influenza vaccination rate is about 2% to 3% for the general population, and approximately 26% for children aged 5 years and below.9 This rate is substantially lower than those observed in developed countries. 4. Changes in Social Behavior: The easing of social restrictions and the reopening of schools have led to an increase in children's social interactions, potentially facilitating a higher transmission rate of respiratory diseases. 5. Environmental and Seasonal Factors: Recent data from the China Meteorological Administration highlight an increase in extreme weather events, including eight instances of sandstorms since June 2023, the highest in the past decade.10 Such conditions, coupled with children's less developed immune systems and lower adaptability to climatic changes, increase their vulnerability to bacterial invasion and infection. These hypotheses, while providing a multifaceted perspective on the rising trend, also underscore the complexity of addressing respiratory infections in a post-pandemic era.
In response to the rising epidemic of mixed infections in children, the Chinese government has implemented several innovative measures for epidemic prevention, focusing on enhancing healthcare services. A key initiative is the integration of big data and intelligent systems in hospitals, which has revolutionized medical service capabilities. This includes providing continuous access to vital information about fever clinics, essential for managing respiratory infections. A standout feature of this technological advancement is the real-time hospital registration monitoring system. Patients now can see current wait times and the number of people ahead of them in line, significantly improving pre-triage processes. This functionality not only streamlines patient flow but also reduces waiting times, enhancing the efficiency of healthcare delivery. In addition, the healthcare system has broadened its offerings to encompass online consultations and prescription services. In an innovative move, medications are now delivered directly to patients' homes by third-party entities, at no extra cost. This shift from traditional in-person medical services to a digital format is crucial in reducing the risk of pathogen transmission in hospital environments, thereby markedly decreasing the potential for cross-infection. These measures mark a strategic transformation in healthcare delivery, aiming to provide effective medical care while simultaneously controlling the spread of infections in a post-pandemic landscape.
The advent of new infectious diseases, particularly acute respiratory infections, has highlighted the critical need for a robust and responsive public health emergency management system in China. This situation urgently calls for the development of a comprehensive early warning and monitoring system, specifically designed for acute respiratory infectious diseases. A key focus in addressing the mixed infection epidemic among children is the investigation into drug resistance mutations of the involved pathogens. Understanding their susceptibility or resistance to current antiviral drugs is crucial for devising effective treatment strategies. Concurrently, the expansion of influenza vaccination programs is paramount, especially for high-risk groups like children and the elderly. Enhancing vaccination coverage is imperative to reduce the risks of hospitalization and mortality in the event of influenza outbreaks. Additionally, the timely and transparent sharing of infection data with the public is essential. This should be accompanied by the distribution of scientifically sound information to promote public understanding and prevent unnecessary panic. Implementing such measures is vital not only for immediate control of the epidemic but also for establishing a resilient public health infrastructure capable of confronting future challenges.
The observation of post-pandemic immunity gaps in both the USA and UK underscores the global nature of this challenge.11 China's response to post-pandemic respiratory infections in children has been exemplary, demonstrating the effectiveness of a proactive and integrated public health strategy. This approach is characterized by the strategic use of technology, including big data and intelligent systems, to bolster healthcare delivery and disease surveillance. Furthermore, prioritizing the expansion of vaccination efforts, particularly among vulnerable populations, and establishing comprehensive early warning systems for infectious diseases emerge as pivotal measures. Enhanced international collaboration, through the exchange of data, experiences, and control strategies, is essential. Such cooperation fosters a global network capable of leveraging technological and policy innovations to effectively counter the threat of emerging infectious diseases.
Declare of AI program assistancePortions of this manuscript were assisted by AI-based tools for language polishing. All final decisions and edits were made by the authors.
Declaration about figure originalityFig. 1 is original and was created by the authors for this manuscript.
FundingThis work was supported by The Special Research Fund for Central Universities, Peking Union Medical College (2022-I2M-C&T-B-065, 2022-I2M-C&T-B-060); National High-Level Hospital Clinical Research Funding (2022-PUMCH-A-018, 2022-PUMCH-C-043); National Key R&D Program of China (2022YFC2407404); Beijing Municipal Science & Technology Commission (Z211100002921058).
CRediT authorship contribution statementKun Wang: Data curation, Formal analysis, Investigation, Writing – original draft. Zhuoheng Lv: Data curation, Formal analysis, Investigation, Writing – original draft. Shuofeng Li: Data curation, Formal analysis, Investigation, Writing – original draft. Hang Yi: Conceptualization, Formal analysis, Investigation, Writing – review & editing.