Aspergilloma is a saprophytic infection that colonizes pre-existing cavities in the lung. These cavities are caused by tuberculosis, bronchiectasis, lung cancer and other pulmonary diseases. Development of aspergilloma in the residual cavities after pulmonary hydatid cyst surgery is rarely described in terms of coexistence of the two conditions. We describe 3 cases of pulmonary aspergilloma grafted in a residual cavity of cystectomy for hydatid disease.
Aspergiloma é uma infecção saprófita que coloniza cavidades pré-existentes no pulmão. Estas cavidades são causadas por tuberculose, bronquiectasias, cancro do pulmão e outras doenças pulmonares. O desenvolvimento de aspergiloma em cavidades residuais, após cirurgia pulmonar de quisto hidático, raramente é descrito em termos de coexistência das duas condições. Descrevemos 3 casos de enxerto de aspergiloma pulmonar numa cavidade residual de cistectomia para doença hidática.
Aspergilloma is a fungal infection which developed in the pre-existing pulmonary cavities. Grafted aspergilloma in the lung cavity after conservative treatment of pulmonary hydatid cyst or co-existence of the both pathologies are rare.
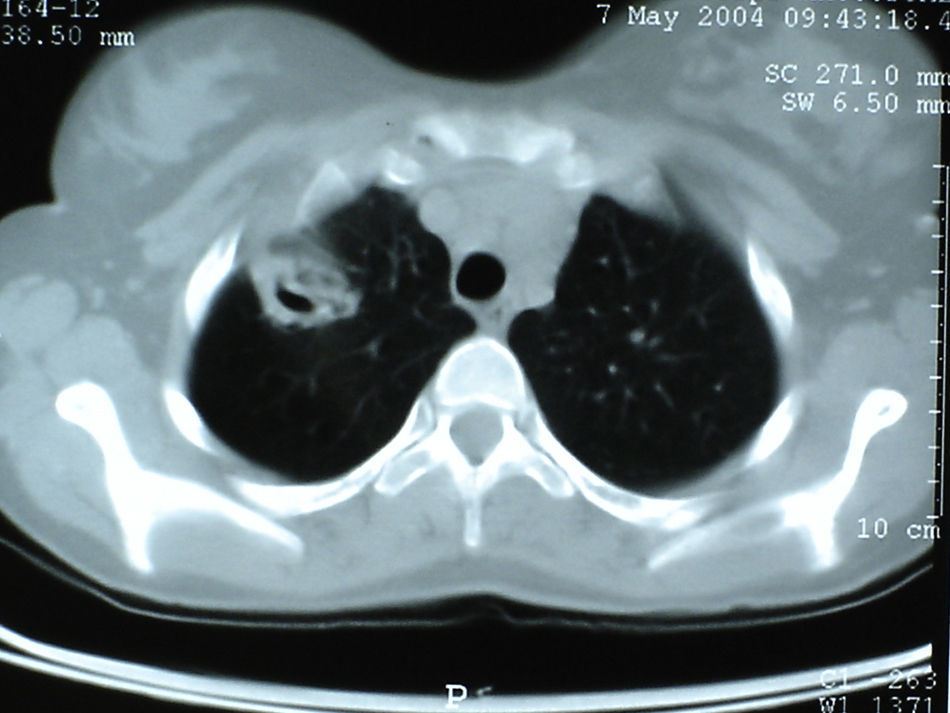
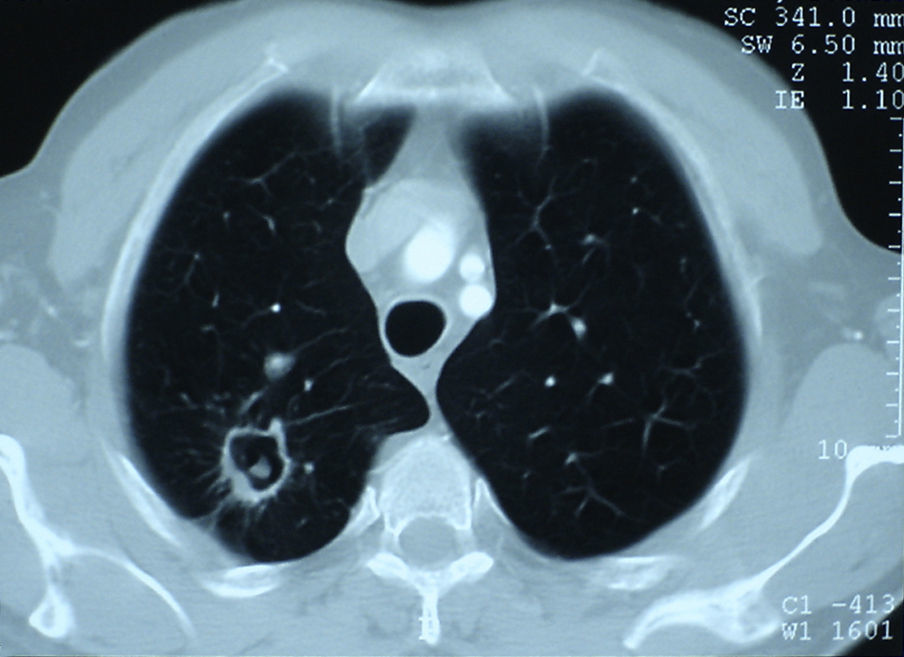
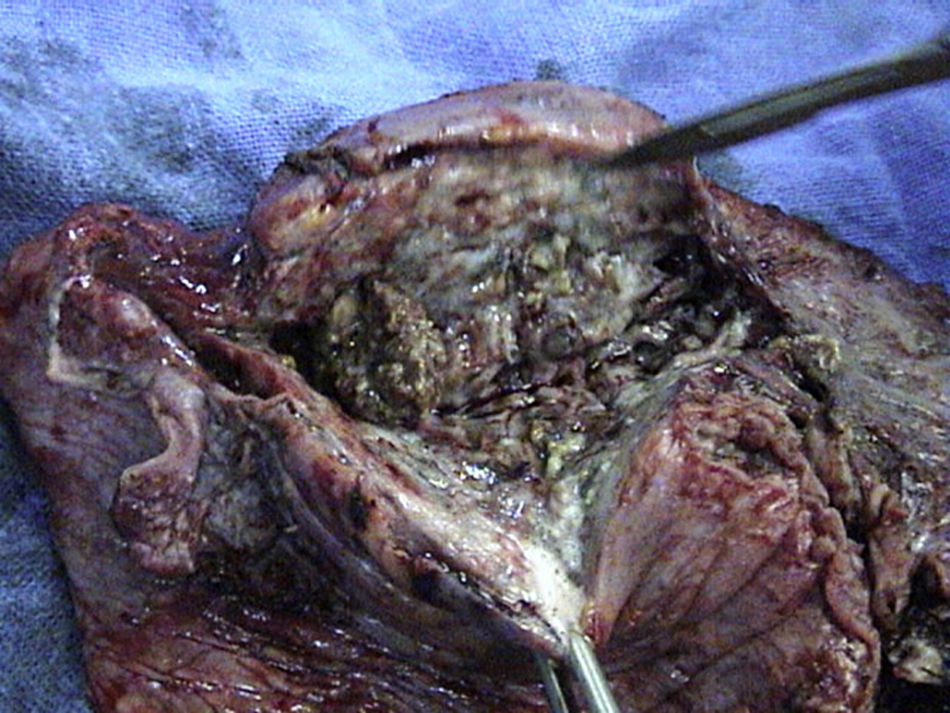
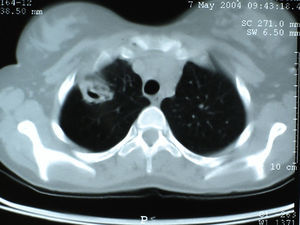
Cases 1 and 2A 35-year-old man and a 56-year-old man who had been operated on 15 and 2 years earlier, respectively, for hydatid cyst of the upper right lobe (cystectomy with and without capitonnage), both presented to our department with minimal hemoptysis and cough. Computed tomography (CT) scan showed an excavated mass of the ventral and posterior segment of the right upper lobe, respectively (Figs. 1 and 2), and bronchoscopy localized the origin of hemoptysis in the upper right bronchus. We performed a right upper lobectomy. Macroscopic examination of the specimen showed the presence of aspergillus material (Fig. 3), confirmed by histological exam. Itraconazole 100mg/day was given for 3 months.
The patients remained asymptomatic with normal radiological control after more than 6 months.
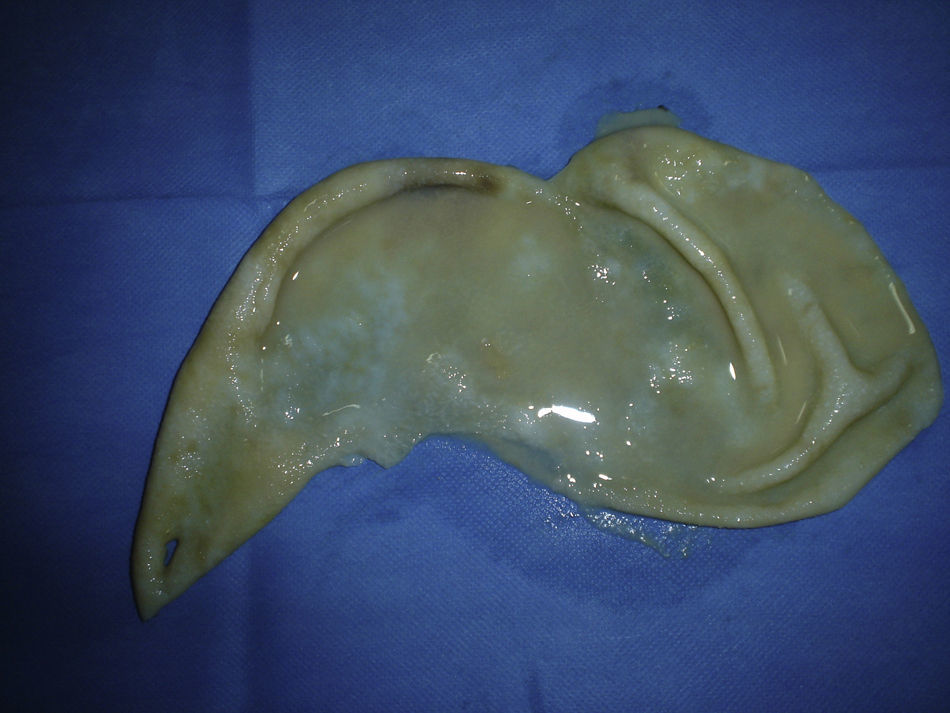
Case 3A 52-year-old man, with pulmonary tuberculosis 30 years prior, with fibrotic changes in both lungs. Four months earlier he had had a cystectomy and capitonnage of a ruptured right lung hydatid cyst of the lower lobe (Fig. 4), and presented to our department with hemoptysis. A TB sputum smear was negative. A right lower lobectomy was performed and postoperative course was uneventful. A microscopic examination of the lower lobe showed the remaining of bronchial communications and a colonization by Aspergillus sp. within the hydatid cavity.
DiscussionPulmonary aspergilloma is a saprophytic infection which occurs as a colonizer of pre-existing pulmonary cavity lesions of any etiology such as sequelae tuberculosis, sarcoidosis, bronchiectasis, cavitatory neoplasia and lung abscess, producing a fungus ball or a mycetoma.1,2
Aspergilloma has rarely been described in operated hydatid cyst cavities in immunocompetent patients, but the coexistence of fungi with a pulmonary hydatid cyst is seen more frequently in immunocompromised patients.
The clinical presentation of pulmonary hydatid cysts depends on whether the cyst is intact or ruptured. A complicated cyst is defined as one that has ruptured into a bronchus, pleural cavity or biliary tree. Intact cysts are either incidental findings or present with cough, dyspnea or chest pain. In addition to these symptoms, patients with a complicated cyst may present with expectoration of cystic contents, repetitive hemoptysis, productive sputum, fever or anaphylactic shock.
The surgical treatment of lung hydatid cyst aims to avoid lung parenchyma resection. This surgery is based on the removal of the cyst membrane (cystectomy or pericystectomy), the closure of bronchial fistulas, and eventually obliteration of the residual cavity with sutures (the capitonnage).3 The capitonnage is not obligatory in the opinion of some surgeons since good results can also be obtained when the residual cavity spontaneously obliterates.4
In the case of persistence of the non-obliterated cavity or bronchial fistulas the aspergilloma can form, and life threatening hemoptysis may be the commonest mode of presentation. Residual cavities can also occur after capitonnage if the sutures break or tear the tissue.
In the English and French literature there are very few reports of association of aspergilloma and operated or unoperated hydatid cavity. The capitonnage was performed in some cases and wedge resection of co-existent aspergilloma and lung hydatid cyst was described in one case.5
Radiological diagnosis is made upon visualizing a well-defined heterogeneous density within a pre-formed cyst cavity, separated from the cyst wall by an air crescent. CT usually reveals globules of gas within the hyphal ball, which may be loose or attached to the cavity wall by granulation tissue.6 With effort, the fungus ball can often be shown to be mobile within the cavity when the ball does not fill the entire cavity.
The recommended surgical treatment of aspergilloma includes lung resection if the pulmonary function tests are adequate,7 as was the case with our patients. In high-risk patients the cavernostomy can be performed.8
In the case of larger hydatid cavities complicated with aspergilloma we prefer safe anatomic lung resection because this latter avoids the uncertainty of how much parenchyma should be removed.
In the other case, even if complicated hydatid cysts can already be colonized by Aspergillus, without apparent clinical symptoms we prefer to perform simple cystectomy with bronchial closure and capitonnage with a complementary medical anti-fungal therapy.
Finally, aggressive surgical treatment with lung resection and anti-fungal therapy for pulmonary aspergilloma in residual hydatid cavities is safe and effective, and can achieve favorable outcomes.
Larger hydatid cysts present an increased risk for secondary infection, particularly those extending to the hilum.9 Long-term follow-up after cystectomy is recommended, especially when residual cavities are present.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.