To investigate the relationship between mucociliary transport and physical activity in daily life (PADL) in smokers and nonsmokers.
MethodsFifty-two current smokers were submitted to an assessment of mucociliary transport (saccharin transit time, STT), carbon monoxide levels in the exhaled air, lung function and smoking history. In addition, subjects kept a pedometer worn at the waist for six days in order to determine their level of PADL (steps/day). The tests were also performed on 30 matched healthy nonsmokers who served as control group.
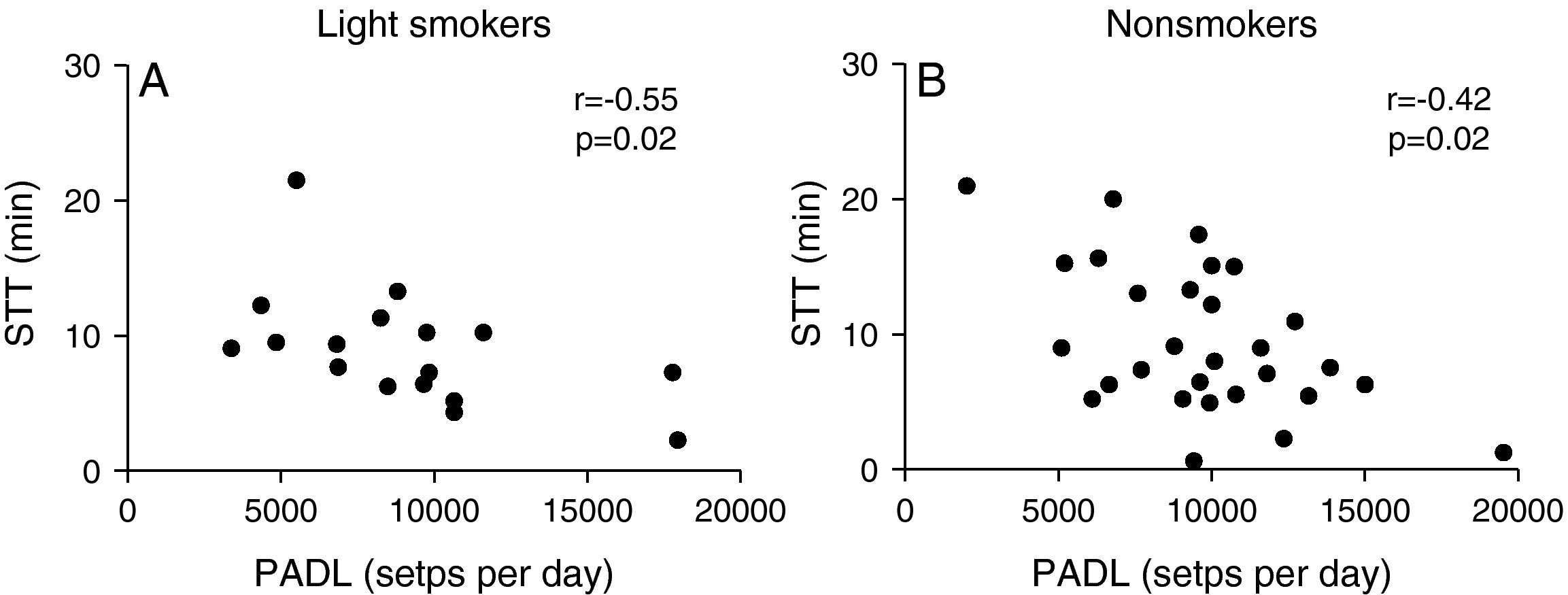
ResultsLight smokers (≤15 cigarettes/day) had a STT of 9 (7–11) min (median [confidence interval]), which was similar to nonsmokers (8 [8–11]min; p=0.8). Both moderate (16–25 cigarettes/day) and heavy (>25 cigarettes/day) smokers had a significantly higher STT (13 [11–17]min and 13 [10–21]min, respectively) than nonsmokers and light smokers (p<0.05 for all). There was no difference in the number of steps/day between any of the groups (p>0.05 for all). In the general group of smokers, STT was not significantly correlated with PADL, pack/years index, years of smoking or age (r<−0.23; p>0.09 for all). There was significant negative correlation between STT and PADL only in light smokers (r=−0.55; p=0.02) and nonsmokers (r=−0.42; p=0.02), but not in moderate and heavy smokers.
ConclusionIn light smokers and non-smokers, better mucociliary function is associated to higher daily physical activity level, as opposed to the decreased mucociliary function observed in smokers, i.e., those with moderate and heavy cigarette consumption.
Investigar a relação entre o transporte mucociliar e a atividade física na vida diária (AFVD) em fumantes e não fumantes.
MétodosCinquenta e dois fumantes foram submetidos à avaliação do transporte mucociliar (Tempo de Trânsito de Sacarina, TTS), dos níveis de monóxido de carbono no ar expirado, da função pulmonar e do histórico tabagístico. Além disso, os sujeitos permaneceram por 6 dias com um pedómetro para determinar o seu nível de AFVD (passos/dia). Os testes também foram realizados em 30 indivíduos não fumantes saudáveis, pareados, que serviram como grupo controlo.
ResultadosOs fumantes leves (≤15 cigarros/dia) apresentaram um TTS de 9 (7-11) minutos (mediana [intervalo de confiança]), que foi similar aos não-fumantes (8 [8-11] min; p=0,8). Ambos os fumantes moderados (16-25 cigarros/dia) e severos (>25 cigarros/dia) apresentaram TTS significativamente maior (13 [11-17] min e 13 [10-21] min, respetivamente) do que os não fumantes e fumantes leves (p<0,05 para todos). No grupo de fumantes em geral, não houve correlação estatisticamente significante entre o TTS e AFVD, índice anos/maço, anos de tabagismo e idade (r<-0,23; p>0,09 para todos). Houve correlação negativa significativa entre o TTS e a AFVD apenas em fumantes leves (r=-0,55; p=0,02) e não fumantes (r=-0,42; p=0,02), mas não em fumantes moderados e pesados.
ConclusãoEm fumantes leves e não fumantes, uma melhor função mucociliar está associada a maiores níveis de atividade física diária, ao contrário dos fumantes com função mucociliar diminuída, ou seja, aqueles com consumo moderado e severo de cigarros.
Studies have shown that the effectiveness of mucociliary clearance is impaired in smokers compared to nonsmokers.1,2 It is also known that, in nonsmokers, regular physical activity when performed at moderate intensity improves the immune system response.3 However, the relationship between physical activity and mucociliary transport is not completely clear and has shown conflicting results. Wolff et al.4 observed a slight increase in mucociliary clearance after exercise, unlike Olseni and Wollmer5 who observed no substantial changes. Furthermore, these studies only described the acute (i.e., transient) response of the mucociliary system to exercise, but the chronic adaptive response to regular daily physical activity remains unknown. In addition, these studies were performed only in nonsmokers, and to the authors’ best knowledge, no studies involving this issue had yet been carried out in smokers.
Thus, the aim of this study was to describe the relationship between mucociliary transport and the level of physical activity in daily life (PADL) in healthy smokers (i.e., with no lung function impairment) and healthy nonsmokers.
Materials and methodsDesign and study subjectsThis cross-sectional observational study was undertaken with a convenience sample of 52 current smokers (Table 1) assessed during intake process before starting a program with the aim of increasing their daily physical activity. They were volunteers and had learned about the project through advertisements in the media, buses and health centers. Inclusion criteria were: current smoking; normal lung function (according to internationally accepted criteria)6; and absence of history of cystic fibrosis, bronchiectasis, immotile cilia syndrome, nasal surgery or trauma and chronic and/or recent inflammation process in the upper airway which was established during an initial interview. Exclusion criterion was the presence of bone, nervous and/or muscle dysfunction which could interfere in the objective assessment of PADL. Subjects were included regardless of whether they intended to quit smoking in the future or not, and no subject quit or reduced smoking during the assessment period. No pharmacological treatment for smoking or any other reason was provided during the assessment period. For comparison, a group composed of 30 healthy nonsmokers (Table 1) was also assessed. This group was matched to the smoker groups by similar age, gender and body mass index.
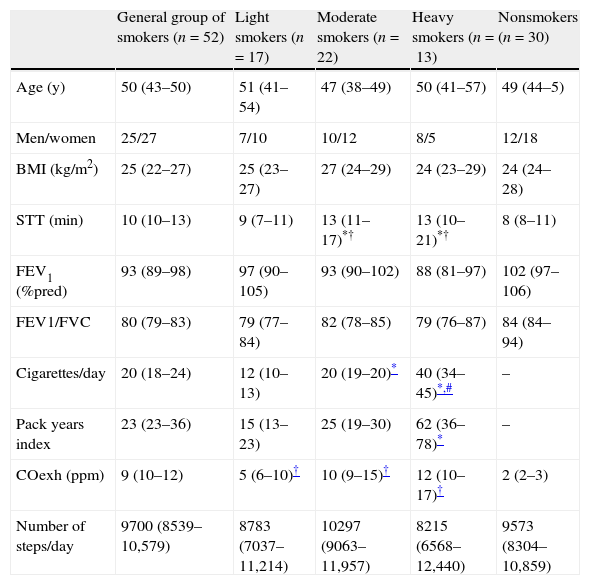
Characteristics of the groups of smokers and nonsmokers.
| General group of smokers (n=52) | Light smokers (n=17) | Moderate smokers (n=22) | Heavy smokers (n=13) | Nonsmokers (n=30) | |
| Age (y) | 50 (43–50) | 51 (41–54) | 47 (38–49) | 50 (41–57) | 49 (44–5) |
| Men/women | 25/27 | 7/10 | 10/12 | 8/5 | 12/18 |
| BMI (kg/m2) | 25 (22–27) | 25 (23–27) | 27 (24–29) | 24 (23–29) | 24 (24–28) |
| STT (min) | 10 (10–13) | 9 (7–11) | 13 (11–17)*† | 13 (10–21)*† | 8 (8–11) |
| FEV1 (%pred) | 93 (89–98) | 97 (90–105) | 93 (90–102) | 88 (81–97) | 102 (97–106) |
| FEV1/FVC | 80 (79–83) | 79 (77–84) | 82 (78–85) | 79 (76–87) | 84 (84–94) |
| Cigarettes/day | 20 (18–24) | 12 (10–13) | 20 (19–20)* | 40 (34–45)*,# | – |
| Pack years index | 23 (23–36) | 15 (13–23) | 25 (19–30) | 62 (36–78)* | – |
| COexh (ppm) | 9 (10–12) | 5 (6–10)† | 10 (9–15)† | 12 (10–17)† | 2 (2–3) |
| Number of steps/day | 9700 (8539–10,579) | 8783 (7037–11,214) | 10297 (9063–11,957) | 8215 (6568–12,440) | 9573 (8304–10,859) |
Values are described as median (95% confidence interval).
BMI: body mass index; STT: saccharin transit time; FEV1: forced expiratory volume in the first second; COexh: carbon monoxide in the exhaled air.
For analysis purposes, smokers were divided into three groups according to the intensity of cigarette consumption: light smokers (n=17), who smoked up to 15 cigarettes/day; moderate smokers (n=22), 16–25 cigarettes/day, and heavy smokers (n=13), more than 25 cigarettes/day (Table 1).7 All participants had been previously informed about the objectives and procedures of the study and, after signing the consent form, became part of the research. The study was approved by the institution's Committee of Ethics in Research (No. 007/07).
ProtocolAll individuals included in the study were interviewed to obtain personal data and smoking history (duration of smoking, number of cigarettes per day, pack/years index) and were then assessed for lung function (by spirometry), mucociliary transport (by saccharin transit time) and carbon monoxide (COexh) levels in the exhaled air (MicroCO Meter). The tests were performed in an environment with controlled temperature and relative humidity. All assessments were performed in the morning, between 8:00 and 10:00h, after a period of 12h of tobacco abstinence which started after the last cigarette smoked the previous evening (between 20:00 and 22:00h, according to formal instructions given to the patients and confirmed by them). In addition, subjects remained for six days with a waist-worn pedometer (DigiWalker SW-200 Yamax, Japan) in order to determine the level of PADL (number of steps/day).
Lung function assessmentSpirometry was performed by Spirobank-MIR (MIR, Italy) 3.6, connected to a microcomputer. The technique was in accordance with the recommendations of the American Thoracic Society and European Respiratory Society guidelines.8 Reference values were specific for the Brazilian population.9
Measurement of mucociliary transport (MCT): the saccharin transit time (STT)Measurement of MCT was performed by STT, as described by Rutland and Cole.10 The test was shown to be valid and reproducible.11,12 Subjects were seated and positioned with the head slightly extended. Granulated sodium saccharin (5μg) was deposited under visual control 2cm inside the right nostril. The time from the placing of the particle to the first perception of a sweet taste in the mouth was recorded in minutes. Participants were instructed to maintain the original position and were not allowed to breath deeply, talk, cough, sneeze or sniff. They were also instructed to swallow only a few times per minute until they felt a sweet taste in the mouth. If they could not taste anything within 60min, the test was stopped and the subjects’ ability to perceive the taste of saccharin was evaluated by placing it on the tongue, and then the procedure was repeated in another occasion.10,12 Participants were strictly instructed not to use pharmacological agents such as anesthetics, analgesics, barbiturates, tranquilizers and antidepressants as well as alcohol and caffeine-based substances for at least 12h before the test.
Measurement of carbon monoxide levels in the exhaled air (COexh)The COexh was measured by a CO analyzer (MicroCO Meter Micro Medical Ltd., Rochester, UK), using an electrochemical sensor, for confirmation of smoking. Subjects were instructed to breathe deeply, hold their breath for 20s and to exhale slowly and completely through the mouthpiece. Values above 6ppm COexh were indicative of smoking.13
Assessment of physical activity in daily life (PADL)The level of PADL was assessed by monitoring the number of steps/day with a pedometer Digiwalker SW200 (Yamax, Japan). The equipment is simple, small, relatively inexpensive and worn on the right side of the waist (in line with the knee). Previous literature14 clearly showed that the use of pedometers, especially the model used in this study, provides a reliable estimate of the number of steps performed by an individual in a given period of time. Classification of PADL level according to steps/day was: <5000steps/day, “sedentary”; 5000–7499, “low active”; 7500–9999, “somewhat active”; ≥10,000, “active”; and >12,500, “highly active”.
The pedometer was used for six consecutive days (Sunday to Friday) for at least 12h a day, and the number of steps/day was recorded daily by each individual in a logbook. For data analysis, the average of steps/day performed during the six days was used.
Statistical analysisStatistical analysis was performed with GraphPad Prism 3.0 (GraphPad Inc., San Diego, USA). Due to the relatively reduced number of subjects in each of the 3 groups of smokers, non-parametric statistics were used and results were expressed as median (95% confidence interval). Comparison among the 3 groups of smokers was performed by the Kruskal–Wallis test (Dunns pos-hoc test). For the comparison between nonsmokers and the general group of smokers, the Mann–Whitney test was used. Correlations were evaluated using the Spearman coefficient. The level of statistical significance was set at p<0.05 for all analysis.
ResultsEighty-two subjects entered the study (52 smokers and 30 nonsmokers), and none of them were excluded during the assessments. Results are shown in Table 1. All three groups of smokers had higher COexh than the nonsmokers group (p<0.05 for all). There was no difference in the number of steps/day between any of the groups (p>0.05 for all). According to the number of steps/day, there was a wide range of subjects with different activity levels, although in general, all groups could be classified as somewhat active to physically active (Table 1).
The median (confidence interval) of STT in light smokers showed no significant reduction in the mucociliary transport compared to nonsmokers (9 [7–11]min and 8 [8–11]min, respectively; p=0.08). Both moderate and heavy smokers had significantly higher STT values than nonsmokers (13 [11–17]min; p=0.04 and 13 [10–21]min; p=0.04, respectively) and light smokers (p=0.02 for both).
In the general group of smokers, no significant correlation occurred between STT and steps/day (r=−0.04; p=0.78). There was a negative significant correlation between STT and steps/day only in light smokers (r=−0.55; p=0.02) and in nonsmokers (r=−0.42; p=0.02) (Fig. 1). No such significant correlation was found in the groups of moderate (r=0.31; p=0.15) and heavy smokers (r=−0.36, p=0.23).
Furthermore, in the general group of smokers, there was no significant correlation between STT and pack/years index (r=−0.14; p=0.30), years of smoking (r=−0.13; p=0.37) and age (r=−0.23; p=0.09). Similarly, number of steps/day was not correlated to pack/years index (r=0.01; p=0.92), years of smoking (r=−0.18; p=0.22) and age (r=−0.03; p=0.81).
The power of the study was calculated by comparing the difference between two correlations, i.e., STT versus steps/day in the control group (0.42) and in the general group of smokers (0.04). By using an α=0.05 (double-sided) and a power of 80%, a total of 52 subjects provided a power of 0.82 in order to detect this difference.
DiscussionThis study showed that, specifically in smokers with light cigarette consumption and non-smokers, PADL is modestly but significantly associated with mucociliary function, unlike for smokers with moderate to severe cigarette consumption. Such results can be linked to the fact that there was no impairment in mucociliary transport in light smokers, while those with moderate to severe consumption showed impaired clearance. However, caution is required to avoid the interpretation of these results as describing a causative relationship between physical activity and mucociliary function, since the results are based solely on simple correlations.
Mucociliary transport (MCT) is the main defense mechanism of upper and lower airways15,16 and may be influenced by different conditions such as in response to stress, physical exercise and exposure to noxious particles (e.g., cigarette smoke).17 Physical exercise is, in general, classified as a stressful stimulus,18 but the MCT response to exercise can be divided into acute (i.e., transient) and chronic adaptation.19 The acute response to exercise is associated with increased levels of adrenergic mediators,20 which stimulate the ciliary beat frequency21,22 and thus the airways clearance. Some studies23–25 have confirmed this idea and found that the respiratory mucosa function is significantly altered by exercise, with improved activity during light-moderate exercise, and impaired activity after strenuous exercise. The novel feature of our study, however, was to investigate how the MCT behaves in relation to the regular level of physical activity (i.e., its chronic adaptation). In our view, the fact that the MCT in light smokers behaves similar to nonsmokers might underline the benefits of regular physical activity for the respiratory system in light smokers. However, in those who already have impairment in STT (i.e., moderate and heavy smokers), the mucociliary system is slowed down by the intensity of tobacco consumption regardless of the level of physical activity. Therefore, in these subjects, regular physical activity is not linked to MCT, but a substantial reduction in smoking intensity is required. On the other hand, as previously mentioned, the design of the present study does not provide solid proof of a causative relationship between higher PADL and better MCT.
The similarities between the results of light smokers and nonsmokers might be due to the degree of daily exposure to cigarette smoke for the former, which was possibly not intense enough to cause important structural damage and reduce mucociliary transport, as happened with moderate and heavy smokers. Since for the general group of smokers STT was not correlated to PADL level, age, pack/years and years of smoking, it is hypothesized that the MCT in smokers depends more on the current daily cigarette consumption than on smoking history and physical activity level. This hypothesis is in line with what was previously suggested by Stanley et al.,2 although that study did not include a detailed profile of the smoking habits (which the present study does) and did not include regular physical activity as one of its outcomes.
The sample size of this present study is relatively small, particularly after stratification according to daily cigarette consumption. This reduces further sub-analysis and could be considered as a limitation of the study. However, despite the relatively small sample in each group, this stratification was important since it provided relevant results such as the differences between light smokers versus moderate/heavy smokers. Further studies with larger number of smokers with different intensities of cigarette consumption would be welcome. Moreover, the authors used minutes to express saccharin transit time for reasons of clarity, although the specialized literature occasionally reports it in seconds.
In conclusion, specifically in light smokers and non-smokers, better mucociliary function is associated to higher daily physical activity level, as opposed to the decreased mucociliary function observed in smokers i.e., those with moderate and heavy cigarette consumption.
FundingThis work was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), Brazil.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Proença M, et al. Transporte mucociliar e sua relação com o nível de atividade física na vida diária em fumantes saudáveis e não fumantes. Rev Port Pneumol. 2012. http://dx.doi.org/10.1016/j.rppneu.2012.03.003.