Virtual Reality (VR) is a promising technology for implementing personalized, motivating and controlled rehabilitation scenarios. Although its clear potential benefits, VR has been poorly investigated in pulmonary rehabilitation. This review analyses the state of the art, by searching the scientific and grey literature, regarding the use of VR for the rehabilitation of patients with chronic obstructive pulmonary disease, providing a technological perspective. First, the main characteristics of the included systems are presented in terms of visualization devices, way of interaction and type of feedback they provide. Then, results of the selected studies are reported considering feasibility, safety, usability and user experience as outcomes. Finally, the main findings are discussed and future directions for research are outlined.
Chronic obstructive pulmonary disease (COPD) is a widespread chronic disease considered a leading cause of mortality and morbidity worldwide.1 It represents a substantial health and economic burden for both developed and low-income countries, with financial impact on national health care systems.2 Due to an impaired respiratory function, COPD leads to an umbrella of comorbidities: physical impairment, cognitive decline, social isolation and lower quality of life. Pulmonary Rehabilitation (PR) is an evidence-based non-pharmacological treatment, consisting of a comprehensive intervention performed by a multidisciplinary team3; it includes physical training, learning breathing techniques, psychological support and nutritional advice. Since the advent of new technologies, researchers have been working on different solutions to improve the rehabilitation process both from the clinical and the economic point of view.4 These include, for example, mobile applications for the self-management of COPD,5 tele-monitoring systems exploiting multiple sensors6 and digital environments for exercise training. Within these solutions, Virtual Reality (VR) represents a powerful tool for improving exercise training allowing personalized treatments, performance monitoring and quantitative measurement—also integrating sensors and external devices.7,8 Virtual Reality, by creating engaging scenarios may enable the “attentional shift”, distracting the patient from negative sensations (e.g. fatigue, breathlessness) during physical activity9; VR can be also effective in increasing motivation, by turning repetitive exercises—typical of the sometimes-boring conventional protocols—in engaging and enjoyable tasks.10 Moreover, VR helps to simulate realistic scenarios that would be otherwise challenging or impossible to reproduce in the real world, in a safe and controlled way. The possibility of providing contextualized tasks which stimulate the cognitive functions of the patients, fosters the transfer of skills acquired during the rehabilitation sessions to activities of daily living.11 In the context of COPD, VR is especially suitable for physical and breathing training. Physical training mainly includes endurance training, aimed to condition the muscles of ambulation and improve cardiorespiratory fitness, and strength training, in which local muscle groups are trained by repetitive movements performed with relatively heavy loads3; breathing training consists of different techniques (e.g. diaphragmatic breathing, pursed-lip breathing, inspiratory sighs) aimed at altering respiratory muscles recruitment and improving their performance thus decreasing breathlessness.12 Hereafter we will consider these components of the intervention when referring to PR. Although it has been extensively used successfully in the treatment of different groups of patients e.g. post-stroke,13 patients with Mild Cognitive Impairment,14 frail elderly,15 children with neuromotor deficits,16 the application of VR to rehabilitation of COPD is still not fully explored. An example of a VR system for physical training is shown in Fig. 1. The aim of this work is to analyse the current state of the art in this topic, focusing on technical aspects and on the user’s perception of technology.
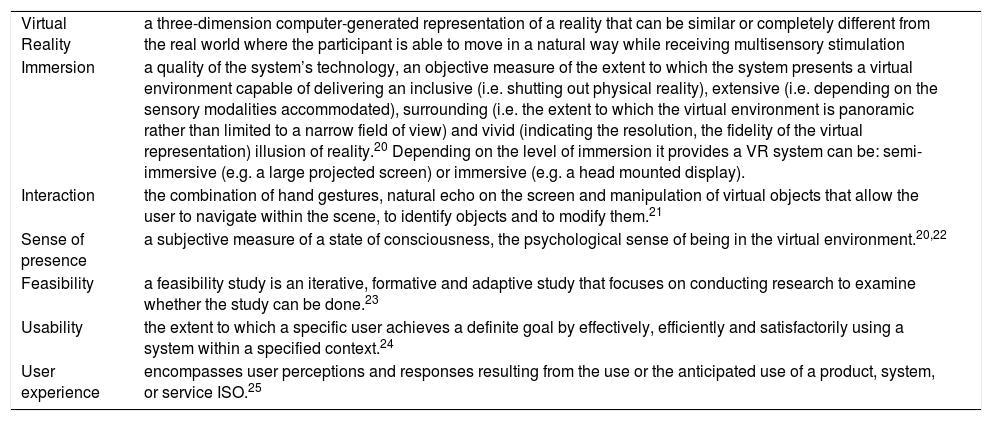
With respect to the analysis of the technical aspects, we need to clarify the term “Virtual Reality”, which researchers often use when referring to any computer-based device that provides visual and audio stimuli, e.g. videogames, on a monitor.17 However, in VR, the user, surrounded by a 3D computer-generated representation, is “transported” into the virtual environment (VE), should be able to move in it and to interact with the virtual objects in a natural way as he/she is part of the scene.18 In fact, two key factors that characterize a VR system are immersion and interaction. These elements, as described in Table 1, influence the sense of presence, which in turn affects the effectiveness of the VR experience, e.g. the training.19
Definitions.
| Virtual Reality | a three-dimension computer-generated representation of a reality that can be similar or completely different from the real world where the participant is able to move in a natural way while receiving multisensory stimulation |
| Immersion | a quality of the system’s technology, an objective measure of the extent to which the system presents a virtual environment capable of delivering an inclusive (i.e. shutting out physical reality), extensive (i.e. depending on the sensory modalities accommodated), surrounding (i.e. the extent to which the virtual environment is panoramic rather than limited to a narrow field of view) and vivid (indicating the resolution, the fidelity of the virtual representation) illusion of reality.20 Depending on the level of immersion it provides a VR system can be: semi-immersive (e.g. a large projected screen) or immersive (e.g. a head mounted display). |
| Interaction | the combination of hand gestures, natural echo on the screen and manipulation of virtual objects that allow the user to navigate within the scene, to identify objects and to modify them.21 |
| Sense of presence | a subjective measure of a state of consciousness, the psychological sense of being in the virtual environment.20,22 |
| Feasibility | a feasibility study is an iterative, formative and adaptive study that focuses on conducting research to examine whether the study can be done.23 |
| Usability | the extent to which a specific user achieves a definite goal by effectively, efficiently and satisfactorily using a system within a specified context.24 |
| User experience | encompasses user perceptions and responses resulting from the use or the anticipated use of a product, system, or service ISO.25 |
All these technical aspects contribute to the realism of the experience, the satisfaction of the user and, consequently, to the effectiveness of the rehabilitation intervention. In addition, when considering a system for rehabilitation two essential requirements are feasibility and safety, which should be evaluated in the context of use. A third factor that should be considered is usability, which should always be high for any kind of technology. Moreover, the overall user experience should be positive and engaging and, therefore, investigating different aspects such as enjoyment, interest, and acceptability is crucial for creating solutions that are well perceived by the patients. Digital solutions, including VR, should induce a positive user experience in patients because “if the users feel like the technology does not match their needs and preferences, or cannot be embedded in their routines, it will not be used”.26 For all these reasons, it is important to consider these aspects both when designing and when evaluating a VR system for rehabilitation.
To the best of our knowledge, this work represents the first analysis providing a technological perspective on VR for PR. However, the increasing interest in understanding whether and how such technology could be effectively applied in this field is demonstrated by four reviews published between February 2019 and May 2020.27–30 All the four reviews focus mainly on the clinical effectiveness of videogames for patients with respiratory diseases. Three of them analyse exergames (i.e. exercise+videogame) for physical training, while Sanchez and colleagues include also studies providing educational intervention.29 We will include in our analysis only the systems for physical and breathing training since these are the elements of PR that may benefit the most from an interactive multi-stimuli training environment, like the one provided by VR. Simmich and colleagues examine the effectiveness of game-based interventions vs. traditional protocols on physiological outcome measures, adherence and enjoyment in subjects with chronic respiratory diseases.28 All respiratory conditions are admitted including asthma, thus widening the target population to children. Since age is a key factor in the perception and adoption of technology, our review will focus only on elderly patients. Similarly, Wang and colleagues published a systematic review including controlled trials but limiting the analysis to COPD patients.30 Based on the seven papers they have analysed, the authors conclude that exergames, in particular active video games (AVGs), are useful and enjoyable as an adjunct to PR. The review by Butler et al. presents controlled studies involving different chronic diseases and considers exercise capacity as the primary outcome; secondary outcomes are dyspnoea, fatigue, energy expenditure as well as enjoyment and user preference.27 The analysis by Sanchez et al. also covers not only COPD but also chronic bronchitis, emphysema, asbestosis, asthma, cystic fibrosis and bronchiectasis.29 Like the other reviews, the analysis is focused on clinical outcomes (e.g. respiratory function, exercise capacity, symptoms, quality of life); knowledge of the disease is also considered with respect to educational interventions.
All the reviews mentioned share a clinical perspective, focusing on the comparison of physiological response and clinical outcomes with a control group. Instead, the present work provides a technological point of view through the analysis of the characteristics of the proposed systems in terms of technology and user experience. The aim of our work is thus to analyse the state-of-the-art-technology and to identify gaps in the existing literature regarding the application of VR to respiratory rehabilitation—and in particular training exercise (physical and breathing).
MethodsSince our analysis focuses on the technological aspects rather than on clinical effectiveness, a scoping review has been preferred. Such a methodology allows inclusion of not only the scientific but also the grey literature, which in this case may present preliminary works not yet eligible for full publication process. We observed the recommendations on scoping studies by Arskey & O’Malley31 to guarantee the application of a rigorous protocol.
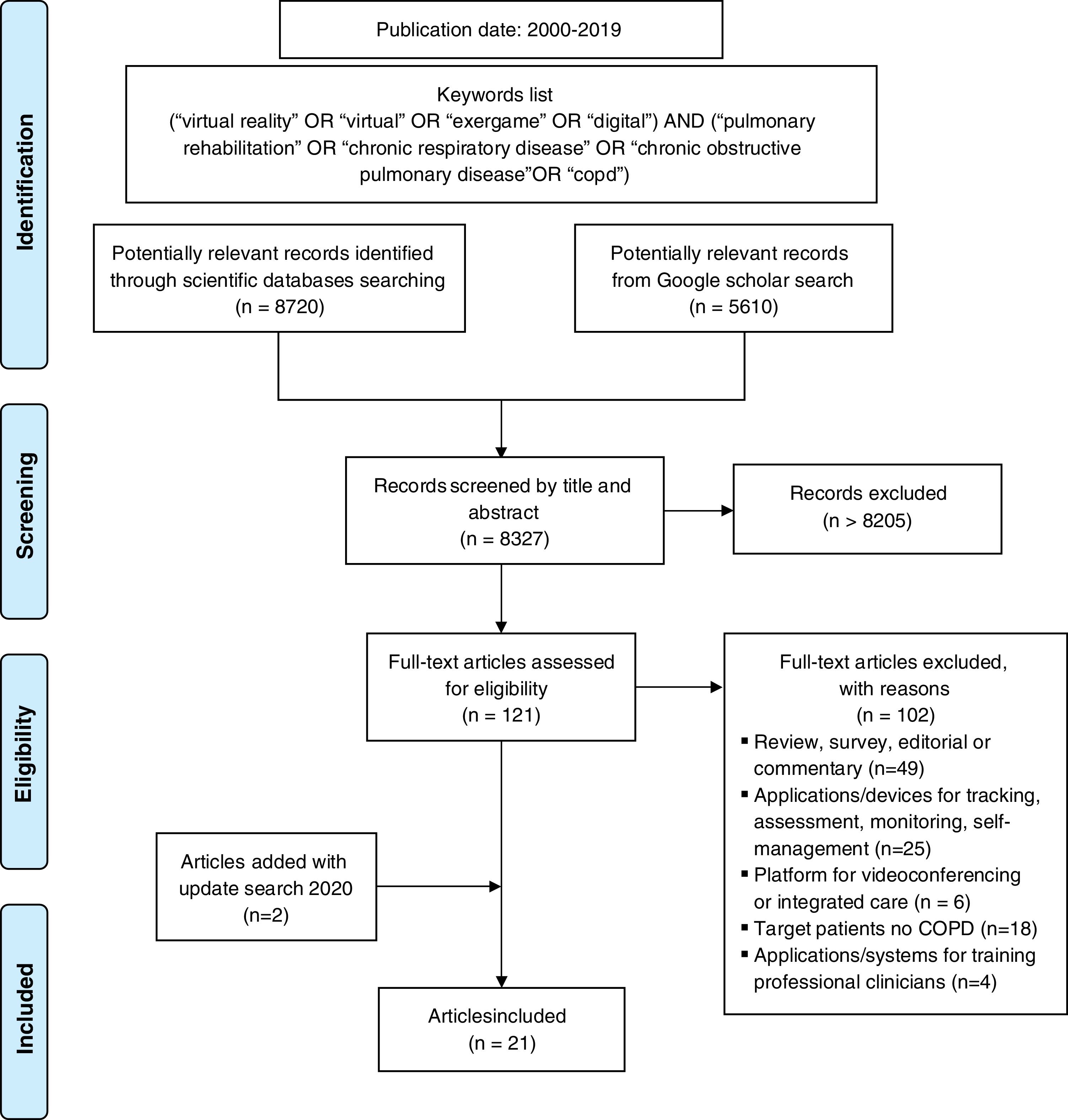
Literature search and study selectionA literature search was carried out between September 2019 and November 2019; an update was carried out on October 31st 2020 in the following scientific databases: MEDLINE, IEEExplore, Scopus (EMBASE). Grey literature was analysed through Google Scholar. The search was restricted to year 2000 in the past because VR technology—in terms of both hardware and software—has significantly improved starting from 1999.32
The authors searched the databases and selected the systems that met the following inclusion criteria.
- •
The system is designed for pre-elderly (between 50–65 y. old) or elderly (>over 65 y. old); main target users are COPD patients;
- •
It provides physical or breathing training;
- •
It is a digital solution, VR application or exergame/active videogame providing a virtual scenario and (at least) visual and/or audio stimuli, active interaction and feedback.
Mobile apps for self-management and apps for rehabilitation—e.g. based on written or video instructions—not providing an interactive virtual scenario were excluded as considered out of the scope of our analysis.
Data extraction and analysisThe following information was retrieved for each of the articles,: year and type of publication, type of training, technology used, interaction device, visualization device, the presence and the type of physiological sensors integrated in the system.
ResultsThe study selection process and keywords are reported in Fig. 2. As a result, 21 articles, published between 2011 and 2020, were included in the analysis. As a scoping review, all types of publications have been admitted: 10 journal papers, 5 conference proceedings papers, 5 abstracts and a book chapter.
Training systems characteristicsThe literature search focused on systems designed for physical and/or breathing training. Most of the systems (73%) are designed for physical exercise; around 16% provides breathing exercises only and 21% allows for both training modalities.
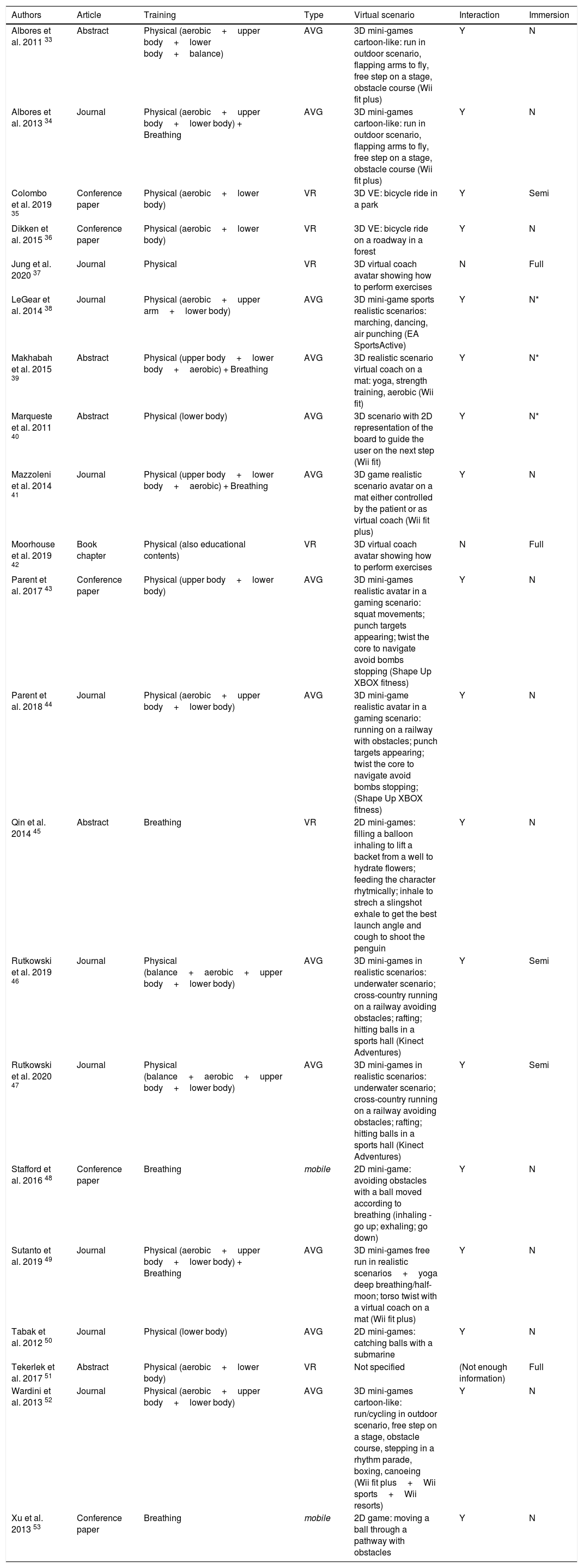
Most of the studies (68%) use active video games (AVGs) as a training tool for both physical and breathing exercises. Active video games, usually experienced through a PC/TV monitor or a mobile device screen, fall into the exergames category. Exergames, coupling physical activity and videogames, show some of the features of VR, e.g. gamification, even if they are characterized by lower naturalistic sensory-motor interaction, limited ecological validity and lower degree of immersion. Regarding the reviewed studies, AVGs are based on consumer devices and, in particular, on Microsoft Kinect for XBOX, Nintendo Wii fit—either with or without the Balance Board. Six systems out of 21 are considered VR systems (see Introduction). Two studies provide training feedback and guidance through mobile applications. The main characteristics of the identified systems are summarised in Table 2.
Main characteristics of the training systems (AVG=Active Video Game, VR=Virtual Reality, Y=yes, N=no, Semi=semi-immersive, Full=immersive, N*=not specified but likely not).
| Authors | Article | Training | Type | Virtual scenario | Interaction | Immersion |
|---|---|---|---|---|---|---|
| Albores et al. 2011 33 | Abstract | Physical (aerobic+upper body+lower body+balance) | AVG | 3D mini-games cartoon-like: run in outdoor scenario, flapping arms to fly, free step on a stage, obstacle course (Wii fit plus) | Y | N |
| Albores et al. 2013 34 | Journal | Physical (aerobic+upper body+lower body) + Breathing | AVG | 3D mini-games cartoon-like: run in outdoor scenario, flapping arms to fly, free step on a stage, obstacle course (Wii fit plus) | Y | N |
| Colombo et al. 2019 35 | Conference paper | Physical (aerobic+lower body) | VR | 3D VE: bicycle ride in a park | Y | Semi |
| Dikken et al. 2015 36 | Conference paper | Physical (aerobic+lower body) | VR | 3D VE: bicycle ride on a roadway in a forest | Y | N |
| Jung et al. 2020 37 | Journal | Physical | VR | 3D virtual coach avatar showing how to perform exercises | N | Full |
| LeGear et al. 2014 38 | Journal | Physical (aerobic+upper arm+lower body) | AVG | 3D mini-game sports realistic scenarios: marching, dancing, air punching (EA SportsActive) | Y | N* |
| Makhabah et al. 2015 39 | Abstract | Physical (upper body+lower body+aerobic) + Breathing | AVG | 3D realistic scenario virtual coach on a mat: yoga, strength training, aerobic (Wii fit) | Y | N* |
| Marqueste et al. 2011 40 | Abstract | Physical (lower body) | AVG | 3D scenario with 2D representation of the board to guide the user on the next step (Wii fit) | Y | N* |
| Mazzoleni et al. 2014 41 | Journal | Physical (upper body+lower body+aerobic) + Breathing | AVG | 3D game realistic scenario avatar on a mat either controlled by the patient or as virtual coach (Wii fit plus) | Y | N |
| Moorhouse et al. 2019 42 | Book chapter | Physical (also educational contents) | VR | 3D virtual coach avatar showing how to perform exercises | N | Full |
| Parent et al. 2017 43 | Conference paper | Physical (upper body+lower body) | AVG | 3D mini-games realistic avatar in a gaming scenario: squat movements; punch targets appearing; twist the core to navigate avoid bombs stopping (Shape Up XBOX fitness) | Y | N |
| Parent et al. 2018 44 | Journal | Physical (aerobic+upper body+lower body) | AVG | 3D mini-game realistic avatar in a gaming scenario: running on a railway with obstacles; punch targets appearing; twist the core to navigate avoid bombs stopping; (Shape Up XBOX fitness) | Y | N |
| Qin et al. 2014 45 | Abstract | Breathing | VR | 2D mini-games: filling a balloon inhaling to lift a backet from a well to hydrate flowers; feeding the character rhytmically; inhale to strech a slingshot exhale to get the best launch angle and cough to shoot the penguin | Y | N |
| Rutkowski et al. 2019 46 | Journal | Physical (balance+aerobic+upper body+lower body) | AVG | 3D mini-games in realistic scenarios: underwater scenario; cross-country running on a railway avoiding obstacles; rafting; hitting balls in a sports hall (Kinect Adventures) | Y | Semi |
| Rutkowski et al. 2020 47 | Journal | Physical (balance+aerobic+upper body+lower body) | AVG | 3D mini-games in realistic scenarios: underwater scenario; cross-country running on a railway avoiding obstacles; rafting; hitting balls in a sports hall (Kinect Adventures) | Y | Semi |
| Stafford et al. 2016 48 | Conference paper | Breathing | mobile | 2D mini-game: avoiding obstacles with a ball moved according to breathing (inhaling - go up; exhaling; go down) | Y | N |
| Sutanto et al. 2019 49 | Journal | Physical (aerobic+upper body+lower body) + Breathing | AVG | 3D mini-games free run in realistic scenarios+yoga deep breathing/half-moon; torso twist with a virtual coach on a mat (Wii fit plus) | Y | N |
| Tabak et al. 2012 50 | Journal | Physical (lower body) | AVG | 2D mini-games: catching balls with a submarine | Y | N |
| Tekerlek et al. 2017 51 | Abstract | Physical (aerobic+lower body) | VR | Not specified | (Not enough information) | Full |
| Wardini et al. 2013 52 | Journal | Physical (aerobic+upper body+lower body) | AVG | 3D mini-games cartoon-like: run/cycling in outdoor scenario, free step on a stage, obstacle course, stepping in a rhythm parade, boxing, canoeing (Wii fit plus+Wii sports+Wii resorts) | Y | N |
| Xu et al. 2013 53 | Conference paper | Breathing | mobile | 2D game: moving a ball through a pathway with obstacles | Y | N |
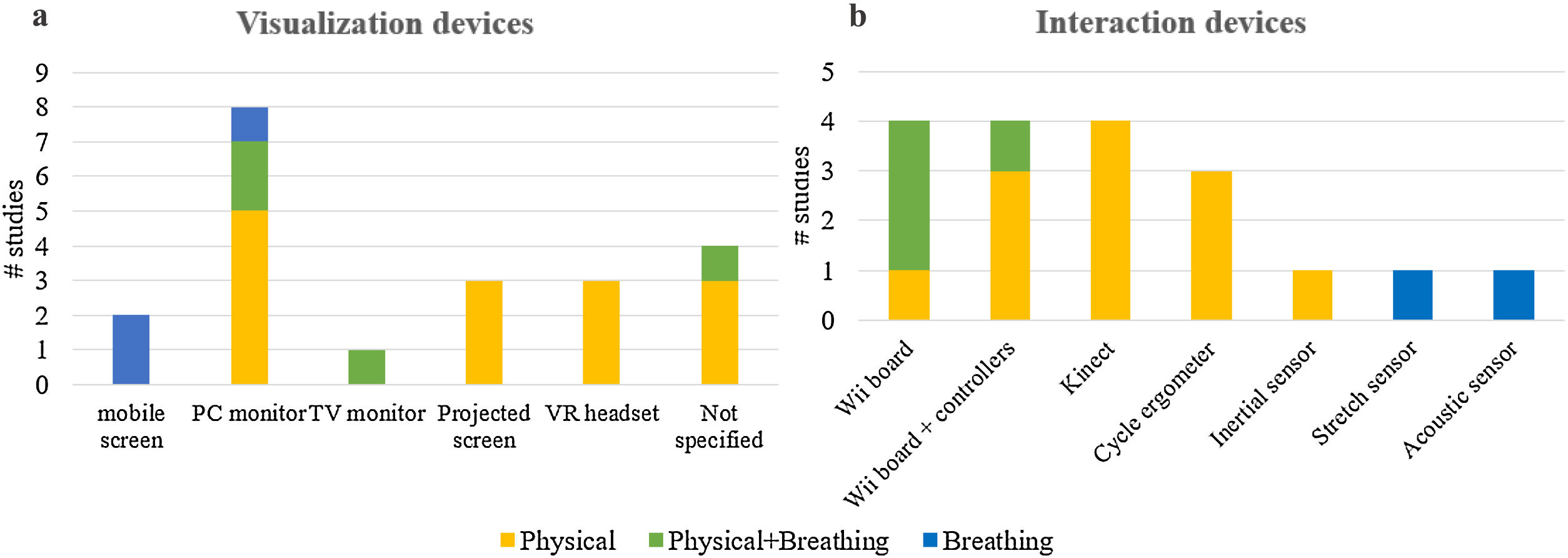
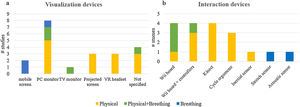
Different types of devices were used (see Fig. 3—Panel a) to display virtual contents to the user, each characterized by specific field of view (FOV), dimension and providing a given level of immersion. Most of the systems identified used a flat screen of small to medium dimensions and limited FOV providing no immersion: a PC monitor (n=8), a TV (n=1), a tablet/smartphone display (n=2). In 4 cases, the authors did not explicitly specify the type of visualization device, however, based on the described systems, it is very likely that a PC/TV monitor was used.38–40,52 Wider screens with a greater FOV were used in 3 studies in the form of a large projected screen.35,46,47 In this case, the VE covers a large part of the FOV thus allowing the viewer to be partly immersed in the virtual scenario (semi-immersive). Only 3 studies used a head mounted display (HMD), characterized by higher FOV providing a fully immersive experience.37,42,51
Interaction and exercise feedbackTo allow the user interact with the virtual contents, the analysed systems use different devices as shown in Fig. 3—Panel b. Most systems (n=8) are based on the Nintendo Wii fit consisting of the Balance Board—a board embedded with weight sensors placed at the four corners detecting the weight displacement over it—and one or two controllers—usually held in the hands and measuring the hands’ displacement through an accelerometer. The user interacts with the VE either moving on the Balance Board (e.g. stepping or swinging) or through the movements of the arms detected by controllers. Four of the included studies used the Microsoft XBOX Kinect, which features an RGB camera, a depth sensor and a microphone array.43,44,46,47 It can track the whole body and compute position and orientation of each joint of the skeleton. The user’s body movement is usually mapped to the human-like body skeleton of a virtual avatar. Those systems providing cycling training (n=3) used a cycle-ergometer with sensors for measuring the cycling speed, which controls the navigation in the VE.35,36,51 The solution presented by Tabak et al. consists of an accelerometer attached to the patient’s hip detecting the vertical displacement during the squat movement.50 The systems for breathing training employed either acoustic sensors48,53 (i.e. a microphone placed at the mouth of the user) or a stretch sensor45,48 (i.e. a chest elastic band) to measure the respiratory signal, through which the user controls specific virtual objects.
In most cases (n=10), feedback on the performance is provided to the patient through a human-like virtual avatar, controlled by the user’s movement, in third-person perspective. In two of the cycling systems, the user navigates the environment in first-person perspective, as if he/she is riding a virtual bicycle.35,36 In all systems for physical training, the patient receives visual and audio feedback on correct movements and remaining time/time passing. In the studies using commercial AVGs, correct movements are often represented by the increase of the total score. When an aerobic task is foreseen—e.g. cycling or jogging in place—also real-time physical parameters, such as cycling speed or distance travelled, are shown to the patient. Few systems include physiological parameters as feedback during the exercise: three of them show heart rate and oxygen saturation level to either the patient or the physiotherapist only35,42,50; one of the AVGs reports energy expenditure.38
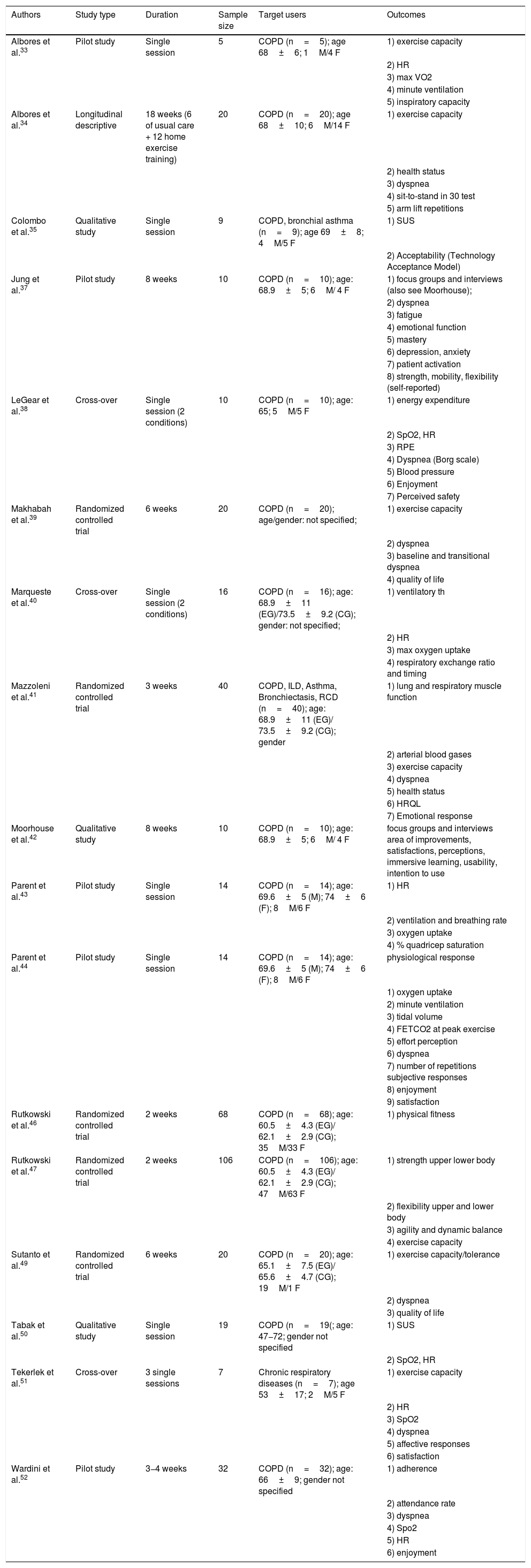
Study resultsSeventeen papers—the characteristics of which are summarised in Table 3—present a clinical study involving COPD patients. Among these, 5 randomized controlled trials compared the outcomes of a group of patients training in VR with those assessed in patients undergoing traditional rehabilitation. Assessments were performed before and after the rehabilitation period, which lasted from 2 to 8 weeks, corresponding to the typical duration of PR. Five pilot studies and one longitudinal descriptive study present results of a VR-based physical training program on COPD patients. Three qualitative studies focused on the user experience investigating patients’ attitude towards the use of technology for rehabilitation. Participants of all studies are adults, most of them are elderly: average age is over 65 for 10 out of 17 studies; two studies do not provide details on participants’ age.39,40
Characteristics of the included studies (M=male, F=female, CG=control group, EG=experimental group, HR=heart rate,VO2 max=maximum rate of oxygen consumption, SpO2=oxygen saturation, RPE=rate of perceived exertion, FETCO2=end-tidal fractional concentrations of CO2, HRQL=health-related quality of life, SUS=system usability scale).
| Authors | Study type | Duration | Sample size | Target users | Outcomes |
|---|---|---|---|---|---|
| Albores et al.33 | Pilot study | Single session | 5 | COPD (n=5); age 68±6; 1M/4 F | 1) exercise capacity |
| 2) HR | |||||
| 3) max VO2 | |||||
| 4) minute ventilation | |||||
| 5) inspiratory capacity | |||||
| Albores et al.34 | Longitudinal descriptive | 18 weeks (6 of usual care + 12 home exercise training) | 20 | COPD (n=20); age 68±10; 6M/14 F | 1) exercise capacity |
| 2) health status | |||||
| 3) dyspnea | |||||
| 4) sit-to-stand in 30 test | |||||
| 5) arm lift repetitions | |||||
| Colombo et al.35 | Qualitative study | Single session | 9 | COPD, bronchial asthma (n=9); age 69±8; 4M/5 F | 1) SUS |
| 2) Acceptability (Technology Acceptance Model) | |||||
| Jung et al.37 | Pilot study | 8 weeks | 10 | COPD (n=10); age: 68.9±5; 6M/ 4 F | 1) focus groups and interviews (also see Moorhouse); |
| 2) dyspnea | |||||
| 3) fatigue | |||||
| 4) emotional function | |||||
| 5) mastery | |||||
| 6) depression, anxiety | |||||
| 7) patient activation | |||||
| 8) strength, mobility, flexibility (self-reported) | |||||
| LeGear et al.38 | Cross-over | Single session (2 conditions) | 10 | COPD (n=10); age: 65; 5M/5 F | 1) energy expenditure |
| 2) SpO2, HR | |||||
| 3) RPE | |||||
| 4) Dyspnea (Borg scale) | |||||
| 5) Blood pressure | |||||
| 6) Enjoyment | |||||
| 7) Perceived safety | |||||
| Makhabah et al.39 | Randomized controlled trial | 6 weeks | 20 | COPD (n=20); age/gender: not specified; | 1) exercise capacity |
| 2) dyspnea | |||||
| 3) baseline and transitional dyspnea | |||||
| 4) quality of life | |||||
| Marqueste et al.40 | Cross-over | Single session (2 conditions) | 16 | COPD (n=16); age: 68.9±11 (EG)/73.5±9.2 (CG); gender: not specified; | 1) ventilatory th |
| 2) HR | |||||
| 3) max oxygen uptake | |||||
| 4) respiratory exchange ratio and timing | |||||
| Mazzoleni et al.41 | Randomized controlled trial | 3 weeks | 40 | COPD, ILD, Asthma, Bronchiectasis, RCD (n=40); age: 68.9±11 (EG)/ 73.5±9.2 (CG); gender | 1) lung and respiratory muscle function |
| 2) arterial blood gases | |||||
| 3) exercise capacity | |||||
| 4) dyspnea | |||||
| 5) health status | |||||
| 6) HRQL | |||||
| 7) Emotional response | |||||
| Moorhouse et al.42 | Qualitative study | 8 weeks | 10 | COPD (n=10); age: 68.9±5; 6M/ 4 F | focus groups and interviews area of improvements, satisfactions, perceptions, immersive learning, usability, intention to use |
| Parent et al.43 | Pilot study | Single session | 14 | COPD (n=14); age: 69.6±5 (M); 74±6 (F); 8M/6 F | 1) HR |
| 2) ventilation and breathing rate | |||||
| 3) oxygen uptake | |||||
| 4) % quadricep saturation | |||||
| Parent et al.44 | Pilot study | Single session | 14 | COPD (n=14); age: 69.6±5 (M); 74±6 (F); 8M/6 F | physiological response |
| 1) oxygen uptake | |||||
| 2) minute ventilation | |||||
| 3) tidal volume | |||||
| 4) FETCO2 at peak exercise | |||||
| 5) effort perception | |||||
| 6) dyspnea | |||||
| 7) number of repetitions subjective responses | |||||
| 8) enjoyment | |||||
| 9) satisfaction | |||||
| Rutkowski et al.46 | Randomized controlled trial | 2 weeks | 68 | COPD (n=68); age: 60.5±4.3 (EG)/ 62.1±2.9 (CG); 35M/33 F | 1) physical fitness |
| Rutkowski et al.47 | Randomized controlled trial | 2 weeks | 106 | COPD (n=106); age: 60.5±4.3 (EG)/ 62.1±2.9 (CG); 47M/63 F | 1) strength upper lower body |
| 2) flexibility upper and lower body | |||||
| 3) agility and dynamic balance | |||||
| 4) exercise capacity | |||||
| Sutanto et al.49 | Randomized controlled trial | 6 weeks | 20 | COPD (n=20); age: 65.1±7.5 (EG)/ 65.6±4.7 (CG); 19M/1 F | 1) exercise capacity/tolerance |
| 2) dyspnea | |||||
| 3) quality of life | |||||
| Tabak et al.50 | Qualitative study | Single session | 19 | COPD (n=19(; age: 47−72; gender not specified | 1) SUS |
| 2) SpO2, HR | |||||
| Tekerlek et al.51 | Cross-over | 3 single sessions | 7 | Chronic respiratory diseases (n=7); age 53±17; 2M/5 F | 1) exercise capacity |
| 2) HR | |||||
| 3) SpO2 | |||||
| 4) dyspnea | |||||
| 5) affective responses | |||||
| 6) satisfaction | |||||
| Wardini et al.52 | Pilot study | 3−4 weeks | 32 | COPD (n=32); age: 66±9; gender not specified | 1) adherence |
| 2) attendance rate | |||||
| 3) dyspnea | |||||
| 4) Spo2 | |||||
| 5) HR | |||||
| 6) enjoyment |
The study results are presented hereinafter focusing on the aspects of interest of our analysis: feasibility, safety, usability and user experience.
Feasibility and safetyThe included studies demonstrate that using VR solutions for training is feasible for patients with COPD. Albores and colleagues designed an intervention based on 6 Nintendo Wii exergames involving upper and lower limbs.33 Results in a small group of patients demonstrated the feasibility of such intervention, which elicits a level of exercise intensity similar to that recommended by standard protocols. The Nintendo Wii system has also been proven safe and feasible as an additional tool to traditional protocols with a group of 32 elderly training for 3−4 weeks.52 In a more recent study by Albores and colleagues, the same intervention proved safe and feasible in an unsupervised scenario with patients training independently at home for 12 weeks with no adverse effects.34 The same system was also used by LeGear and colleagues in a cross-over trial with 10 patients performing a single session of training including marching, dancing and two air punching exercises.38 An education session with therapists explaining and demonstrating the exergames was performed prior to the training. All participants found the intervention enjoyable and safe; they all felt comfortable with the possibility of performing the exercises at home without supervision. Relatives and colleagues evaluated the feasibility of a training program based on high intensity AVGs by Microsoft Kinect XBOX.44 In this study, the original descriptions of some tasks, provided by the manufacturer, have been adapted to match the patients’ requirements better, e.g. “Squat as much as you can” has been modified to “Sit and stand on chair”. Although most participants enjoyed the intervention and expressed their willingness to have the system at home, not all of them felt sufficiently confident about using it by themselves. More clear instructions and reminders (e.g. using pictures) should be added to ease the interaction especially for those patients who have little experience with technology. Moreover, monitoring the physiological response is considered crucial for both clinicians and patients to ensure safety in home-based setting. In most of the cases, safety was assured by the presence of a therapist, monitoring the vital signs and symptoms (e.g. heart rate, SpO2, fatigue) during the whole exercise session using external devices, as used in the standard practice. These include pulse oximeters,38,41 respiratory monitor,41 heart rate sensors,47 activity monitor to measure energy expenditure38 and a portable metabolic analyzer.44 In a few cases, these measurements were integrated in the application receiving data from a heart rate band and a pulse-oximeter,36 a finger clip50 and a wrist worn pulse-oximeter.35,37
Usability and user experienceThree studies evaluated the usability, either through a standard tool (i.e. the System Usability Scale – SUS) or through one-to-one interviews. For both the cases in which the SUS was used, the usability was excellent.35,50 In both cases, however, the interaction between the user and the virtual contents was quite simple, representing a limitation to the positive results. In the system by Colombo et al. the user navigates the VE by simply cycling on the real ergometer35; in Tabak et al., the user controls the exercise—i.e. moving a submarine to collect bubbles—through his/her movements acquired by an accelerometer attached to the hip.50 When a higher level of interaction was required, i.e. using a VR headset for performing exercises, the patients found the system fairly easy to use even if some technical aspects could be improved (e.g. “adding the possibility to pause the system easily”) to make the interaction easier.37,42
Two studies explicitly include the evaluation of acceptability, assessed through ad-hoc questionnaires and spontaneous comments by the users. Colombo et al. focused attention on four variables: intention to use, perceived ease of use, perceived usefulness and subjective norm, which represents the perceived social pressure to engage or not to engage in a specific behaviour (here adhering to the treatment).35 Mazzoleni et al. evaluate the acceptability of a Nintendo Wii program in a group of patients undergoing 3-week rehabilitation addressing the following items: “comfort”, “absence of pain”, “fatigue”, “enjoyment”, “advantages”, “desire to continue” and “suggest to anyone”. In both studies, the acceptability was high.41 Even if a direct comparison cannot be made due to different methodology, both results suggest that patients show positive attitudes towards the use of technology for performing physical exercise. It is worth mentioning that both protocols foresaw the presence of a physiotherapist supervising the situation.
Tekerlek compared cycling on a stationary bike in three conditions: no feedback, music and VR. Patients reported low satisfaction—assessed through a 10-cm Visual Analog Scale—when in the VR condition mainly due to characteristics of the headset (weight, induced over sweating); they found the virtual content (video) repetitive and boring.51 A little discomfort with the use of an HMD has been reported in the study presented by Moorhouse et al. and Jung et al.37,42 Even if patients found the interaction quite easy to use, some of them complained about the weight of the device. The authors also performed focus groups and one-to-one interviews with participants to investigate all aspects of the VR training, which was divided into modules of increasing difficulty. A few patients found some modules too easy; a more personalized solution would make the VR experience more challenging and attractive. Nevertheless, all participants were satisfied with the training program; they reported a sense of satisfaction and increased motivation when successfully achieving a new training goal, e.g. completing a level of difficulty. Moreover, knowing that their usage and data were being tracked by health practitioners represented a strong motivator to adhere to the treatment. These qualitative results were supported by quantitative self-reported data presented in Jung et al. demonstrating improvements also in anxiety disorders, self-confidence and perceived physical strength and mobility.37
In general, all studies reported that patients enjoy training with technology finding the virtual contents fun and motivating either at home or as part of the rehabilitation program in the hospital.35,44,50,52
DiscussionAlthough the application of VR to PR is still developing, our review supports its feasibility, and its potential effectiveness to improve patients’ motivation and engagement thus maintaining the benefits of rehabilitation over a longer period of time.
The papers included in our analysis are mainly focused on physical training; some are about teaching breathing techniques while few others combine breathing and physical exercise. This is in line with the standard practice for PR, which foresees physical training as cornerstone. The effects of breathing exercises on dyspnoea and overall patient’s health condition is, instead, variable so that their role in the comprehensive management of COPD is not as widespread as physical activity.12 Even if physical activity seems to also improv cognitive functions and the use of VR itself is able to stimulate cognitive functions even without specific tasks, more research should focus on investigating the effect of integrating specific cognitive training in PR programs.14,54 In fact, no studies providing cognitive training have been identified even if the literature suggests that, also due to the typical age of COPD patients, cognitive decline impacts on their quality of life.55
Most of the available studies employed AVGs, based on consumer devices, adapting the level of difficulty to the patients’ needs. As a result, most of the proposed solutions did not follow a user-centred design approach; AVGs have a wider and more heterogenous audience. Patients with COPD have specific needs and are in a vulnerable condition so that additional safety concerns should be considered (e.g. assuring that the intensity of the exercise is adequate through real-time monitoring). However, commercial exergames, which undergo product testing based on standards for quality, guarantee functional safety and reliability. Moreover, they provide attractive graphics and audio feedback. On the other hand, for prototypes, only basic functional testing is performed while no functional safety standards are applicable because the development efforts would exceed the scope of a prototype build-up. Among the included studies, 7 prototypes have been specifically designed for elderly patients.
Strengths of these systems are that they are based on standard PR protocols following the guidelines provided by the American Thoracic Society and the European Respiratory Society: cycling on a stationary bike for those referring to physical training; “pursed-lip breathing” and “holding breath and coughing” for those pertaining breathing training.
The most common visualization modality is the flat screen (either PC or TV monitors), which is cheap and simple to use both for clinicians and for patients. This is in line with most of the rehabilitation systems for the elderly, even if, in recent years, more complex and immersive systems are successfully spreading in other fields, e.g. in neuro-motor rehabilitation.13
As explained in §1, the level of immersion, which is defined by the number and range of motor and sensory channels involved, influences the sense of presence and, as a consequence, may positively alter the effectiveness of the VR-based training. The importance of presence makes VR different to exergaming, which uses video feedback or distraction techniques (e.g., watching a video) where presence is not required. Our analysis demonstrates the first attempts to introduce more immersive solutions in PR too. Projected screens represent a valuable solution for providing a wider FOV, which should make the user feel more present in the VE, even if they require a proper set up and a dedicated room. This may be the reason why only three studies have preferred such a solution. Head Mounted Displays provide a higher level of immersion—and consequently sense of presence—and are more portable, while there are still concerns about using such devices for this group of patients. Regarding technical aspects of HMDs and their acceptability, the few available studies show different results. In one situation, most participants tolerated wearing the helmet well, but even though they found the experience acceptable, some of them would hav appreciated a lighter weight device. In the second case, most patients complained about the weight of the device and the over sweating induced. The differing results are likely to be related to the different headsets used.
The other factor influencing presence is the interaction, which depends on the device through which the interaction is made possible and the feedback provided to the user (see Table 1). The more realistic the interaction—i.e. the user reacts as if he/she were actually there—the higher the level of ecological validity, which represents an important advantage of VR.56 Interaction with the virtual contents was simple and natural in most of the analysed systems thanks to specific embedded sensors (e.g. accelerometers, encoders, acoustic sensors) able to measure the physical performance, e.g. in terms of hand’s position and rotation, cycling speed and breathing rate. In most studies, physiological parameters were assessed using external devices both to assure safety and to assess primary outcomes (e.g. heart rate, energy expenditure). Embedding monitoring functionality in the applications may represent a step towards more efficient and more complete solutions, able both to provide a comprehensive overview to the clinicians and to be used by the patients at home with low supervision.
Given these characteristics, studies showed that VR-based training (aerobic, strength and breathing exercises) is feasible and safe for patients. A technological solution for health should be feasible—from technical, organisational and economic points of view—and safe, especially when dealing with vulnerable people, e.g. elderly, children, patients.26 Regarding the studies analysed, the feasibility has been proven both as an alternative solution to standard protocols and as integrative one. Although few studies demonstrated that home-based training is feasible, most of them preferred a supervised scenario with an expert clinician constantly monitoring and guiding the patient. Further research should focus on evaluating feasibility in unsupervised situations. Continuity of care at home is indeed one of the main challenges in improving PR and the treatment of chronic conditions in general. Furthermore, promoting effective home-based rehabilitation is becoming more and more crucial, also given the recent COVID-19 pandemic, which has highlighted the need for more effective interventions that do not require patients, who are at higher risk of a more severe infection, to physically go to hospitals or clinical care facilities. Regardless of the level of supervision, we found that a familiarization session and step-by-step instructions are needed in order to make the patients—even the less confident—feel comfortable with technology.
As most of the studies are based on commercial exergames—which undergo product testing before being launched into market—only few studies evaluated the usability. Despite the scarcity of information, our analysis suggests that further research is needed to understand if more complex systems—such as HMDs—with a high level of interaction and immersion can be effectively used with COPD patients. In particular, the most advanced HMDs should be evaluated in order to guarantee the most comfortable experience thus avoiding weight and over sweating issues. Usability is a crucial requirement, especially for those users, such as the elderly, who may be less confident with technology; however, there are other factors influencing the individual adoption of a technological solution which are worth investigating.
Only two studies presented results on acceptability; both showed that VR-based systems are considered useful and are well accepted by patients, who would like to have them at home. All patients were satisfied with this innovative way of training and enjoyed the virtual contents. They all found the proposed intervention highly motivating both because it distracts them from negative sensations (e.g. fatigue and breathlessness) and because it generates a report that the therapist can access thus inducing a sense of responsibility. Despite some evidence, the impact of these “human” factors on the motivation, engagement and, therefore, on the clinical outcomes is still under investigated.
ConclusionsIn this paper, we investigate the use of Virtual Reality as a promising solution to improve both at home and in-hospital PR, providing a technological perspective and focusing on subjective experience of patients. Despite an increasing number of studies showing encouraging results demonstrating feasibility, acceptability and safety of VR for physical and breathing training of COPD, further research is needed. In particular, most of the systems identified are commercial exergames and are characterized by low levels of immersion and interaction. Further research should investigate whether higher immersion (e.g. using head mounted displays) and a more natural interaction (e.g. integrating physiological and motion sensors) enhances the rehabilitation outcomes, e.g., by inducing attentional shift from negative sensations.
Given the variety of factors affecting the successful implementation of technological solutions for health, cooperation between developers and clinicians is fundamental in order to maximize the benefits of VR for COPD rehabilitation. Only in this way can ad-hoc VR systems be built which exploit the most advanced technologies and which, at the same time, follow rigorous clinical protocols, with a real impact on patients’ quality of life.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors have no conflicts of interest to declare.