In 2013 new “mouthpiece ventilation” modes are being introduced to commercially available portable ventilators. Despite this, there is little knowledge of how to use noninvasive intermittent positive pressure ventilation (NIV) as opposed to bi-level positive airway pressure (PAP) and both have almost exclusively been reported to have been used via nasal or oro-nasal interfaces rather than via a simple mouthpiece.
Non-invasive ventilation is often reported as failing because of airway secretion encumbrance, because of hypercapnia due to inadequate bi-level PAP settings, or poor interface tolerance. The latter can be caused by factors such as excessive pressure on the face from poor fit, excessive oral air leak, anxiety, claustrophobia, and patient-ventilator dys-synchrony. Thus, the interface plays a crucial role in tolerance and effectiveness. Interfaces that cover the nose and/or nose and mouth (oro-nasal) are the most commonly used but are more likely to cause skin breakdown and claustrophobia. Most associated drawbacks can be avoided by using mouthpiece NIV. Open-circuit mouthpiece NIV is being used by large populations in some centers for daytime ventilatory support and complements nocturnal NIV via “mask” interfaces for nocturnal ventilatory support. Mouthpiece NIV is also being used for sleep with the mouthpiece fixed in place by a lip-covering flange. Small 15 and 22mm angled mouthpieces and straw-type mouthpieces are the most commonly used.
NIV via mouthpiece is being used as an effective alternative to ventilatory support via tracheostomy tube (TMV) and is associated with a reduced risk of pneumonias and other respiratory complications. Its use facilitates “air-stacking” to improve cough, speech, and pulmonary compliance, all of which better maintain quality of life for patients with neuromuscular diseases (NMDs) than the invasive alternatives. Considering these benefits and the new availability of mouthpiece ventilator modes, wider knowledge of this technique is now warranted. This review highlights the indications, techniques, advantages and disadvantages of mouthpiece NIV.
Em 2013, foram introduzidos novos modos de «ventilação por peça bucal», para ventiladores portáteis disponíveis comercialmente. Apesar disto, há pouco conhecimento sobre como usar a ventilação não invasiva por pressão positiva intermitente (NIV) em oposição à pressão positiva bi-nível (PAP) e ambas têm sido referidas, quase exclusivamente, como sendo utilizadas através de interfaces nasais ou oro-nasais, em vez de através de uma simples peça bucal.
É referido com frequência a falência da ventilação não invasiva, devido à acumulação de secreções nas vias respiratórias, devido à hipercapnia por deficiente ajuste dos parâmetros da PAP ou devido a uma reduzida tolerância à interface. Esta última pode ser causada por fatores como pressão excessiva na face devido a um ajuste defeituoso, fuga excessiva de ar pela boca, ansiedade, claustrofobia e falta de sincronia entre o doente e o ventilador. Deste modo, a interface tem um papel crucial na tolerância e eficácia. Interfaces que cobrem o nariz e/ou a boca (oro-nasal) são as mais habitualmente usadas, mas são as que apresentam maior propensão a provocarem lesões na pele e claustrofobia. A maioria dos inconvenientes associados pode ser evitada usando VNI por bocal. A VNI de circuito aberto por peça bucal está a ser usada por um número significativo de doentes em alguns centros, na assistência ventilatória diurna e como complemento da VNI noturna através de «máscara». A VNI por peça bucal é igualmente utilizada durante o sono com o bucal fixo na posição, através de uma orla de cobertura do lábio. As peças bucais mais utilizadas são as pequenas anguladas de 15 e 22 mm e as de tipo «palhinha».
A VNI através de de peça bucal é usada por um número significativo de doentes como uma alternativa eficaz à ventilação assistida através de tubo de traqueostomia (VTM) e está associada à redução do risco de pneumonias e outras complicações respiratórias. A sua utilização facilita a «acumulação de ar» que aumenta a eficácia da tosse, o discurso e a compliance pulmonar, melhorando a qualidade de vida dos doentes com doenças neuromusculares (DNM) em comparação as alternativas invasivas. Considerando estes benefícios e a disponibilização de modos ventilatórios NIV por peça bucal, é agora garantido um maior conhecimento desta técnica. Esta revisão destaca as indicações, técnicas, vantagens e desvantagens do VNI por peça bucal.
In 1953 Dr. John Affeldt pointed out at a Round Table Conference on Poliomyelitis Equipment, Roosevelt Hotel, New York City, “you can simply attach this (mouthpiece), hang it by the patient, he grips it by his lips, and thus it allows for the excess to blow off which he doesn’t want. It works very well. We even had one patient who has no breathing ability who has fallen asleep and been adequately ventilated by this procedure, so that it appears to work very well, and I think does away with a lot of complications of difficulty of using (invasive) positive pressure. You just hang it by the patients and they grip it with their lips, when they want it, and when they don’t want it, they let go of it.” Thus, intermittent positive pressure ventilation (NIV) via a mouthpiece was used as an alternative to tracheostomy ventilation (TMV) for patients requiring continuous ventilatory support over 60 years ago. Noninvasive ventilation reduces or eliminates the work of breathing (WOB), improves gas exchange, relieves dyspnea, rests inspiratory muscles, and when using mouthpiece interfaces can provide total ventilator support1 and avert endotracheal intubation for some patients during acute exacerbations of chronic obstructive pulmonary disease (COPD),2,3 cardiogenic edema,4 or neuromuscular respiratory muscle failure.5 It can prolong life and preserve quality of life as many patients become continuous NIV (CNIV) dependent without hospitalization.2,5–9 The noninvasive interface, however, must be comfortable and reasonably air tight.10,11 Fortunately, there are now over 100 to choose from. Reports of “NIV” failing and resulting in intubation for as many as 77% of patients are usually caused by inadequate ventilator settings, that is, the use of bi-level PAP at low pressure spans, skin pressure ulcers from continuous mask instead daytime mouthpiece ventilation, and/or failure to use mechanically assisted coughing (MAC) to eliminate airway secretions.5,12 Failure can also occur because of severe bulbar innervated muscle dysfunction, severe cognitive impairment or lack of cooperation, poor pulmonary compliance, severe concomitant lung or airways disease, and administration of sedative medications and/or supplemental oxygen therapy.9,11–20 Thus, appropriate interface selection is crucial for successful NIV.21 Alternating different types of interfaces to change skin pressure points relieves skin pressure difficulties.22,23 While Schettino et al.24,25 have raised concern about potential rebreathing with the total face mask, this is not a problem with open circuit ventilation.
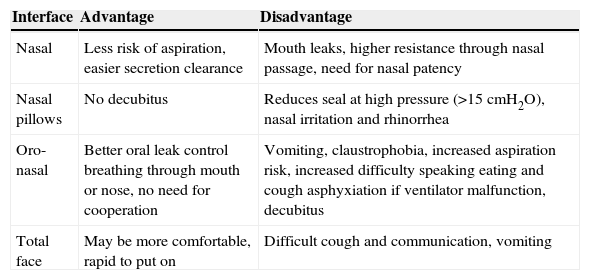
While nasal and oro-nasal interfaces, including nasal pillows types, total face masks, and helmets (Table 1)26,27 are useful for NIV use during sleep and in critical care, they are usually not practical for daytime support. Currently, because mouthpiece NIV is rarely tried, tracheostomy is widely proposed for patients requiring more than nocturnal plus daytime support. Tracheostomy, however, can increase health care costs, complications, has social disadvantages,28 and when given the choice, patients never prefer it to NIV.29
Main advantages and limits of each type of NIV interface.
| Interface | Advantage | Disadvantage |
|---|---|---|
| Nasal | Less risk of aspiration, easier secretion clearance | Mouth leaks, higher resistance through nasal passage, need for nasal patency |
| Nasal pillows | No decubitus | Reduces seal at high pressure (>15cmH2O), nasal irritation and rhinorrhea |
| Oro-nasal | Better oral leak control breathing through mouth or nose, no need for cooperation | Vomiting, claustrophobia, increased aspiration risk, increased difficulty speaking eating and cough asphyxiation if ventilator malfunction, decubitus |
| Total face | May be more comfortable, rapid to put on | Difficult cough and communication, vomiting |
Weakening patients who try to discontinue nasal NIV in the morning eventually continue it into daytime hours to avoid dyspnea. Since this is unseemly, this is the point at which they should be introduced to daytime mouthpiece NIV. Flexed mouthpiece fixed adjacent to the mouth by a flexible support arm are most convenient for air delivery. Many patients used simple mouthpiece NIV around-the-clock since 1953 but then in 1968 the Bennett lipseal came onto the American market.30,31 The Bennett Lipseal fixes the mouthpiece in the mouth for sleep and seals the lips to prevent insufflated air from leaking out of the mouth. Patients reported mouthpiece NIV to be easy to apply, and simple to use during activities of daily living such as eating and speaking.32
Surprisingly, this technology is still not commonly used, and long-term survival for daytime use has not been extensively documented for patients requiring ventilator support 24h a day other than for one center that has published over 500 such cases since 1993.28 There are no evidence-based guidelines for this technique, and the application is based on the experience of only a few centers28,33–36; thus, this review aimed at highlighting the strengths and weaknesses of this method.
Rationale for and difficulties using MPVWhat are the reasons to consider continuous (24h/day) use of NIV rather than tracheostomy for individuals who need full-time ventilatory support? Although tracheostomy is necessary for survival for patients with severe dysfunction of the glottis who have decreased upper airway patency and who aspirate severely it is simply unnecessary for NMD patients without impaired upper airway patency caused by spasticity or collapse of upper airways irrespective of extent of ventilatory failure.34,35
The use of CNIV along with ancillary techniques for expelling airway secretions can avert the need for hazardous endotracheal intubations for many. Translaryngeal as well as tracheostomy tubes, especially with inflated cuffs, can ulcerate tracheal tissues and result in tracheal stenosis, trachiectasis, hemorrhage, fistulae, and perforations. Further, cartilage damage and loss of structural integrity increase tracheal collapsibility (tracheomalacia).37–40 Invasive ventilation is also associated with a high incidence of pneumonia due to the tube and airway colonization with pathogenic bacteria. The tubes also impair mucociliary clearance.41–43Likewise, because of the difficulties associated with CNIV use during waking hours for critical care and long-term users, mouthpiece ventilation via 15 or 22mm mouthpieces (Fig. 1) is the logical, more cosmetic, and comfortable alternative but requires more active participation than the use of facemasks. It has the following advantages:
- (1)
less negative impact on the patient
- (2)
no risk of skin breakdown
- (3)
facilitates speech
- (4)
facilitates eating and swallowing
- (5)
better appearance and
- (6)
is safer by permitting use of glossopharyngeal breathing in the event of sudden ventilator failure or accidental disconnection from the ventilator.
Custom-molded bite-plates have also been constructed for mouthpiece NIV with and without retention straps.28,44 Bach et al. also reported the use of daytime mouthpiece NIV in combination with lipcovering custom-molded orthodontic bite plates for mouthpiece NIV use overnight.27 In one study, mouthpiece NIV was reported for patients with cystic fibrosis and acute and chronic respiratory failure.45 More recently, mouthpiece NIV was reported to be as effective as a full-face mask NIV in reducing inspiratory effort for treating ARF.46
Mouthpieces for daytime use may elicit salivation and long-term use can cause orthodontic deformities after 20–30 years use.26,27 Nasal pledges or nose clips can be used to avoid air leak through the nares for patients using lipcovering interfaces for mouthpiece NIV during sleep.26,27 However, air may also be swallowed and cause gastric distension. Recently, because of the availability of so many self-molding designs, custom-molded bite-plate interfaces have been almost completely abandoned.47
Since mouthpiece and nasal NIV are open systems of ventilator support, the low pressure alarms of ventilators not having mouthpiece NIV modes can often be sound. However, back pressure from a 15mm angled mouthpiece is sufficient to prevent a low-pressure alarm set at 2cmH2O. Assist control mode with a physiological back-up rate is recommended so that every breath triggers supplemental air from the ventilator.48 The patient triggers the breath by placing the mouth on the mouthpiece and creating a small negative pressure in the circuit by sipping or inhaling.48,49 With the “kiss trigger” on mouthpiece mode of the Trilogy ventilator (Philips-Respironics Inc.) all the patient has to do is to touch it for air delivery. No back-up rate is needed for daytime use so no air blows into the patients’ faces.
Types of ventilators for open circuit mouthpiece ventilationVolume cycling of portable ventilators in assist-control mode48–50 both provides ventilatory support and permits air stacking. Pressure cycling in assist control mode, also using active ventilator circuits, can be used as well but does not permit air stacking. Since the patient can take as much of the delivered air as wanted for speech, shouting, eating, coughing, etc., volumes are set from 700 to 1500mL for adult patients.50,51 The mouthpiece can be mounted close to the head so that the patient can grab it as desired.47–49 Air stacking is done by taking multiple volumes without exhaling thereby increasing lung volumes to maintain pulmonary compliance and cough more effectively.28,51,52 Using a volume cycling ventilator the NIV user can air stack independently. In this manner, a NMD patient who has an ineffective cough can often produce a peak cough flow (PCF) sufficient to clear airway secretions as needed.53
Mouthpiece NIV can be used for diseases other than NMDs.54–59 Currently, in Europe, volume-cycling portable ventilators are uncommon. Thus, ventilators usually pressure set and include: the Resmed Elisee 150, Breas Vivo 50 and Resmed VS III with mouthpiece platform. The Philips Respironics Trilogy with its dedicated mouthpiece NIV mode is used with a single active circuit with an exhalation valve (Fig. 2).
Ancillary techniquesLong-term CNIV including mouthpiece NIV cannot be successful without mechanical insufflation–exsufflation (mechanically assisted coughing or MAC) used to increase cough flows for patients with respiratory muscle weakness. The MAC can increase PCF from being negligible and ineffective to over 300L/m to thereby clear the airways of debris and prevent or return oxyhemoglobin saturation to normal levels, thereby averting ARF and intubation or permitting intubated patients and patients with tracheostomy tubes who have little or no ventilator-free breathing ability the possibility of being extubated without undergoing tracheotomy or being decanulated of any tracheostomy tubes.60–62
The clinical evidenceThe most common indication for mouthpiece NIV is for NMD. It was initially used for daytime ventilatory support for ventilator-dependent post-poliomyelitis and NMD patients who were otherwise continuously dependent on iron-lungs in the 1950s and 1960s.50 CNIV has continued to be used by these and other patients in and around the same centers.63,64
In neuromuscular diseasesIn a 1993 study of 257 patients with acute or chronic respiratory failure, NIV via mouthpiece was reported as the predominant ventilatory support during the day and it was used with lipcover phalange for sleep by 163 of the 257 patients. Sixty-one of them had little or no measurable vital capacity.28 In a cohort study, Bach et al. compared 24 patients using NIV (14 of them CNIV dependent with 22 patients using continuous (C) TMV). The CNIV users had significantly fewer hospitalization days per year (d/Y) (2.3±2.4 d/y/patient vs. 0.3±2.4 d/y/patient, p≤0.04) and hospitalizations/year/patient (0.3±0.4 vs. 0.1±0.4).64 In a retrospective study of Gomez-Merino et al., patients with DMD who used CNIV along with a protocol of home management of secretion expulsion by MAC were compared to a group that did not have access to the protocol and were tracheostomized.12 The protocol consisted of using air stacking, mouthpiece NIV for daytime support, nasal NIV for sleep, and MAC to maintain oxyhemoglobin saturation>94% using a pulse oximeter at home. Among the 34 CNIV users with access to the protocol 3 of them died from heart failure and none from respiratory complications. Among the 31 patients who did not have access to the protocol 27 died: 20 from respiratory failure and 7 from heart failure. A consensus statement of the American Thoracic Society on respiratory care in DMD supports this method for preventing and treating acute and chronic respiratory failure.65
A management protocol of NIV with follow-up of 12 years for 23 DMD and 6 post-polio patients was published by Curran et al. with progressive generalized muscle weakness and decreasing vital capacity from an average of 482mL to 336mL the DMD group required an average increase of 0.95h per day of mouthpiece NIV use per year. The average overall survival increased from 19 years and 9 months to 25 years and 9 months with ventilator use in that study but the patients did not have access to MAC.66 Ishikawa et al. demonstrated mean survival to 39.6 years of age for 88 patients with DMD treated with CNIV including mouthpiece ventilation vs. to 28.1 years of age for 21 treated by CTMV.67 Toussaint et al. reported diurnal use of mouthpiece NIV in a regimen of CNIV that improved survival rates in DMD to 88, 77, 58 and 51% after 1, 3, 5 and 7 years, respectively with mean survival to 31 years of age for a total of 184 patient-years.68 More recently, Villanova reported that 19 DMD patients depended on CNIV for a total of 329 patient-years, up to 16 years in one case.69 The patients became CNIV dependent once their VCs had decreased below 297±113ml.69 In 2013 McKim et al. reported prolongation of survival by an average of 5.7 years for 12 DMD patients by CNIV.34
In respiratory failure from other disordersTwenty-nine COPD patients treated with NIV via mouthpiece were matched to 29 patients who received NIV and standard medical treatment. At admission, age, PaCO2, and pH were recorded. The two groups had similar PaCO2 and pH at admission (78.6±12mmHg and 7.30±0.04 mouthpiece NIV group, 79.8±12mmHg and 7.29±0.04 nasal mask NIV group). Mouthpiece NIV use averted need for endotracheal intubation for 27 of the 29 patients and nasal mask NIV for 25 of 29 patients. At the end of the treatment protocol, the PaCO2 was lower in the mouthpiece NIV (62.2±9.6mmHg) compared to the other group (72.4±20.4mmHg, p<0.018). This study shows that in the case of moderate respiratory acidosis, NIV via mouthpiece significantly reduces the need for endotracheal intubation compared with standard medical therapy and can be an alternative to nasal NIV especially when the latter is poorly tolerated.59
One study focused on daytime mouthpiece NIV and nocturnal nasal NIV for a group of 113 adults with cystic fibrosis and chronic respiratory failure and reported probable successfully sustaining life until lung transplantation became available to them.
Mouthpiece ventilation was also compared with facemask ventilation for patients in respiratory failure due to chronic obstructive respiratory diseases and cardiogenic insufficiency. NIV delivered by both facemask or mouthpiece increased pH and lowered paCO2 and averted need for endotracheal intubations.54 Recently mouthpiece ventilation has also been proposed in the treatment of severe sleep related breathing disorders.55–58
Advantages and disadvantages of mouthpiece ventilationThe most important advantage of using a mouthpiece for assisting ventilation is that there is less interference with speech, very little dead space, better appearance, and no need for headgear, thereby eliminating any possibility of claustrophobia. The greatest disadvantage is its limitation to being useful predominantly for waking hours28,47 except when retained by a lip covering interface like the Lipseal or Oracle. Another disadvantage which could limit its use for ARF are nasal leaks,34,46,70 but mouth air leaks can be controlled with a tight-fitting lip seal and nasal pledges or nose clips can be used to avoid air leak via the nares.47,70
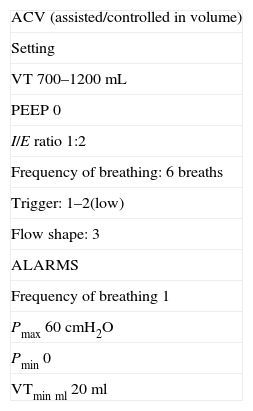
Positive expiratory pressure (EPAP or PEEP) cannot be maintained for patients using open systems of NIV and, indeed, are rarely if ever needed for these patients. Obstructive apneas are relieved by sufficient positive inspiratory pressure delivery. Apnea alarms, when present, should be set at the highest threshold to avoid unnecessary activation and nuisance. The most common ventilator mode used is assist volume-controlled (ACV) with tidal volume between 0.7 and 1.5L with no PEEP (EPAP), low pressure alarm set at the minimum and maximum apnea duration50 (Table 2). Although volume cycling permits air stacking, when gastric inflation is severe, volume cycling is discontinued in favor of pressure cycling. For some patients, a gastrostomy is required so that air insufflated into the stomach can be “burped out” during sleep. Mouthpiece NIV is not successful when patients are uncooperative, cannot access the interface, or when a severe bulbar dysfunction causes aspiration of saliva such that the O2 saturation baseline remains below 95%. It can cause or exacerbate dry mouth. Such patients may benefit from heated humidification or switching to oro-nasal interfaces.
Example of ventilator setting.
| ACV (assisted/controlled in volume) |
| Setting |
| VT 700–1200mL |
| PEEP 0 |
| I/E ratio 1:2 |
| Frequency of breathing: 6 breaths |
| Trigger: 1–2(low) |
| Flow shape: 3 |
| ALARMS |
| Frequency of breathing 1 |
| Pmax 60cmH2O |
| Pmin 0 |
| VTminml 20ml |
VT, tidal volume Pmin, minimal pressure; PEEP, positive end expiratory pressure; VTmin, minimal tidal volume; Pmax, maximal pressure.
Some authors think that tracheostomy is more secure for continuous ventilator support despite significantly longer survival and fewer complications using NIV.35 Daytime mouthpiece NIV in a regimen of CNIV support is a safe and acceptable alternative to CTMV. There is widespread agreement that NIV is preferable to TMV during the early stages of DMD ventilatory insufficiency, but there continues to be widespread ignorance of its benefits over invasive management for continuously dependent patients. The swallowing and speech difficulties associated with tracheostomy are avoided by mouthpiece NIV. Patients with DMD and other NMDs should be offered diurnal NIV via a mouthpiece when nocturnal-only NIV becomes inadequate (Fig. 3). If mouthpiece NIV and MAC are not available at many medical centers,71,72 it can become available by ordering the appropriate equipment and training the staff. Hopefully, this brief review will encourage many such centers to invest in this. It should also be noted that the access to the resources necessary to support patients living at home with TMV vary greatly throughout Europe, so mouthpiece NIV may be especially valuable in countries where these resources are scarce and there is a total or partial lack of respiratory home care services.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
AuthorshipGiancarlo Garuti and Antonello Nicolini planned, drafted and revised the manuscript. Bruna Grecchi, Mirco Lusuardi, João Winck, revised the manuscript. John Robert Bach drafted, and revised the manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare. João Winck is an employee of Linde AG (Medical Director for REMEO).
The authors want to thank Dr. Cornelius Barlascini for his valuable help in revising the manuscript.