Capnometry is a noninvasive method to estimate the partial pressure of carbon dioxide (pCO2) in respiratory gases.1,2 We describe here a case of a 48-year-old woman (who provided consent for using her anonymised data) with nemaline myopathy admitted to our unit. The patient had been undergoing noninvasive ventilation (NIV) for more than twenty years. Because of discomfort following new ventilator settings prescribed at home, she was admitted to the hospital –for readaptation to NIV– presenting with compensated chronic respiratory failure (pH 7.38, PaCO2 63.5 mmHg, PaO2 76.9 mmHg, HCO3 33.6 mmol/L) while on standard oxygen therapy (FiO2 28% via nasal prongs). After a few days, the patient optimised comfort and synchronisation with the ventilator. On day 4, however, she presented with acute-on-chronic respiratory acidosis (pH 7.34, PaCO2 84.3 mmHg, PaO2 73.7 mmHg, HCO3 39.1 mmol/L). The patient, whose Hospital Anxiety and Depression Score was 21 points, reported having taken 2 mg of lormetazepam to manage an anxiety crisis.
Despite the hypercapnia level during the clinical stability phase, the patient could still perform daily moderate respiratory and motor exercises (see below) at home. The recent exacerbation episode posed us the question of whether we can proceed with physiotherapy because of the elevated levels of PaCO2. Resting hypercapnia or pulmonary function tests do not predict hypercapnia during exercise,3 which in some patients may reach elevated values, theoretically putting them at risk. The possible development or worsening of alveolar gas exchange during exercise is usually assessed with a cardio-respiratory test that measures minute ventilation (VE), physiologic dead space (VD/VT), and carbon dioxide output (VCO2). This test is somehow burdensome and has some technical biases when exercise is performed with supplemental oxygen, while capnometry may much easier depict gas derangement during exercise, but it is very seldom used. Indeed, this test is mostly used in COPD patients, while no data is available for restrictive patients.
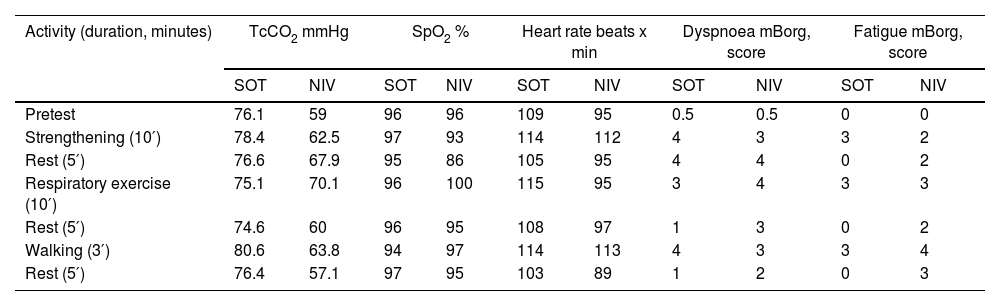
We, therefore, monitored capnometry during the hospital physiotherapy, which consisted of respiratory (chest expansion, breathing control techniques, and inspiratory muscle training) and motor exercises (strengthening and aerobic). The strengthening exercise consisted of active squats of the lower limbs, whereas aerobic activities focused on walking and marching on the spot with alternate arm elevation. The patient exercised at an intensity of 13–14 points (somewhat hard) in the ratings of the perceived exertion scale,4 and each session lasted about 30 min as per patient's tolerance. Transcutaneous CO2 (TcCO2) monitoring (SenTec Digital Monitoring System, Therwil, Switzerland) was executed on two different days under two ventilatory modalities (standard oxygen therapy via nasal prongs and NIV with additional O2) to determine to which extent exercise contributed to a possible increase in hypercapnia. We measured physiological parameters such as oxygen saturation, heart rate, dyspnoea intensity and muscle fatigue (using the modified Borg scale).5 In Table 1, TcCO2 monitoring data and physiological parameters during exercise are listed in detail. These data, taken together with TcCO2, contributed to planning an appropriate exercise programme, suggesting that NIV cycles may contain a further increase in hypercapnia vs standard oxygen via nasal prongs and avoid taking benzodiazepine on exercise days.
TcCO2 monitoring during exercise under two different ventilatory modalities: SOT and NIV.
TcCO2, transcutaneous CO2; SOT, standard oxygen therapy; NIV, noninvasive ventilation; mBorg, modified Borg scale.
This is the first report assessing exercise hypercapnia in a restrictive patient, suggesting that a simple technique such as capnometry can titrate the optimal mode of supporting exercise without applying more complex instrumentation, like during a cardiopulmonary test.
Studies have investigated the use of capnography in patients with COPD and back pain, exploring the possibility of using capnography as a biofeedback, promoting self-regulated breathing.6,7 A critical feature of these studies was the psychological aspect; anxiety and depression were two of the most hidden and impactful complications in patients with COPD. In a case series of 29 patients with back or neck pain, the authors found patients had poor respiratory function as tested with capnography, and all could improve respiratory function with retraining.6
Furthermore, in the CALM project, it has been found that guiding respiratory exercise with real-time biofeedback (capnography) can promote self-regulated breathing, reducing the connections between dyspnoea and anxiety symptoms and targeting breathing efficiency and self-efficacy in COPD.7
In the case described here, we were able to define the optimal exercise modality and suggest the patient adhere to a given protocol to avoid hypercapnia. Transcutaneous capnometry-guided exercise is a promising practice that could simplify and optimise physiotherapy practice in respiratory settings.
The authors received no financial support for the research, authorship, and/or publication of this article.