Human heartworm is a zoonotic disease caused by the parasite Dirofilaria spp., a helminth of the Nematoda class which was first reported in 1961 in a case of human pulmonary dirofilariasis (HPD).1
We report the case of a 38-year-old man, engineer, former smoker (4 pack-per-year) who presented to the emergency department with face edema. No pathological background. No animals at home.
Physical examination revealed a slight face edema. Except for eosinophilia (2000/uL) other routine tests were unremarkable and on chest X-ray a small peripheral solitary lung nodule on the right lung was visible.
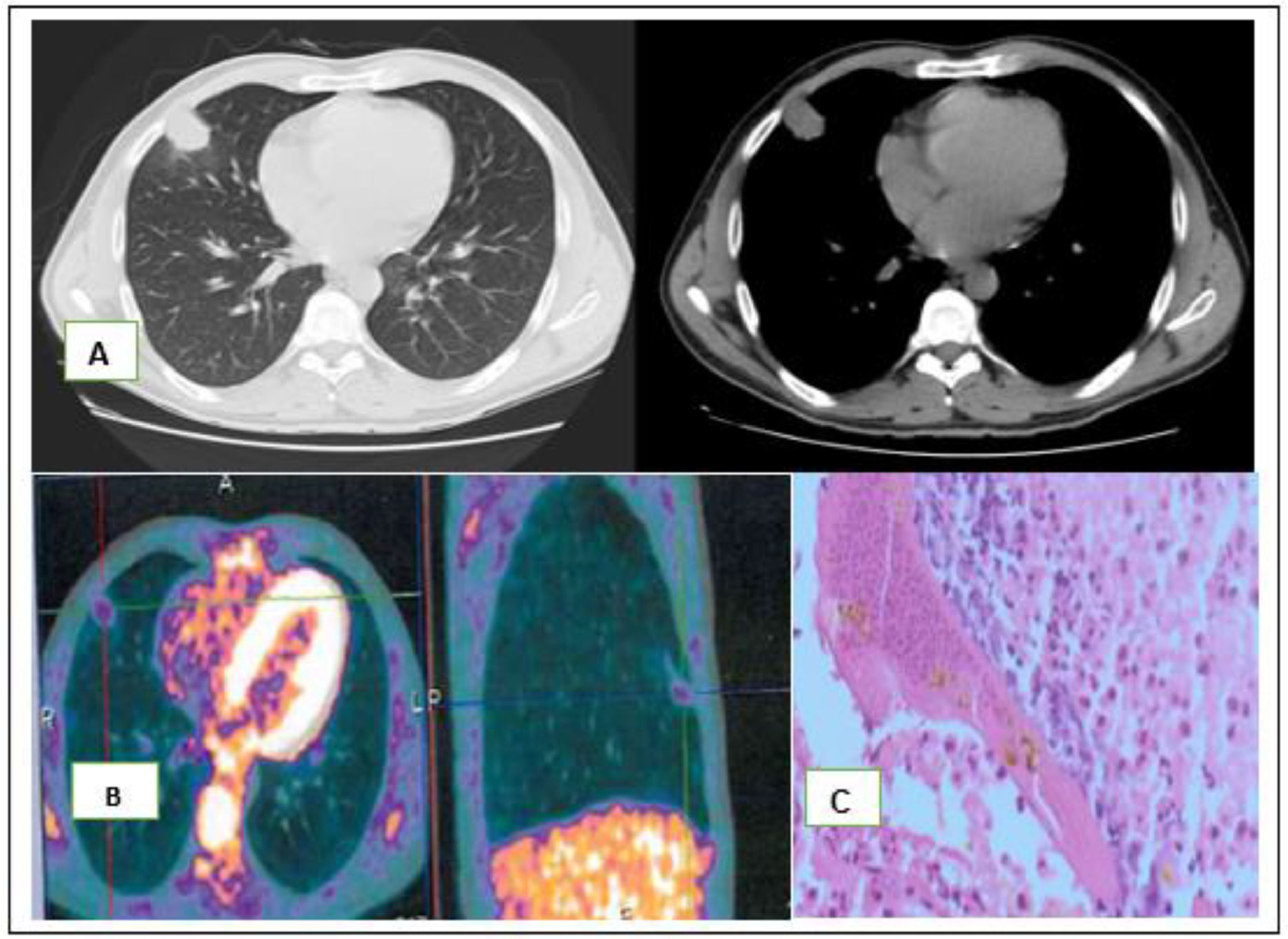
Chest computed tomography, demonstrated a 4 × 3 × 2,3 cm, irregular justa-pleural solid mass of the right middle lobe (Fig. 1-A). A CT-Guided transthoracic lung biopsy was performed but revealed extensive necrosis, histiocytes, lymphocytes and myofibroblasts suggestive of a benign, granulation-like tissue, few eosinophilic cells, Charcot Leyden crystals and was negative for malignancy. A 18F-FDG PET-CT showed low 18F-FDG uptake by the nodule with maximum standardized uptake (SUV) of 1.3 (Fig. 1-B). Since diagnosis could not be obtained from histological examination and malignancy could not be excluded, a video-assisted thoracoscopic surgery (VATS) with wedge resection was performed.
A- Chest computed tomography with an irregular justa-pleural mass. In the anatomical piece, a white well-delimited area was observed and when sliced a yellow justa-pleural nodule with increased consistency measuring 2,3 × 1,9 × 1,2 cm was identified; B- PET-CT with low 18F-FDG uptake (1.3); C- The intraoperative histopathological diagnosis was granuloma without malignant cells. Postoperative histopathological diagnosis was consistent with a central zone of necrosis surrounded by granulomatous inflammation and a fibrous wall. A worm was found in the lumen of an artery within the area of necrosis containing remnants of Dirofilaria immitis.
In the anatomical sample, a white well-delimited area was observed and when sliced a yellow nodule with increased consistency measuring 2,3 × 1,9 × 1,2 cm was identified. The intraoperative histopathological diagnosis was granuloma without malignant cells.
The postoperative histopathological diagnosis was consistent with a central zone of necrosis surrounded by granulomatous inflammation and a fibrous wall. A worm was found in the lumen of an artery within the area of necrosis containing remnants of Dirofilaria immitis (Fig. 1- C).
The final pathologic review of the resected lesions suggested a diagnosis of HPD.
Human pulmonary dirofilariasis is rare in Europe, with less than 40 cases reported. However, true incidence is limited since data is derived from isolated case reports.2
Dirofilaria is endemic in the Mediterranean region. Nevertheless distribution is changing due to environmental questions like temperature increase.3
Human dirofilariasis is transmitted by the bite of an infected mosquito from an infected dog or cat, which acts as a vector, and transmits Dirofilaria immitis larva to the skin.4
In accidental hosts, like humans the surviving larvae migrate to the small vessels of the pulmonary artery and generate vasculite, formation of granulomas and obstruction, inflammation and pulmonary infarction after death of parasite.2
Most cases reported are in middle-aged adults between 40 and 50 years of age.4
More than half of Dirofilaria infections patients are asymptomatic and symptomatic forms include fever, hemoptysis, dyspnea and chest pain.2
Systemic eosinophilia is relatively uncommon with 11–17% in most Japanese series.5
It usually presents as a solitary spherical, non-calcified, wedge-shaped, often spiculated or cavitated subpleural pulmonary nodule, ranging from 1 to 3 cm, with predilection to the right lower lobe of the lung.5
Serological studies have poor sensitivity (50%) in detecting antibodies because of cross reactivity with other nonfilarial parasites and their presence may only indicate exposure to larval antigens.6
Because there is no reliable noninvasive test for Dirofilaria infection, nearly all cases require biopsy to establish the diagnosis and permit treatment.6
In summary, the authors draw attention to this case for its extreme rarity.
The pathological analysis is fundamental in a case where the most frequent diagnostic hypotheses were ruled out by the other complementary diagnostic tests and where careful anamnesis continues to play a fundamental role.
Although considered a clinically benign disease, an excisional lung biopsy is nearly always needed for diagnosis and treatment and minimally invasive surgery with VATS should be performed whenever possible.
Conflicts of InterestThe authors have no conflicts of interest to declare.