Even though chronic obstructive pulmonary disease (COPD) is primarily a disease of the respiratory system, limb muscle dysfunction characterized by muscle weakness, reduced muscle endurance and higher muscle fatigability, is a common secondary consequence and a major systemic manifestation of the disease. Muscle dysfunction is especially relevant in COPD because it is related to important clinical outcomes such as mortality, quality of life and exercise intolerance, independently of lung function impairment. Thus, improving muscle function is considered an important therapeutic goal in COPD management. Pulmonary rehabilitation (PR) is a multidisciplinary, evidence-based and comprehensive approach used to promote better self-management of the disease, minimize symptom burden, optimize functional status, and increase participation in activities of daily life. Exercise training, including cardiovascular and muscle exercises, is the cornerstone of PR and is considered the best available strategy to improve exercise tolerance and muscle function among patients with COPD. This paper addresses the various components of exercise training within PR used to improve limb muscle function in COPD, providing clinicians and health-care professionals with an overview and description of these various exercise modalities and of their effects on limb muscle function. Guidance and recommendations to help design optimal limb muscle training regimens for these patients are also presented.
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality worldwide. The international prevalence of Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 2 and higher COPD is estimated to be 10%, a figure that is steadily increasing.1,2 COPD is estimated by the World Health Organization to be the third leading cause of death in 2030.3 Although COPD is characterized by chronic airflow limitation, limb muscle dysfunction is a common consequence and a major systemic manifestation in COPD.4–6 Limb muscle dysfunction is associated with important clinical outcomes such as increased mortality,7,8 reduced quality of life,9 greater healthcare utilization,10 and exercise intolerance,11–13 independently of lung function impairment. Exercise intolerance is considered one of the key disabling factors in COPD with dyspnea and leg fatigue being the most frequently reported exercise limiting symptoms.4,14 Clinical manifestations of limb muscle dysfunction in COPD include muscle atrophy, weakness, reduced endurance, and/or greater muscle fatigability.4 Assessment of limb muscle mass and limb muscle function in COPD is therefore highly encouraged and improving this common feature of COPD is an important therapeutic goal.6,15
This article provides clinicians and health-care professionals with an overview and description of the various exercise modalities used within pulmonary rehabilitation (PR) to improve limb muscle function, especially highlighting effective modalities at the muscle level. Our objective is to provide guidance and recommendations to help clinicians’ design optimal limb muscle training during PR for patients with COPD.
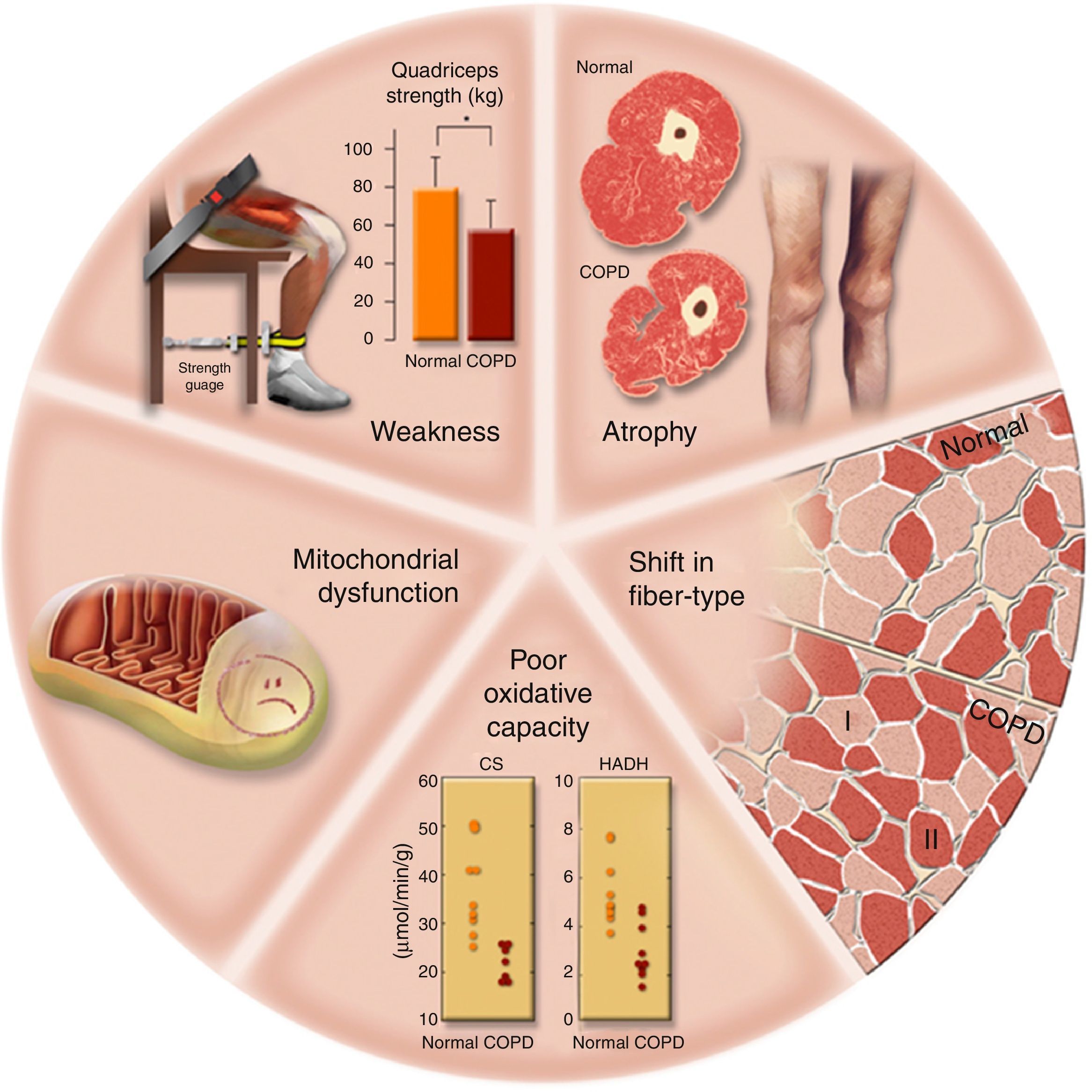
Limb muscle function in patients with COPDLimb muscle dysfunction encompasses muscle weakness, reduced endurance or greater muscle fatigability.15 Prevalence rates of muscle weakness ranges from 20 to 40% depending on disease severity,16 while reduced limb muscle endurance and muscle fatigue occur in 30–80% of patients with COPD.6,17,18 The impairment in limb muscles function in COPD is heterogeneous with strength and endurance of upper limbs seemingly more preserved than those of lower limbs.6,19–21 Decreased limb muscle strength and endurance, especially when involving lower limbs, are associated with reduced walking capacity22 and physical activity,13,20,23 exercise intolerance,11,24 morbidity, mortality as well as increased health care service use, dyspnea and poor quality of life.8,10,9,25 Lower limb muscles of patients with COPD also exhibit a greater susceptibility to fatigue than that of age-matched healthy individuals.13,26 Limb muscle dysfunction is the end result of several muscle structural, molecular and cellular alterations which are summarized in Fig. 1 and include weakness, atrophy, fiber-type distribution shifts, reduced oxidative capacity, mitochondrial dysfunction, and reduced capillarisation that are mediated by numerous etiological factors.6,27,28 These include sedentarity, poor nutritional status, repeated COPD exacerbations and systemic use of corticosteroids.5 Other relevant etiological factors include cigarette smoke, hypoxia, hypercapnia and acidosis, metabolic alterations of several types including vitamin D and testosterone deficiencies, systemic inflammation and co-morbidities.5,6,29
Morphological and structural alterations reported in limb muscles in patients with chronic obstructive pulmonary disease (COPD). CS, citrate synthase; HADH, 3-hydroxyacyl CoA dehydrogenase. Reprinted with permission of the American Thoracic Society. Copyright © 2016 American Thoracic Society.
In patients with COPD, limb muscle strength is a determinant of the level of physical activity30 and of functional capacity4. Moreover, muscle strength is related to dyspnea as well as to quality of life.10,8 Quadriceps muscle strength significantly predicts mortality in COPD8, while weakness is associated with impaired balance and an increase risk of falls.31 Despite its clinical relevance, muscle strength mostly reflects the action of fast-twitch fibers32 and represents only one aspect of limb muscle function.13 Limb muscle endurance, defined as the muscle's ability to sustain or repeat a specific task over time,33 and muscle fatigability, the reversible reduction in force generated by the muscle during a given task, reflect other aspects of muscle function such as muscle oxidative capacity and oxygen supply34 that are relevant to the endurance tasks that are part of daily life physical activities of patients with COPD.35,36 Limb muscle endurance is also related to walking capacity and upper limb muscle function in COPD.22 An important concept is that strength and endurance cannot be predicted from each other as they reflect different muscle properties.37 Understanding that strength and endurance are both clinically important and that they reflect different muscle properties is important in the design of rehabilitative interventions aimed at improving limb muscle function in COPD.
Pulmonary rehabilitation (PR)PR is an individualized, comprehensive and multidisciplinary approach that involves exercise training, education, psychosocial support, and nutritional interventions, in order to promote better self-management of the disease, minimize symptom burden, optimize functional status, and increase participation in activities of daily life.38–41 Body composition abnormalities (such as weight loss and muscle wasting) are prevalent in COPD.6,42 Sarcopenia has been reported in about 15% of patients with COPD and impairs function and health status of the individual patient. Patients with COPD and sarcopenia have reduced exercise capacity, functional performance, level of physical activity and health status compared with patients with COPD without sarcopenia.43 Nutritional interventions, dietary counseling, food fortification, and supplementation44,45 are recommended and may be efficient for increasing weight, fat-free mass, exercise tolerance as well as survival in compliant patients. Educational sessions should address smoking cessation, basic information about COPD and pathophysiology of the disease, general approach to therapy and specific aspects of medical treatment, strategies to help minimize dyspnea, advice about when to seek help, self-management and decision making during exacerbations, and advance directives and end-of-life issues.3,46 PR is perhaps the best example of evidence-based medicine in pulmonology as it improves, among other things, exercise capacity, health-related quality of life, as well as relieving dyspnea and fatigue.47 Risks of hospitalization, mortality,38,47 and healthcare utilization costs 48 are also reduced with PR. Although there is currently no consensus regarding the optimal duration of a PR program, the current recommendations suggest 8–12 weeks, while keeping in mind that extending this length might benefit patients who need more time to achieve clinical improvements.38,49 Even though the content of PR may vary depending on factors such as healthcare systems, resources, personnel or settings, individually tailored exercise training is considered the cornerstone of PR.47 Whole body aerobic training involving upper and lower extremities and strengthening exercises are recommended components of exercise training in patients with COPD.40 Exercise training within the context of PR is also considered one of the best available means to improve limb muscle function in COPD, demonstrating increase limb muscle strength, limb muscle endurance as well as reduced fatigability.40
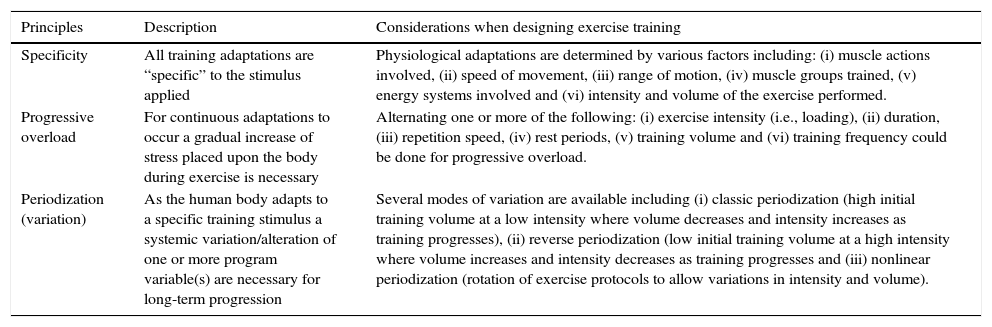
It is recommended that an exercise assessment be carried out before commencing PR and exercise training in order to tailor the exercise prescription to the individual's specific requirements and goals.40,50 Such an assessment should include evaluation of exercise capacity and of muscle function. Design of exercise programs should always be based on the foremost principles of exercise training, including but not limited to, the principles of specificity, progressive overload and variation51 (Table 1). Firstly, the principle of specificity states that all training adaptations are specific to the stimulus applied.52 Second, the above discussion about muscle strength,53 endurance and fatigability implies that specific interventions are required to address these different aspects of muscle function. Lastly, specific aims of the training should be kept in mind in designing the program.
Principles of exercise training.
| Principles | Description | Considerations when designing exercise training |
|---|---|---|
| Specificity | All training adaptations are “specific” to the stimulus applied | Physiological adaptations are determined by various factors including: (i) muscle actions involved, (ii) speed of movement, (iii) range of motion, (iv) muscle groups trained, (v) energy systems involved and (vi) intensity and volume of the exercise performed. |
| Progressive overload | For continuous adaptations to occur a gradual increase of stress placed upon the body during exercise is necessary | Alternating one or more of the following: (i) exercise intensity (i.e., loading), (ii) duration, (iii) repetition speed, (iv) rest periods, (v) training volume and (vi) training frequency could be done for progressive overload. |
| Periodization (variation) | As the human body adapts to a specific training stimulus a systemic variation/alteration of one or more program variable(s) are necessary for long-term progression | Several modes of variation are available including (i) classic periodization (high initial training volume at a low intensity where volume decreases and intensity increases as training progresses), (ii) reverse periodization (low initial training volume at a high intensity where volume increases and intensity decreases as training progresses and (iii) nonlinear periodization (rotation of exercise protocols to allow variations in intensity and volume). |
In the latest official American Thoracic Society/European Respiratory Society (ATS/ERS) statement on key concepts and advances in PR, increasing muscle strength was highlighted as an important goal of rehabilitation in COPD.40 Aerobic exercises such as walking and cycling have been found to increase muscle strength in patients with COPD.37,54,55 Aerobic exercise, either of interval or constant-load modalities also increases muscle cross-sectional area (CSA)56–58 and reduces the proportion of type IIx fibers in the quadriceps.57,58 Metabolic adaptations, such as, but not limited to, increased oxidative capacity of the quadriceps muscle and reduction in exercise induced lactic acid production are also seen after aerobic training protocols in patients with COPD.6,57,58 Even though the optimal intensity is still debatable, higher intensities (>60% of maximal work rate) seems to be preferable over lower aerobic training intensities to induce a physiological adaptation to training.59
Nevertheless, if the goal is to improve muscle strength, resistance training has a greater potential than aerobic training protocols.40 Greater effects on muscle strength are obtained with resistance training in comparison to aerobic training or when resistance training is added to an aerobic training protocol.40,55,60–62 The tolerability of resistance training is also considered to be superior to that of aerobic training since it results in less exercise induced dyspnea,63 allowing more patients to reach targeted exercise intensities, thus optimizing the effect of the exercise performed. As all training adaptations are specific to the stimulus applied (principle of specificity),52 greater effects on muscle strength are expected with resistance training protocols as these regimens are specifically designed for increasing muscle strength, particularly when they use fairly large weights and a low number of repetitions (often 8–15 repetitions).62,64 In contrast, aerobic based protocols (involving submaximal contractions over a long time, normally 20–60minutes or more)40 use a different exercise setup that might not be optimal to increase limb muscle strength.52
Muscle fiber CSA, arrangement of muscle fibers according to their pennation angle, muscle length, joint angle and contraction velocity are all factors influencing muscle strength.6,52 Increases in mid-thigh CSA, diminished inflammation and stimulation of satellite cells (which maintain muscle mass and contribute in muscle fibers regeneration)65 have all been shown after resistance training regimes in COPD. Other limb muscle adaptations following resistance training included upregulation of muscle insulin-like growth factor-I system as well as of myogenic regulatory factors.66
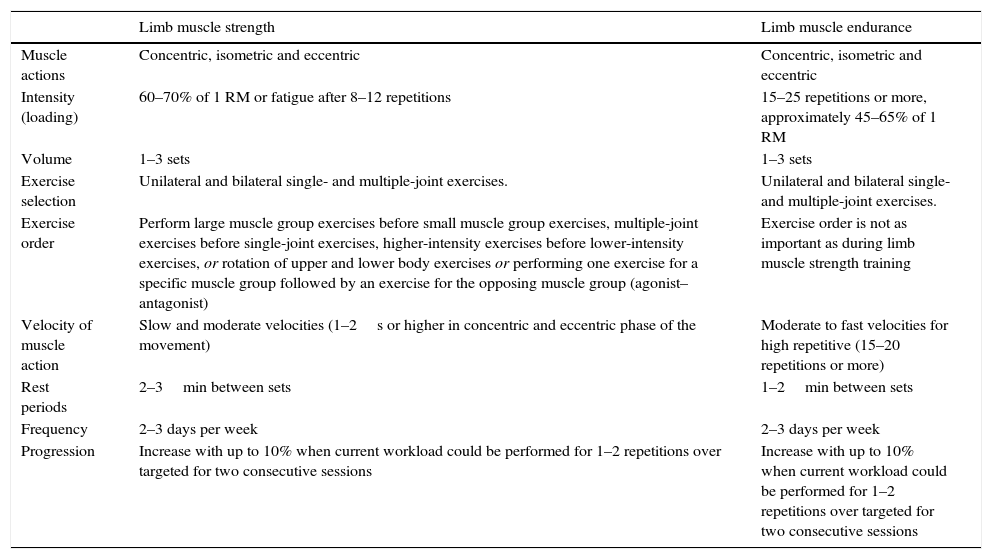
The optimal resistance training prescription for patients with COPD has yet to be determined.40 The American College of Sports Medicine (ACSM) guidelines for enhancing muscle strength in older adults are useful to consider for patients with COPD (Table 2). The ACSM recommends performing resistance training, 1–3 sets of 8–12 repetitions undertaken against high load on 2–3 days each week. Initial loads equivalent to either 60–70% of the one repetition maximum (1 RM) (that is, the maximal load that can be moved only once over the full range of motion without compensatory movements) or one that evokes fatigue after 8–12 repetitions are recommended. It is further proposed that exercise dosage must increase over time (following the exercise principle of progressive overload) to facilitate improvements in muscular strength and muscle mass).40,52 This overload can be achieved by increasing the resistance or weight, increasing the repetitions per set, increasing the number of sets per exercise, and/or decreasing the rest period between sets or exercises52,67 (Table 1). The majority of studies that have investigated the effects of resistance training on muscle strength in COPD have used exercise approaches similar to the ACSM recommendations.64 Nevertheless, other resistance training approaches, such as 4 sets of 5 repetitions at 85–90% of 1 RM,68 6–8 repetitions at 70–85% of 1 RM66,69 and even 2 sets of 20–25 repetitions at 40–55% of 1 RM have demonstrated significant increases in muscle strength among patients with COPD.70,71
Resistance training recommendations for improving limb muscle function.
| Limb muscle strength | Limb muscle endurance | |
|---|---|---|
| Muscle actions | Concentric, isometric and eccentric | Concentric, isometric and eccentric |
| Intensity (loading) | 60–70% of 1 RM or fatigue after 8–12 repetitions | 15–25 repetitions or more, approximately 45–65% of 1 RM |
| Volume | 1–3 sets | 1–3 sets |
| Exercise selection | Unilateral and bilateral single- and multiple-joint exercises. | Unilateral and bilateral single- and multiple-joint exercises. |
| Exercise order | Perform large muscle group exercises before small muscle group exercises, multiple-joint exercises before single-joint exercises, higher-intensity exercises before lower-intensity exercises, or rotation of upper and lower body exercises or performing one exercise for a specific muscle group followed by an exercise for the opposing muscle group (agonist–antagonist) | Exercise order is not as important as during limb muscle strength training |
| Velocity of muscle action | Slow and moderate velocities (1–2s or higher in concentric and eccentric phase of the movement) | Moderate to fast velocities for high repetitive (15–20 repetitions or more) |
| Rest periods | 2–3min between sets | 1–2min between sets |
| Frequency | 2–3 days per week | 2–3 days per week |
| Progression | Increase with up to 10% when current workload could be performed for 1–2 repetitions over targeted for two consecutive sessions | Increase with up to 10% when current workload could be performed for 1–2 repetitions over targeted for two consecutive sessions |
RM, repetition maximum.
In addition to aerobic and resistance training protocols, transcutaneous neuromuscular electrical stimulation (NMES) training may also increase muscle strength in COPD.72 The technology induces muscle contractions by depolarizing motor neurons through the application of an electrical current via electrodes placed on the skin over the targeted muscles. NMES is a feasible alternative to resistance training in severely disabled patients in whom the tolerance to traditional whole body training might be compromised.72,73 High-frequency NMES, is recommended over low-frequency NMES and has shown comparable muscle strengthening effects than resistance training in severely dyspneic patients with COPD.74 NMES could also be an alternative for home use and in this context, may increase in type II fiber CSA with a decrease in type I fiber CSA of the quadriceps muscle in patients with COPD.75
Increasing limb muscle enduranceLimb muscle endurance is decreased among patients with COPD, often to a larger magnitude than strength.18,76 Limb muscle endurance is also seemingly more closely related to walking capacity as well as to upper limb muscle function than limb muscle strength in this group of patients.22 However, although the effects of PR on limb muscle strength are well documented, the effect of PR on limb muscle endurance has not been investigated to the same extent. Available data suggest that exercise training improves lower as well as upper extremity functional capacity, demonstrated by increased walking capacity, arm endurance and arm function following eight weeks of high-repetitive resistance training.70 The decrease in limb muscle endurance reported in patients with COPD is at least partly related to intrinsic muscle abnormalities, and the need to include some forms of muscle-specific training is warranted if one goal of PR should be to increase limb muscle endurance.18 There are currently no specific recommendations on how to increase limb muscle endurance among patients with COPD. ACSM nevertheless suggests that healthy adults perform multiple sets of resistance exercises using light loads involving 15–25 repetitions or more, 2–3 days each week with moderate to fast repetition velocities and rest periods between 1 and 2min (Table 2). There is no specific recommendation concerning the percentage of 1 RM at which exercises should be performed,52 but 40–65% of 1 RM has been used during resistance training among patients with COPD allowing 15–25 repetitions per set. This strategy was followed by Nyberg et al. 2015, incorporating upper and lower extremity exercises performed during 25 repetitions at 55% of 1 RM and it resulted in increases in both upper and lower limb muscle endurance as well as increases in quadriceps strength, walking distance and arm function.70 A similar approach was used by Wurtemberger and Bastian,71 however no measurements of limb muscle endurance was performed. Another type of low intensity limb muscle training was tested by Clark et al.77 and was composed of 10 upper and lower-body home exercises undertaken for 30s (with 15-s progressions up to 60s) every day during 12 weeks with only body weight used as resistance. These authors reported increased isotonic upper (shoulder flexion) and lower (knee extension and flexion) limb muscle endurance, and reduced ventilation during exertion in the trained group compared to the control group. Finally, a study by Arnardottir et al.78 also utilized a high number of repetitions, (15–20 repetitions at 65% of 1 RM), however no assessment of limb muscle function was incorporated. Intrinsic mechanisms explaining the effects of high-repetitive resistance training on limb muscle endurance in patients with COPD still require further investigation. In healthy untrained men, an increased percentage of type IIAX muscle fibers, myosin heavy chain isoform and muscle CSA have been demonstrated following eight weeks of high-repetitive (20–28 RM) resistance training.79 In addition to being associated with improved limb muscle endurance, high-repetitive resistance training may also improve oxygen uptake and increased maximal mitochondrial respiration in trained muscles.80
Quadriceps muscle endurance could also be improved using NMES in patients with COPD.74 Even though high-frequency NMES seem to result in greater improvements of muscle endurance than low-frequency NMES, both low- and high-frequency NMES have shown effects on muscle endurance comparable of those achieved from a strength training protocol.74 However, interpretation of the comparable results on limb muscle endurance should be treated with caution considering that the strength training protocol used included 4 sets of 8 repetitions at 70% of 1 RM, i.e., not in line with ACSM recommendations for increasing limb muscle endurance.52 Lastly, phototherapy with combination of super-pulsed laser and light-emitting diodes can increase quadriceps muscle endurance when compared to a placebo treatment. However, the trial was small and the effect in comparison to a resistance training protocol was not investigated.81
Studies using aerobic exercise modalities (e.g., interval or continuous cycling protocols) often lack specific assessment of the limb muscle.18 Nevertheless, quadriceps muscle endurance was evaluated by O’Donnell et al.,37 who did not see any changes in quadriceps muscle endurance following 6 weeks of walking, treadmill and cycling exercises for the lower limbs. The main focus of aerobic training studies has been to demonstrate the positive impact of exercise training on muscle determinants of muscle endurance such as muscle fiber capillarization, mitochondrial density and oxidative capacity.57,82 More research on the specific effects of aerobic training on limb muscle endurance is warranted.
DiscussionIf the goal of exercise training is to improve specific aspects of limb muscle function such as strength and endurance, resistance training should be preferred over other available exercise modalities within PR. Resistance training protocols seem superior to aerobic training protocols with regard to increasing limb muscle function, especially limb muscle strength, in patients with COPD.37,40,52,55,60–62 Other exercise alternatives such as high-frequency NMES are feasible, especially in more severe patients,72 but more studies are needed to compare their effects with those of traditional exercise training protocols.
The requirements for improving limb muscle strength or endurance are different and this has serious implications for the exercise training approach to be used for optimal benefits. The exercise programs should be built on the founding principles of exercise training (progressive, overload, specificity and variation) (Table 1) and individualized and adapted to the specific goals of treatment. It would seem advisable to follow ACSM recommendations40,52 for increasing limb muscle strength or limb muscle endurance (Table 2).
The vast majority of resistance training regimens, aimed at improving limb muscle function in patients with COPD has used weight machines as a primary choice of exercise equipment.62,64 However, there is a growing evidence in COPD that exercise training using minimal equipment such as body weight and/or elastic resistance bands is also effective in improving both limb muscle strength and limb muscle endurance.70,83,84 The use of elastic resistance bands is also considered clinically applicable both for patients as well as care providers and could be considered a practicable and less costly alternative to weight machines,85 that could be more easily implemented outside specialized centers. The principle of progressive overload and, to some extent, the principle of specificity have been used in resistance training regimes for patients with COPD. However, variation or periodization which could be done by systemic variations of, for example, exercise volume and intensity, is rarely incorporated. Since the body adapts quickly to exercise regimens, variations in training parameters may help to ensure continual progression and optimization of the training intervention.52 Classic, reverse or undulation variation strategies could theoretically be used, however data on patients with COPDs are lacking.40 In one study, nonlinear exercise training was found to be superior to traditional non-varied exercise training with regard to improving aerobic work capacity on cycle ergometry.86 The potential use of nonlinear periodization in resistance training for improving limb muscle function among patients with COPD is interesting, but has yet to be investigated. Since improving limb muscle strength and endurance requires different exercise approaches, a periodized exercise approach including both high load, low-repetitive (muscle strength) and low load, high-repetitive (muscle endurance) components would appear to be a promising approach in this group of patients.
Conflicts of interestThe work was funded with grants from the CIHR/GSK Research Chair on COPD, Université Laval, The Swedish Heart and Lung Foundation and The Fonds de recherche du Québec – Santé (FRQS).
François Maltais reports grants and lecture fees from Boehringer Ingelheim, GlaxoSmithKline and Novartis. François Maltais holds a CIHR/GSK research Chair on COPD at Université Laval.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
The work was funded with grants from the CIHR/GSK Research Chair on COPD, Université Laval, The Fonds de recherche du Québec – Santé (FRQS) and The Swedish Heart and Lung Foundation.