The aim of this bench study is to compare the standard NIV and nCPAP devices (Helmet, H; Full face mask, FFM) with a modified full face snorkeling mask used during COVID-19 pandemic.
MethodsA mannequin was connected to an active lung simulator. The inspiratory and expiratory variations in airways pressure observed with a high simulated effort, were determined relative to the preset CPAP level. NIV was applied in Pressure Support Mode at two simulated respiratory rates and two cycling-off flow thresholds. During the bench study, we measured the variables defining patient-ventilator interaction and performance.
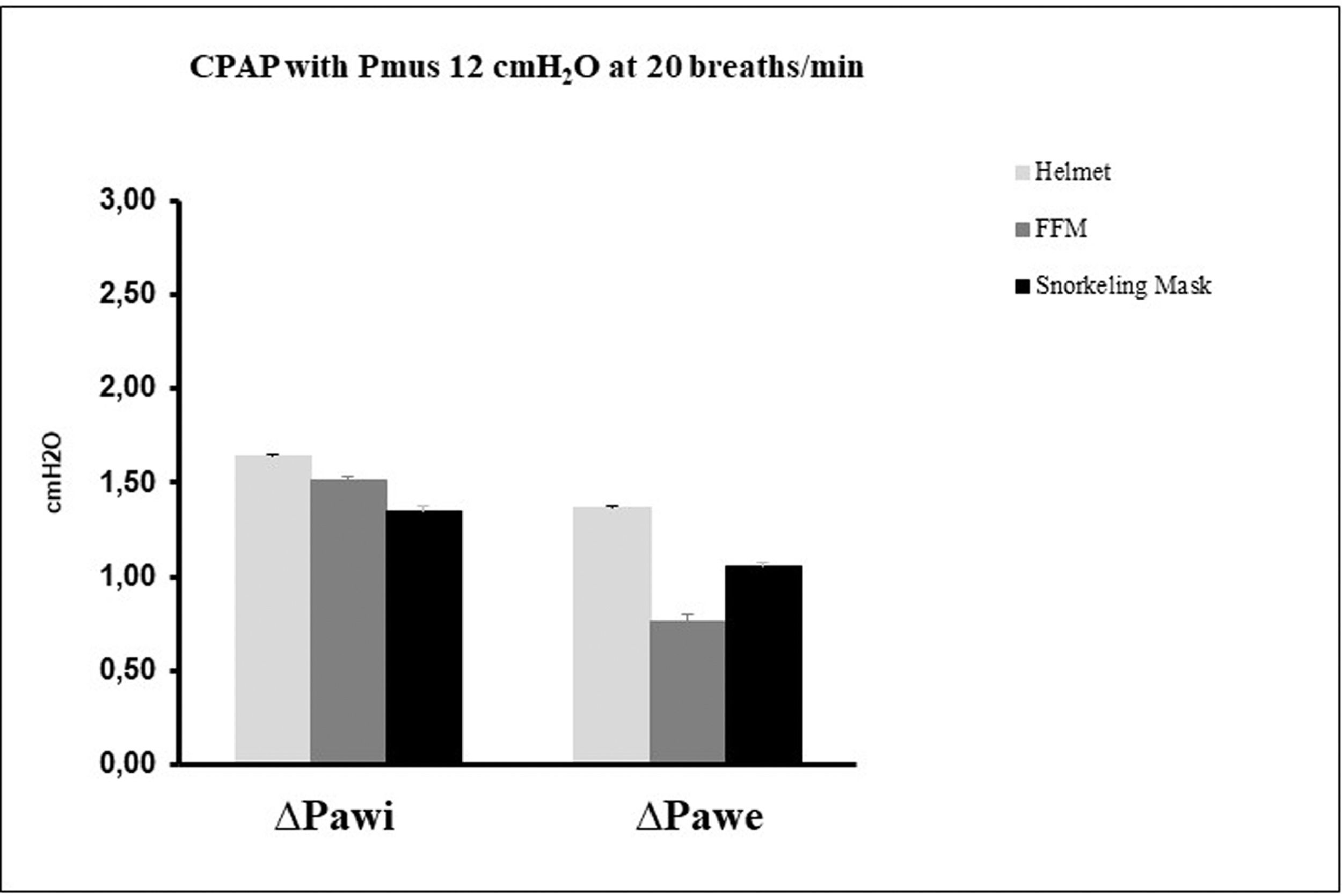
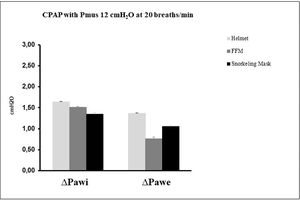
ResultsDuring nCPAP, the tested interfaces did not show significant differences in terms of ∆Pawi and ∆Pawe.
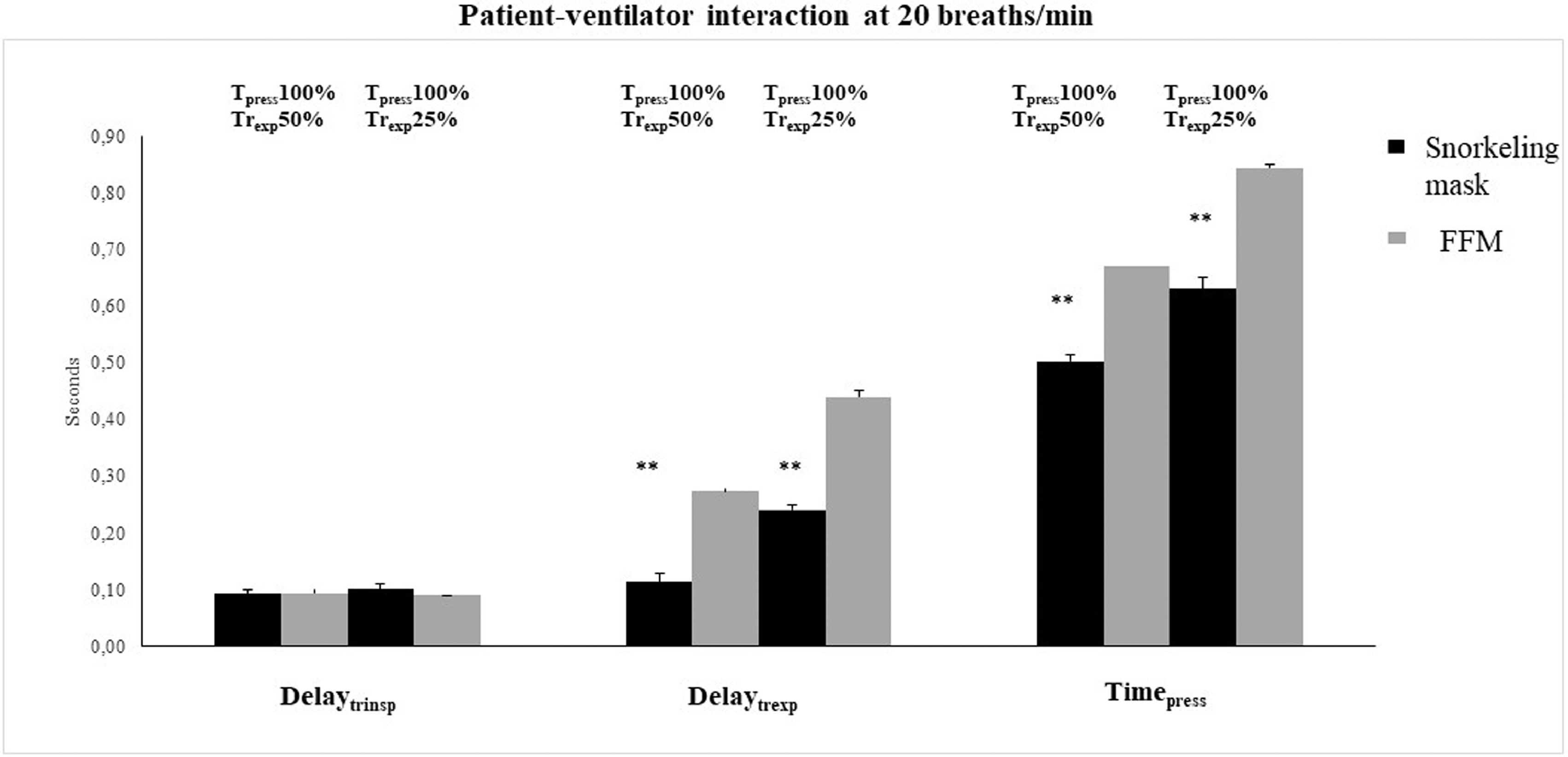
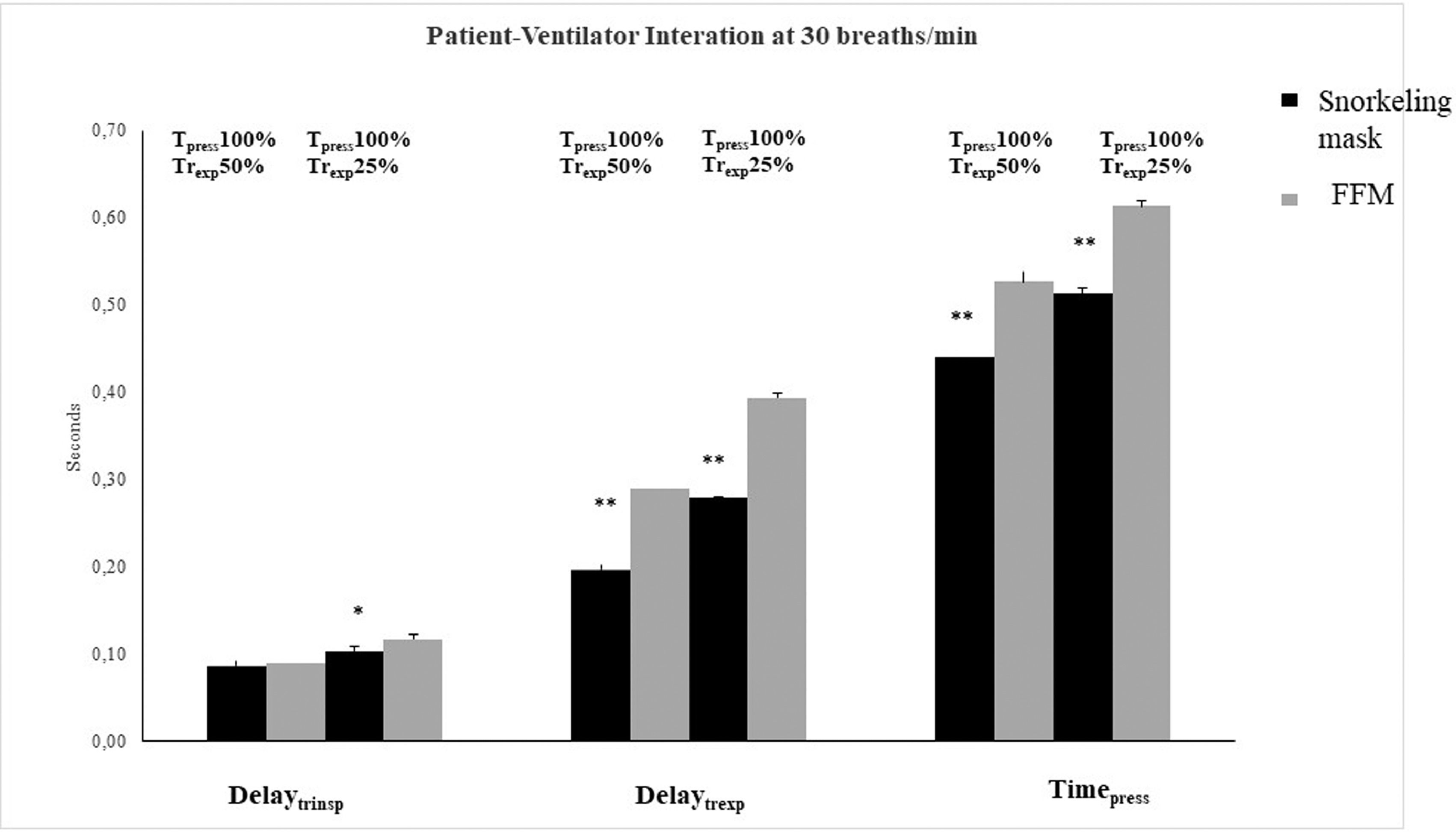
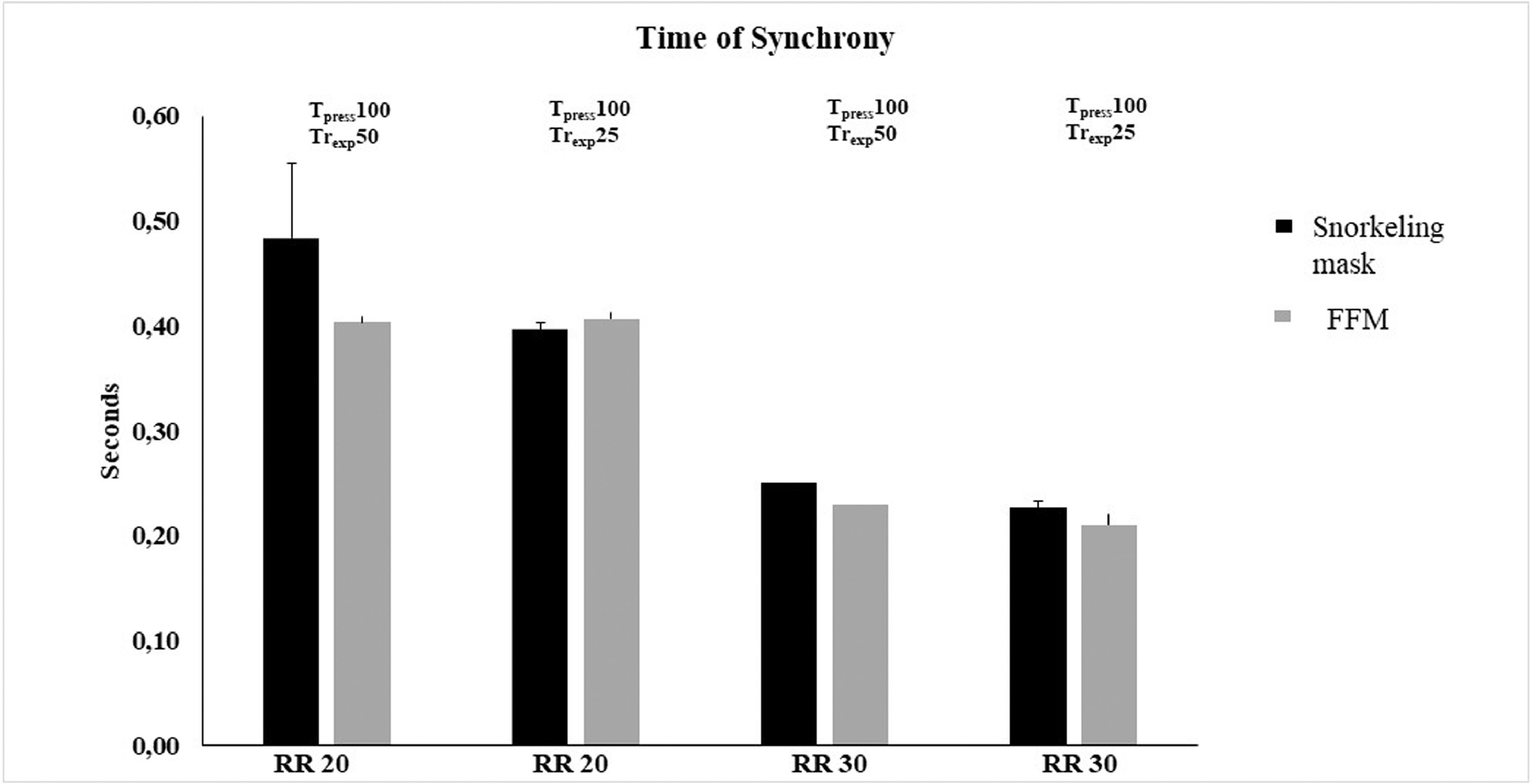
During NIV, the snorkeling mask demonstrated a better patient-ventilator interaction compared to FFM, as shown by significantly shorter Pressurization Time and Expiratory Trigger Delay (p < 0.01), but no significant differences were found in terms of Inspiratory Trigger Delay and Time of Synchrony between the interfaces tested. At RR 20sim, the snorkeling mask presented the lower ΔPtrigger (p < 0.01), moreover during all the conditions tested the snorkeling mask showed the longer Pressure Time Product at 200, 300, and 500 ms compared to FFM (p < 0.01). A major limitation of snorkeling mask is that during NIV with this interface it is possible to reach maximum 18 cmH2O of peak inspiratory pressure.
ConclusionsThe modified snorkeling mask can be used as an acceptable alternative to other interfaces for both nCPAP and NIV in emergencies.
In March 2020, the World Health Organization (WHO) declared the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak a pandemic, due to the increasing number of cases reported worldwide,1 with high rates of hospitalization and ICU admission.2 The high number of SARS-CoV-2 cases initially in Lombardy, and subsequently throughout the whole country, made Italy one of the most affected countries in Europe.3
As happened in March 2020, wherein Lombardy in few days a total of 1593 patients, affected by severe respiratory failure due to COVID-19, were admitted to the ICU,4 out of a total of 1202 ICU beds available,2 the National health care system is now again under pressure from a growing second wave of patients hospitalized or admitted to ICU for acute respiratory failure.
COVID-19 is characterized by a viral interstitial pneumonia5 with fever, dry cough, dyspnoea, and bilateral ground-glass opacities,6 with about 67% of patients evolving to severe pneumonia.7,8
Preliminary reports described that COVID-19 patients, compared to conventional Acute Respiratory Distress Syndrome (ARDS), are characterized by moderate to severe hypoxemia despite a relatively high pulmonary compliance.9,10 Due to the enormous number of COVID-19 patients with acute respiratory failure and to the shortage of ICU beds and ventilators, in many Italian hospital, the management of patients with respiratory failure was entrusted to Non-Invasive Ventilation (NIV) or Non-invasive continuous positive airway pressure (nCPAP).
Several respiratory managements were applied to treat ARDS COVID 19 related. The High flow nasal cannula was used, also as first-line therapy, in Chine, and in USA (although with a high risk of air contamination). The NIV or CPAP were applied in hospitalized patients in China, Italy, and USA with the same proportion (20%, 11% and 19%).11
In particular, in a scenario of a discrepancy between facilities and a large number of casualties, as with COVID-19 pandemic, the application of NIV or nCPAP has been useful as a respiratory supportive strategy, especially in patients with mild to moderate ARDS and a PaO2 to Inspired oxygen fraction ratio (PaO2/FiO2) >150. In our country, the Helmet4,10 has been the most widely used device for non-invasive respiratory support during COVID-19 outbreaks both in general wards and in ICU.10
Unfortunately, a major problem of ventilator and device for NIV shortages rapidly emerged because of the further spread of the virus in other regions of Italy. To relieve the pressure on our National Health System, a device converting a full-face snorkeling mask into a mask for CPAP or NIV has been designed and proposed for clinical use, with the help of 3D printers.
Given the large diffusion of this modified full face snorkeling mask in COVID-19 patients, we designed this bench study to evaluate and compare a helmet, a full-face mask, and a modified full face snorkeling mask in delivering nCPAP and NIV in Pressure Support Ventilation mode (PSV).
MethodsThe study was performed at the Respiratory Mechanics Lab (Ventilab) of the Fondazione Policlinico Universitario A. Gemelli IRCCS, Università Cattolica del Sacro Cuore in Rome, Italy.
Bench studyNon-invasive CPAP and non-invasive positive pressure ventilation delivered in PSV mode were applied to a mannequin (LaerdalMedical AS, Stavanger, Norway) connected to an active test lung system (ASL 5000; Ingmar Medical, Pittsburgh, PA) set using a single-compartment model, an active inspiration simulated by a semi-sinusoidal pressure waveform (Rise Time 15%, Pause 0% and Release Hold 25%) and the following mechanical properties of the respiratory system: resistance 5 cmH2O/l/s and compliance 40 ml/cmH2O. nCPAP was applied via Helmet (H) (CPAP-Castar Starmed, Mirandola, Italy), PerforMax Full face mask (Philips Respironics, Murrysville, PA, USA) (FFM), and a modified full face snorkeling mask (SEA VU DRY, Mares Spa, Rapallo, Italy), while non-invasive PSV was delivered through FFM and snorkeling mask. The Helmet used for this bench study is a transparent latex-free polyvinylchloride hood, joined by a rigid plastic ring to a soft collar and secured by two padded armpit braces at four hooks (two in the front and two in the back of the plastic ring). The helmet used was the size Small to attain a good seal and avoid air-leaks.
The snorkeling mask total internal volume is 1350 ml, but the mouth-and-nose pocket internal volume is only 80 ml, while the FFM internal volume is 500 ml and the H internal volume is 15,000 ml (a real pressurized gas reservoir during inspiration).
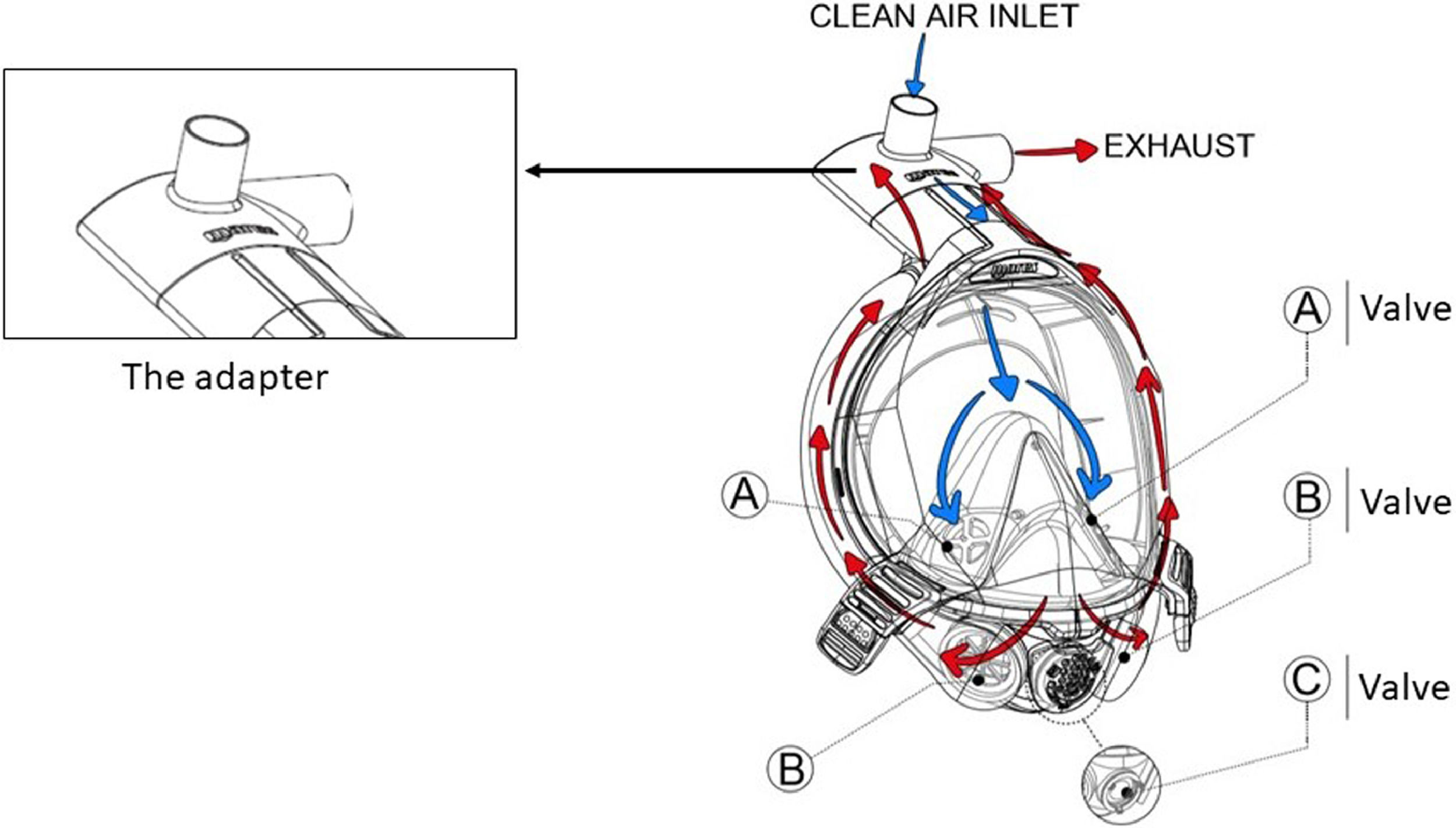
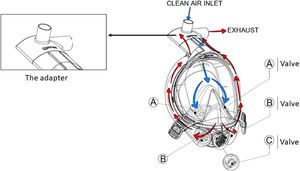
The snorkeling mask differs from Performax full face mask for shape and design characteristic; it presents a complete separation between inspiratory and expiratory circuits with the following main features: hypoallergenic silicone mouth-and-nose pocket connected to a polycarbonate transparent main body; quick-release buckles for easy doffing and a polycarbonate Charlotte valve with an inspiratory and an expiratory channel. See Fig. 1 for details. The snorkeling mask presents two parallel connections with a complete separation between inspiratory and expiratory limbs, while Performax Full face mask is characterized by a single limb connected to the Y piece. The measure of masks used was the medium size for FFM and large size for snorkeling mask to attain a good seal and avoid air-leaks. nCPAP (10 cmH2O) was applied at a simulated respiratory rate (RRsim) of 20 breaths per min (b/min) and a simulated level of inspiratory effort (Pmus) of 12 cmH2O, using a standard CPAP device delivering a flow rate of 60 l/min with reservoir (Drager CF 800 Continous Flow CPAP System; Dragerwerk AG & Co, Lubeck, Germany). During nCPAP test we applied a PEEP valve in the expiratory limb.
Mares snorkeling mask features: presence of two separate limbs; the inspiratory one is highlighted by blue arrows, the expiratory one by red arrows. The adapter created with 3 d printers features two channels: the central upward-pointing channel is the inspiratory channel, the side channel is the expiratory channel.
NIV in PSV mode was delivered at 2 RRsim (20 and 30 b/min) and a Pmus of 12 cmH2O with the mechanical ventilator (Puritan Bennet 840; Covidien Health-Care, Mansfield, MA) set in inspiratory pressure support (iPS) of 10 cmH2O, Positive End-Expiratory Pressure (PEEP) of 8 cmH2O, the fastest rate of pressurization, and a cycling-off flow threshold of 25 and 50% of the peak inspiratory flow. We set the inspiratory flow trigger at the lowest value not determining auto-cycling: this threshold was 5 L/min during all conditions tested. This setting was chosen for comparing the performance of these interfaces under the condition of highest pressurization rate and fast or slow cycling-off criteria.12
MeasurementsAir flow (V′) was measured with a pneumotachograph (Fleish No.1, Metabo, Epalinges, Switzerland), while airway pressure (Paw) was measured by a pressure transducer with a differential pressure of ±100 cmH2O (Digima Clic-1, ICULab system; KleisTek Engineering, Bari, Italy), placed distally from the pneumotachograph. Airflow (V’) and airway pressure (Paw) at the helmet inlet during the inspiratory phase were measured using a pneumotachograph (Fleisch n.2; Metabo, Epalinges, Switzerland) and a pressure transducer with a differential pressure of ±100 cmH2O (Digima Clic-1; KleisTEK, ICU-Lab System, Italy) sited at the distal end of the inspiratory limb of the circuit. When the mannequin was ventilated through the FFM, the pneumotachograph and the pressure transducer were positioned at the Y-connection of the ventilator circuit, instead, when we tested the snorkeling mask the pneumotachograph and the pressure transducer were positioned on the inspiratory channel. All these signals were acquired, amplified, filtered, digitized at 100 Hz, recorded on a dedicated personal computer, and analyzed with specific software (ICU lab 2.3; KleisTEK Advanced Electronic System, Italy and Analysis Plus).
Each trial lasted 5 min; the breaths of the last minute (20 or 30 depending on the trial) were recorded and averaged for analysis.
The measured variables assessed during nCPAP were the maximum inspiratory deflection (∆Pawi, inspiratory drop) and the expiratory peak (∆Pawe), calculated as differences from the preset CPAP level.
During the NIV test, we evaluated the following variables: Ventilator inspiratory and expiratory time (mechanical TI and mechanical TE, respectively), and ventilator rate of cycling were all determined on the flow tracing. The inspiratory duty cycle (mechanical TI/Ttot) was calculated as the ratio between mechanical TI and the total mechanical breath duration (Ttot). Airflow (V′) and tidal volume (VT) delivered to the simulator, airway opening pressure (Paw), and inspiratory muscles effort were displayed online on the computer screen. The signals obtained with the ASL were transmitted to a PC host via 10/100MBit Ethernet, sampled, and processed in real-time by means of specific software (Lab View, Ingmar Medical). The signals obtained with the ASL were integrated with the signals from the ICULab system by using a specific application of the ICULab (ICULab 2.7, KleisTek). The numerical integration of flow over time determined the mechanical tidal volume (mechanical VT). The amount of tidal volume delivered to the simulator during its active inspiration (i.e., the neural tidal volume, VTneu) was calculated as the volume generated from the onset of inspiratory muscle effort negative deflection to its nadir.
Interfaces performance was evaluated using the following parameters12–14:
- 1)
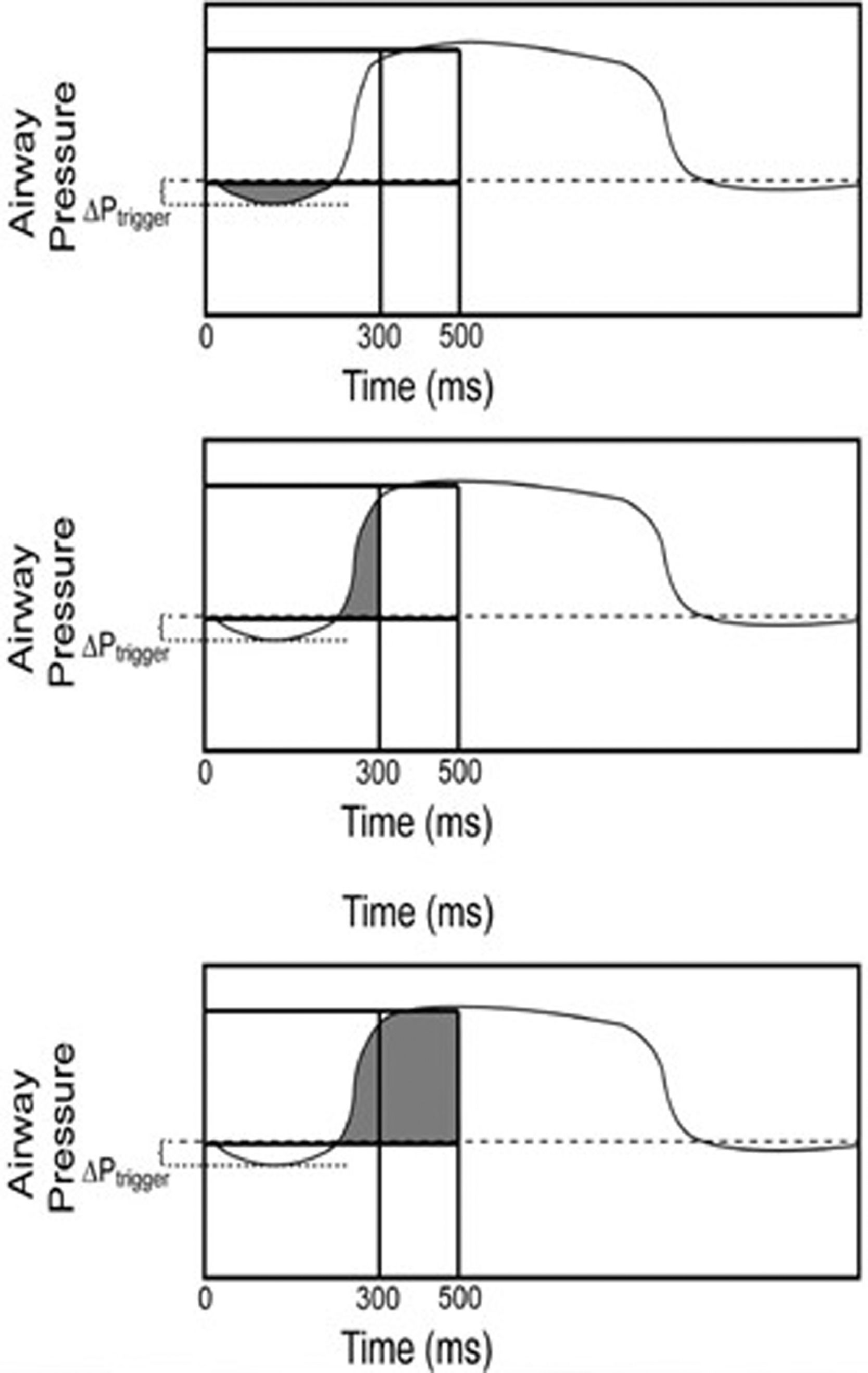
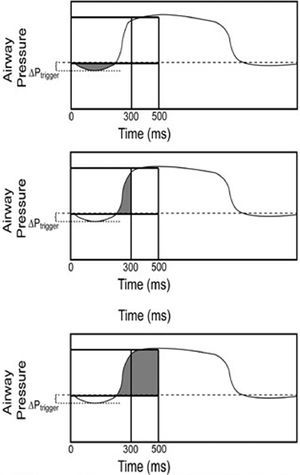
Trigger pressure drop (ΔPtrigger), defined as the pressure swing generated by the simulator inspiratory effort in the airway during the triggering phase; 2) Inspiratory pressure–time product (PTPtrigger), defined as the area under the Paw curve relative to the time between the onset of inspiratory effort and the start of mechanical assistance; 3) pressure-time product at 200 ms from the onset of the ventilator pressurization (PTP200), as the index of pure pressurization performance15; 4)Pressure-time product at 300 ms (PTP300) defined as the integration of Paw over time during the first 300 msec and representing the speediness of the ventilator in reaching the preset level of pressure support; 5) Pressure-time product at 500 ms (PTP500), defined as the integral Paw area over insufflation time from the simulated effort onset, representing the ventilator capability of maintaining the pressurization; 6) PTP500 ideal index, expressed as a percentage of the ideal PTP, which is unattainable because it would imply a trigger pressure drop and an instantaneous pressurization of the ventilator (Fig. 2).
Patient-ventilator interaction was evaluated by determining:
- 1)
Pressurization time (Timepress), defined as the time necessary to achieve the pre-set level of pressure support from the baseline value; 2) Inspiratory trigger delay (Delaytrinsp), calculated as the time lag between the onset of inspiratory muscle effort negative swing and the start of the ventilator support (i.e., Paw positive deflection); 3) Expiratory trigger delay (Delaytrexp), assessed as the delay between the end of the inspiratory effort and the end of the mechanical insufflations (i.e., flow deflection); 4) Time of synchrony (Timesync), defined as the time during which inspiratory muscle effort and Paw are in phase (ideally 100%); 5) SimulatorVT/mechanicalVT, intended as the percentage of VT delivered during inspiratory muscle effort negative deflection; 6) The time during which simulator respiratory effort and ventilator assistance were synchronous, indexed to simulated inspiratory time (Timesync/Tineu) was also computed16–18. 7) Wasted efforts, defined as ineffective inspiratory efforts, not assisted by the ventilator; 8) Auto-triggering, namely a mechanical insufflation in absence of inspiratory effort.
Continuous data were expressed as mean ± standard deviation (SD). Categorical data were presented as numbers and percentages in brackets. All variables were compared with each interface used. Comparisons were made by Student's t-test and Chi test, as appropriate. The analysis of variance (ANOVA) for repeated measures was used to detect significant differences between the different experimental conditions. When significant differences were detected, a post-hoc analysis was performed using the Bonferroni test; p values < 0.05 were considered statistically significant. Statistical analysis was performed using MEDcalc version 18.6.
ResultsAs shown in Fig. 3, during nCPAP, no significant difference in ∆Pawi and ∆Pawe was observed between the three tested interfaces (∆Pawi p = 0.67; ∆Pawe p = 0.10).
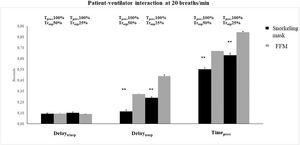
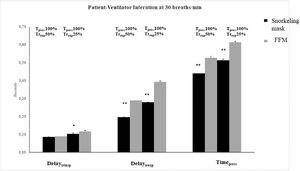
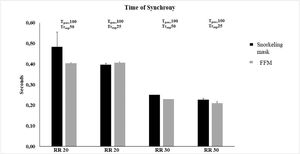
Patient-ventilator interaction described by the measurement of Delaytrinsp, Timepress, and Delaytrexp during NIV delivered through the snorkeling mask and FFM are shown in Figs. 4 and 5. At both RRsim tested and both ventilator settings, the snorkeling mask showed a significantly shorter Timepress and Delaytrexp compared to FFM (p < 0.01). Under all conditions, no significant differences were found in terms of Delaytrinsp, Timesync (Fig. 6), and Timesynch/Tineu between all the interfaces tested. Under all study conditions, the volume delivered with the snorkeling mask was higher than that delivered with the FFM (p < 0.01) (Table 1).
Tidal volume delivered with the different interfaces tested.
VTmech, mechanical tidal volume; VTneu, neural tidal volume; VTneu/VTmech, the percentage of tidal volume delivered during inspiratory simulated muscle effort negative deflection; FFM, respironics PerforMax full face mask; RR, respiratory rates.
The trigger and pressurization performances of the two masks during NIV are shown in Tables 2 and 3. At RRsim 20, the snorkeling mask showed a significantly lower ΔPtrigger than FFM (p < 0.01), while no difference was found at RRsim 30. No significant differences were found in terms of PTPtrigger between the interfaces during all tested conditions.
Performance of the interfaces during NIV at 20 RRsim.
ΔPtrigger, trigger pressure drop; PTPt, pressure time product during the triggering phase; Paw, airway pressure; PTP200, PTP300 and PTP500, pressure time product during the initial 200, 300 and 500 ms from the onset of the ventilator pressurization expressed as the absolute value; PTP500 ideal index, pressure time product during the initial 500 ms from the onset of the simulated effort, expressed as the percentage of the area of ideal pressurization, with different ventilator settings (see text); FFM, respironics PerforMax full face mask; RR, respiratory rates.
Performance of the interfaces during NIV at 30 RRsim.
ΔPtrigger, trigger pressure drop; PTPt, pressure time product during the triggering phase; Paw, airway pressure, PTP200, PTP300 and PTP500, pressure time product during the initial 200, 300 and 500 ms from the onset of the ventilator pressurization expressed as the absolute value; PTP500 ideal index, pressure time product during the initial 500 ms from the onset of the simulated effort, expressed as the percentage of the area of ideal pressurization, with different ventilator settings (see text); FFM, respironics PerforMax full face mask; RR, respiratory rates.
Significant differences in PTP 200, PTP 300, and PTP 500 were found between the snorkeling mask and FFM (p < 0.01) in all conditions tested. The snorkeling mask demonstrated a significantly higher capacity to maintain the pressurization at 200, 300, and 500 ms after opening the inspiratory valve.
In all settings, no asynchrony phenomena were detected with both interfaces.
During the NIV test, with the snorkeling mask it was possible to reach a maximum of 18 cmH2O of peak inspiratory applied pressure. Over this pressure, the presence of air leaks determined important continuous asynchrony phenomena (as continuous auto cycling and double triggering), not modifiable with a change in flow or pressure trigger.
DiscussionIn this bench study, during nCPAP, the interfaces tested showed a similar performance. Instead, during NIV, the snorkeling mask outperformed the FFM for most of the variables considered and in most of the simulated settings.
During the recent SARS-CoV-2 pandemic, early non-invasive respiratory support allowed for the treatment of a large number of patients with respiratory distress to prevent ICU admission. For several reasons, the CPAP application by Helmet represented the first choice of treatment in patients with mild to moderate COVID-19 related ARDS. The Helmet was demonstrated to be an effective alternative to a face mask in recruiting alveolar units and improve hypoxemia. It can also limit air-leaks and room contamination, increasing the patient's comfort and is better tolerated than the face mask, requiring fewer discontinuations.10,19,20 The choice of Helmet as privileged interface applied during treatment of ARDS COVID-19 related is affected by the high diffusibility of SARS-CoV-2 infection. This characteristic of the recent pandemic SARS-CoV-2 infection can increase the level of biological hazard to which healthcare workers are exposed thus requiring the use of personal protective equipment (PPE).21
Unfortunately, the enormous demand for helmet CPAP resulted in a rapid lack of supply, so many laboratories, to try to fill this gap, started to readjust snorkeling masks into devices for respiratory support.
We, therefore, decided to compare the modified snorkeling mask with the Helmet and one of the most popular full face masks (PerforMax full face mask), during CPAP. We applied CPAP at 10 cmH2O because this is a value most commonly applied in this clinical setting.22,23
In our nCPAP bench study evaluation, the snorkeling mask presented a similar performance in terms of ΔPawi and ΔPawe compared to the other interfaces tested.
The snorkeling mask showed stability in maintaining the PEEP level applied during nCPAP.
The snorkeling mask was initially proposed as an alternative to the helmet for CPAP, but during the emergency, it was often used also for NIV. Therefore, we decided to compare this interface with one of the most popular interfaces used in ICU for NIV (FFM). We limited the comparison only to the FFM because, as previously demonstrated by Chiumello et al.,24 in pressure support mode, the mask was more efficient than the helmet. In fact, with the helmet, the initial part of the inspiratory pressure applied is dissipated to pressurize its soft wall. Accordingly, Navalesi et al.25 demonstrated that the helmet significantly worsens patient-ventilator synchrony, when compared to the facemask, as indicated by longer delays between inspiratory muscle effort and support delivery, both at the onset and at the end of inspiration, and by the occurrence of wasted efforts.
Several NIV interfaces, such as Full face mask and Helmet, are characterized by high compliance due to material features that can influence patient-ventilator interaction, and interface performance.
One of the reasons for choosing Respironics mask for this bench study was that this model has relatively low compliance.
For NIV settings, the values of the simulated effort, RRsim, resistance, and compliance, were those already utilized in previous investigations.26,27 The snorkeling mask demonstrated the better simulated patient-ventilator interaction compared to FFM, as shown by shorter Timepress and Delaytrexp. These results are further validated by interface performance data. Probably the better performance underlined by lower ΔPtrigger, and higher PTP 200, 300, and 500 can be explained by the reduced snorkeling mask inner volumes and its materials (Fig. 1). A prerogative of this mask is the presence of two separate limbs. The fresh air enters through the snorkel's central channel, passing the lens, and keeping it fog-free. It then enters the oral-nasal pocket through non-return valves and flows towards the nose and mouth. The oral-nasal pocket's structure guides exhaled CO2 through 4 no-return valves:
- •
2 no-return valves, one each side of the nose, to prevent backward flow,
- •
2 no-return valves at the entrance of the exhalation tubes.
- •
Exhaled CO2 is channeled into the soft silicone side tubes through the second pair of no-return valves. This configuration could explain our results in terms of simulated patient-ventilator interaction and performance devices during NIV settings.
A major limitation of the snorkeling mask must be underlined: during NIV with this interface, it is possible to reach a maximum of 18 cmH2O of peak inspiratory applied pressure. Over this pressure, the presence of air leaks determines continuous asynchronies (as auto cycling and double triggering), not modifiable with a change in flow or pressure trigger. For this reason, our test was limited to single pressure support and PEEP level (PS 10 cmH2O and PEEP 8 cmH2O).
ConclusionThe results of this comparative bench study suggest that this modified snorkeling mask can be used as an alternative to other interfaces for both CPAP and NIV in emergencies. The snorkeling mask can be proposed in the event of a new pandemic surge or for countries where the number of COVID-19 patients is such that all user interfaces for non-invasive respiratory support must be used. Particular attention should be paid to the use of this modified snorkeling mask during NIV, related to the maximum pressure limit of 18 cmH20.
FundingThis study was funded solely by institutional/departmental resources.
The authors are grateful to all ICU doctors, residents, and nurses who fight this COVID 19 pandemic with their efforts and passion.