Cigarette smoke contains a mixture of over 5000 chemicals many of which harm the human body causing a broad range of diseases. With approximately 5 million tobacco-related deaths annually, smoking is the leading cause of preventable premature mortality in the world.1 Death is mainly caused by lung cancer, ischemic heart disease, chronic obstructive pulmonary disease, and stroke.2,3
Tobacco is one of the most main causes of respiratory diseases.4
Smoking is also recognized as a risk factor for interstitial lung disease (ILD). The relationship of smoking with each of these entities has generally been established on the basis of epidemiologic evidence.5 The relationship between cigarette smoking and pulmonary Langerhans cell histiocytosis (PLCH), respiratory bronchiolitis (RB), respiratory bronchiolitis-associated interstitial lung disease (RB-ILD), and desquamative interstitial pneumonia (DIP) is well described.6–9 Data suggesting an association between cigarette smoking and acute eosinophilic pneumonia (AEP) are also emerging, whereas the relationship between smoking and idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia remains uncertain.10,11
The risk of lung cancer, heart disease, chronic lung disease, stroke, and other cancers diminishes rapidly after quitting.12
Smoking cessation maybe the most important and cost-effective therapeutic option7 for smoker with smoking-related ILDs. Smoking cessation should be strongly encouraged in these patients, and they should be offered effective treatment.4
All physicians should strongly advise every patient who smokes to quit because evidence shows that physician advice to quit smoking increases abstinence rates.13 Evidence-based recommendations indicate that smoking cessation programs are useful in helping smokers to quit,13 but the powerful addictive qualities of nicotine create a huge hurdle, even for those with a strong desire to quit. Once established, smoking is a very difficult addiction to break.
The majority of smokers persist in tobacco use for many years and typically cycle through multiple periods of remission and relapse. It has been shown that approximately 80% of smokers who attempt to quit on their own relapse within the first month of abstinence and only about 3–5% remain abstinent at 6 months.14 This reflects the chronic relapsing nature of tobacco dependence. Treatment for smoking cessation includes various methods, from simple medical advice to pharmacotherapy. Evidence-based recommendations indicate that although counseling and medication on their own are helpful for treating tobacco dependence when used in combination they are more effective.13
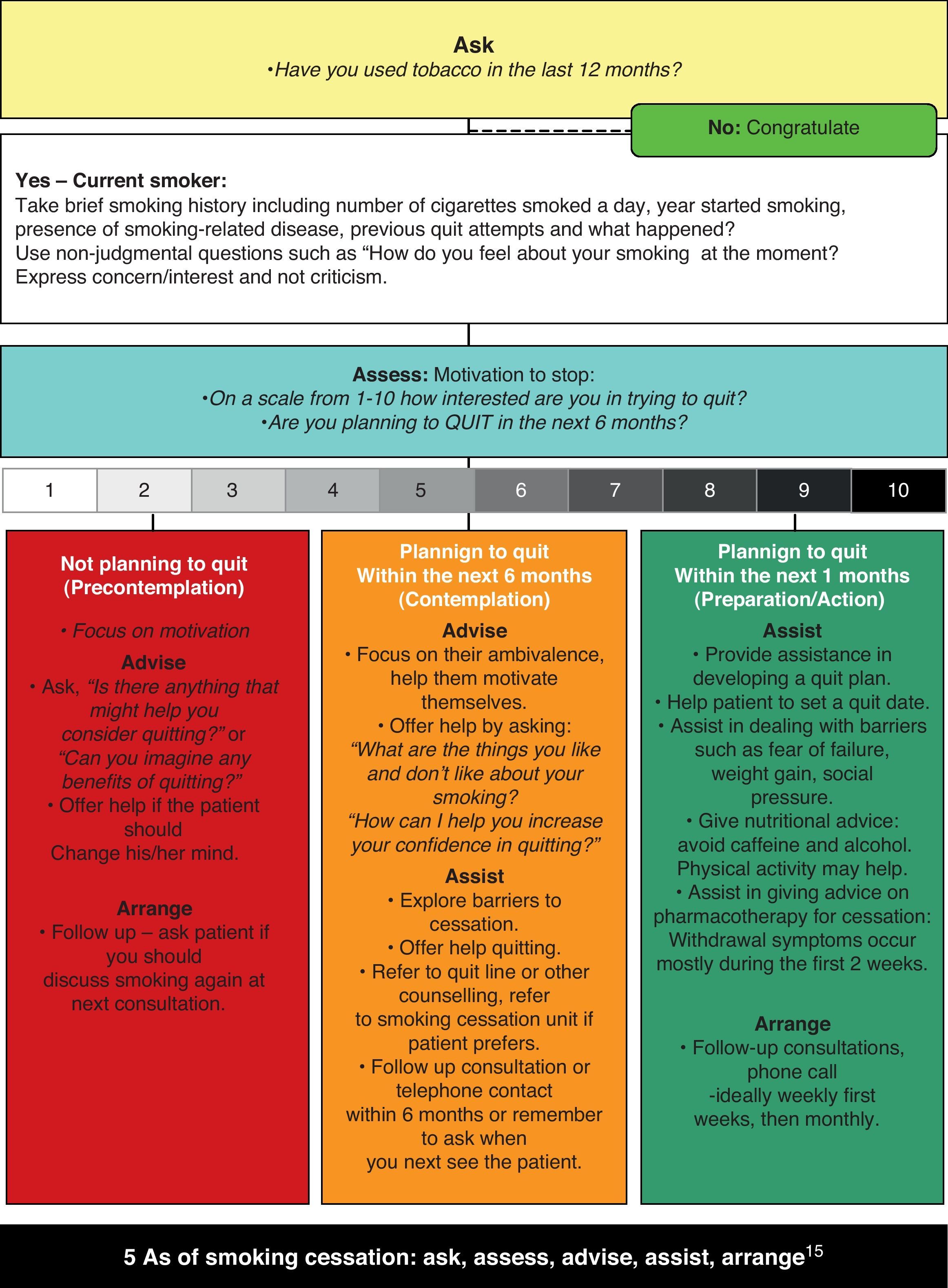
To help their patients quit smoking, clinicians can use the “five A's” approach15 (Fig. 1): ask patients about smoking, advise all smokers to quit, assess willingness to make a quit attempt, assist those who want to quit, and arrange follow-up visits with those trying to quit. Each intervention can be completed in less than 3min and has been associated with a cessation prevalence of 5–8%.13
A guide for assisting the smoker. The first step in treating tobacco use and dependence is to identify tobacco users. Asking systematically whether your patients smoke at every visit is imperative (ASK). All smokers should be advised to quit. This advice should be clearly stated and specifically adapted in relation to the patient's problems (ADVISE). The willingness of smokers to make a quit attempt at this time should be assessed (ASSESS). If the patient is ready to quit, health care providers should be prepared to offer assistance. This entails working together with the patient to set a sensible plan with a commitment to a quit date and to frequent follow-up visits. Alternatively, referring the patient to a tobacco intervention resource (eg, a smoking cessation quit line or health educator) that would deliver additional treatment to the patient might be contemplated (ASSIST). All patients who receive a tobacco dependence intervention should be regularly assessed for abstinence, beginning within the first week after the quit date. Abstinent patients should have their quitting success acknowledged.
There is a strong dose–response relation between the session length of person-to-person contact and successful treatment outcomes. Intensive interventions are more effective than less intensive interventions and should be used whenever possible. Person-to-person treatment delivered for four or more sessions appears especially effective in increasing abstinence rates.13
All patients with ILD should be routinely asked about their smoking status. This advice should be clearly stated and personalized. Clinicians treating smokers with ILD have an ideal “teachable moment” in that they are treating a disease that may have been caused or exacerbated by smoking and that can be ameliorated by quitting. It is important tell the patient that his disease is caused by or related to smoking and that can be ameliorated by quitting.13
After giving this advice, clinicians should assess whether smokers desire to quit at the present time.
For those smokers ambivalent about quitting, or less motivated, motivational interviewing appear to be effective in increasing a patient's likelihood of attempting to quit. Therefore, clinicians should use these techniques to encourage smokers who are ambivalent about quitting, or less motivated, to consider making an attempt.13
Clinicians should assist patients who want to quit. All clinicians and clinicians-in-training should be trained in effective strategies to assist tobacco users willing to make a quit attempt and to motivate those unwilling to quit.13
The clinician should work together with the patient to set a date to quit and should provide the patient with practical advice about how to quit and self-help materials. Clinicians should determine whether the patient is likely to require adjunctive help and whether the patient is a candidate for pharmacotherapy. Pharmacotherapy should be considered for all patients motivated to make a quit attempt, except in the presence of specific contraindications. The choice may take into account previous patient experience and preferences. Clinicians should also present other treatment options to their patients who want to quit. In particular, patients should be made aware of community cessation resources available.
Clinicians should arrange for a follow-up visit to discuss smoking cessation within two weeks of the chosen date to quit.13 Scheduling follow-up visits (or making follow-up telephone calls) improves cessation success. More intense interventions yield better outcomes. Outcomes are influenced by a host of structural factors, including session length, session frequency, total number of sessions, and number and types of treatment modalities.13
Smokers differ in their motivation to quit smoking, and these differences are thought to affect treatment prognosis. A theoretical structure for assessing these differences is offered by the model advanced by Prochaska and Di Clemente. Briefly, the model proposes that smokers go through a series of stages (not necessarily linearly) on the way to achieving prolonged abstinence from smoking (Fig. 1): not thinking seriously about quitting in the next six months, thinking seriously about quitting in the next six months, planning to quit in the next month, actually trying to quit, and trying to remain abstinent. If a relapse occurs, smokers should return to an earlier stage in the model.16
Helping smokers to overcome their addiction involves prompting quit attempts by offering help to all smokers without necessarily asking whether they are interested in quitting17 and clinicians should use the motivational interviewing on cessation to encourage all smokers to quit.13
Once established, cigarette smoking is a very difficult addiction to break. Smokers trying to quit have to simultaneously cope with psychological and pharmacological aspects of tobacco dependence. The pharmacological effects of nicotine play a crucial role in tobacco addiction and therefore pharmacotherapy is important to address this component of tobacco dependence in order to improve success rates. There is little doubt that currently marketed smoking cessation products (such as NRT, buproprion and varenicline) increase the chance of committed smokers stopping smoking, particularly when combined with counseling programs. This is because psychological therapies and counseling help smokers to cope with psychological aspects associated with tobacco dependence.
Unfortunately, many smokers relapse while receiving treatment for tobacco dependence. We acknowledge that this reflects the chronic relapsing nature of tobacco dependence and is not the fault of the physician, nor a failure of their patients, but more effective smoking cessation interventions are clearly needed.
Conflicts of interestR.C. and P.C. have no conflicts of interest or declarations towards the contents of this paper. R.P. has received lecture fees from Pfizer and GSK; he has also served as a consultant to Pfizer.