Inhalers mishandling remains an important clinical problem.1 However, a large proportion of patients refer to a lack of effective training from their health care professionals and inhaler technique is seldom systematically checked up on during medical visits.2 Actually, even after being learned correctly, inhaler technique can deteriorate over time. The aim of this study was to evaluate if educational intervention with COPD outpatients on the correct use of inhaler devices (IDs), can sustain long-term improvement in inhalation technique and to assess the inhaler and patient-related characteristics that are associated with some improvement in inhalation technique.
An interventional study was conducted in the outpatient respiratory care of Guimarães hospital. Stable COPD patients ≥ 40 years diagnosed according to GOLD criteria were evaluated in two different medical visits,3 with a 10–12 months interval between them. They were recruited consecutively and evaluated on a first medical visit between March 2016 and May 2017. Refusal to participate and inability to understand simple questionnaires were the exclusion criteria. In the first visit, a survey of demographic and clinical data and the Portuguese versions of the Graffar social classification and the Beliefs about Medicines Questionnaires were conducted.4 The BMQ has a Necessity and a Concern scale, assessing respectively the beliefs about the medication necessity and concerns about the side-effects of medication. Symptom evaluation was done using the COPD Assessment Test (CAT) and the Medical Research Council Dyspnea Questionnaires (mMRC). The number of acute exacerbations of COPD in the previous year was recorded. All participants performed at least one spirometry according to ERS/ATS criteria and referenced according to the Global Lung Function Initiative prediction equations (GLI 2012).5,6 Participants were then invited to demonstrate the use of their prescribed IDs, and the inhaler technique was accessed by using previous defined checklists of essential steps and critical errors. All the participants received face-to-face demonstration and training with inhalers containing placebo medications, until correct usage was achieved. After 10–12 months, participants were invited by mail for a second medical visit, and a re-evaluation of inhalers’ technique was conducted. The difference in number of critical errors between the two visits, expressed as qualitative, was defined as outcome. A statistical analysis was then performed.
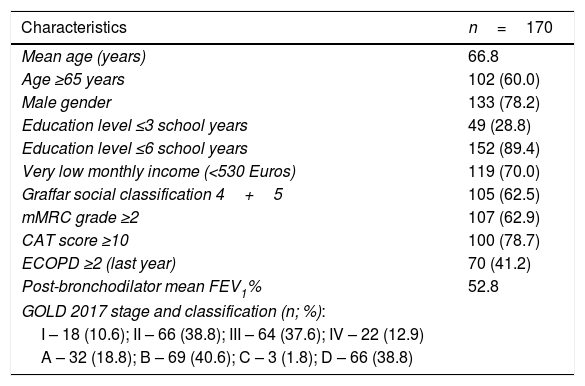
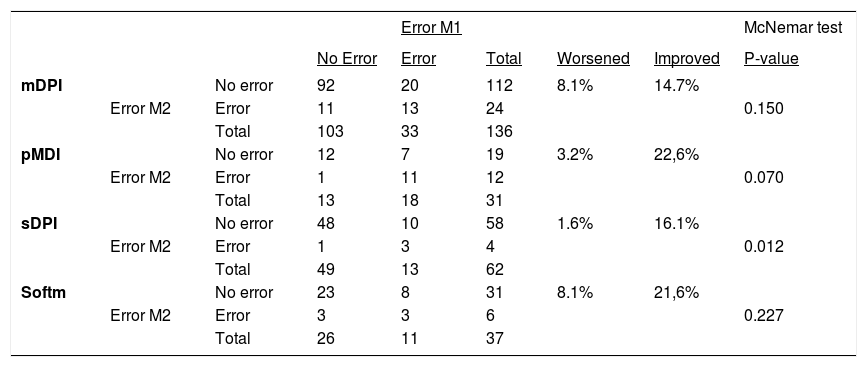
Only 201 patients agreed to participate in the second medical visit. From these, 31 were excluded because they were using different IDs. We evaluated 170 participants performing 266 inhalation manoeuvres. The main demographic, clinical and functional characteristics of patients are described in Table 1. Ten different IDs were examined, in a total of 31 (11.7%) pMDI, 63 (23.7%) single-dose inhalers (sDPI) 136 (51.1%) multiple dose inhalers (mDPI) and 37 (13.9%) SMI-Respimat®. An improvement in number of critical errors was observed in 50 (18.8%) and a worsening in 21 (7.9%) demonstrations, and critical errors were more often related to inhalation manoeuvres than to priming/loading. There was a general improvement in critical errors in all types of IDs, but with different statistical significances (Table 2). A worsening in the total number of critical errors was observed in 20 (8.8%) patients and an improvement in 47 (25.9%). Improvement was significantly related to CAT score (CAT<10: 22.2% worsened and 22.2% improved inhalation technique; CAT≥10: 6% worsened and 25% improved inhalation technique, p=0.037), but not to any other demographic, clinical or functional characteristics of patients. In the subset of patients who improved their inhalation technique, males had a higher average BMQ Necessity score than females (mean BMQ Necessity score were respectively 21.97 and 17.88, p=0.017).
Demographic, clinical and functional characteristics of COPD patients.
| Characteristics | n=170 |
|---|---|
| Mean age (years) | 66.8 |
| Age ≥65 years | 102 (60.0) |
| Male gender | 133 (78.2) |
| Education level ≤3 school years | 49 (28.8) |
| Education level ≤6 school years | 152 (89.4) |
| Very low monthly income (<530 Euros) | 119 (70.0) |
| Graffar social classification 4+5 | 105 (62.5) |
| mMRC grade ≥2 | 107 (62.9) |
| CAT score ≥10 | 100 (78.7) |
| ECOPD ≥2 (last year) | 70 (41.2) |
| Post-bronchodilator mean FEV1% | 52.8 |
| GOLD 2017 stage and classification (n; %): | |
| I – 18 (10.6); II – 66 (38.8); III – 64 (37.6); IV – 22 (12.9) | |
| A – 32 (18.8); B – 69 (40.6); C – 3 (1.8); D – 66 (38.8) | |
Note: Data shown as mean or n (%).
Abbreviations: mMRC, modified Research Council Dyspnoea Questionnaire; CAT, COPD Assessment Test; ECOPD, chronic obstructive pulmonary disease acute exacerbations; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
Variation on critical errors in the different groups of inhaler devices.
| Error M1 | McNemar test | |||||||
|---|---|---|---|---|---|---|---|---|
| No Error | Error | Total | Worsened | Improved | P-value | |||
| mDPI | No error | 92 | 20 | 112 | 8.1% | 14.7% | ||
| Error M2 | Error | 11 | 13 | 24 | 0.150 | |||
| Total | 103 | 33 | 136 | |||||
| pMDI | No error | 12 | 7 | 19 | 3.2% | 22,6% | ||
| Error M2 | Error | 1 | 11 | 12 | 0.070 | |||
| Total | 13 | 18 | 31 | |||||
| sDPI | No error | 48 | 10 | 58 | 1.6% | 16.1% | ||
| Error M2 | Error | 1 | 3 | 4 | 0.012 | |||
| Total | 49 | 13 | 62 | |||||
| Softm | No error | 23 | 8 | 31 | 8.1% | 21,6% | ||
| Error M2 | Error | 3 | 3 | 6 | 0.227 | |||
| Total | 26 | 11 | 37 |
Note and abbreviations: Error Moment 1: first assessment; Error Moment 2: 2nd assessment; errors shown as number of demonstrations; Worsened/Improved described as % of demonstrations.
A significant number of papers explore the effects of educational intervention on frequency of inhaler errors,7 and a significant improvement of inhalation technique is usually reported. In a recent systematic review of inhalers’ critical errors, 11 out of 21 studies exploring the relationship between previous inhaler instructions and frequency of inhaler errors found a positive association between previous instructions and a better inhaler technique.8 In the present study, some improvement in inhalation technique was achieved after a single education intervention in all types of IDs, with statistical significance in the group of inhalers with an easy feed-back to the patient that a significant amount of medication had been inhaled. It appears that these devices attributes, by improving patient confidence in their use, improve the maintenance of a correct inhaler technique. We found a significant positive association between symptoms and improvement of the inhaler technique. We hypothesized that more symptomatic patients can be more motivated to learn how to use inhalers properly. We also found that male patients who improve their inhalation technique seem to greater belief in need for medication than women. Probably men, but not women, have to believe in the need of medication to improve their learning of correct inhalation techniques. This information is new and needs to be confirmed by other studies.
Author contributionsDuarte-de-Araújo conceived and developed the study, carried out the collection of data and data interpretation, wrote the first draft and collaborated in the final text. Pedro Teixeira carried out the statistical analysis, contributed to the section on methods and results, and collaborated in the final writing. Venceslau Hespanhol reviewed the final draft. Jaime Correia-de-Sousa reviewed all the drafts and collaborated in the final writing. All the authors approved the final manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare.