Malignant peripheral nerve sheath tumors (MPNSTs) are extremely rare tumors (0,001% incidence in the general population, less than 10% of all soft tissue sarcomas) and, in adulthood, they are associated with neurofibromatosis type 1.1 Primary pulmonary MPNSTs can mimic lung cancer but there are few literature case reports.2,3
A 53-year-old non-smoker male, with no relevant past medical history, went to the emergency department complaining of chest discomfort over several days. The patient had no family history of neurofibromatosis or café-au-lait spots on physical examination. The electrocardiogram and cardiac markers were normal, but the x-ray showed a left hypotransparency. The chest computed tomography (CT) presented a homogeneous spindle-shaped mass (100 × 70 mm), with no signs of invasion of mediastinal structures or lymphadenopathies.
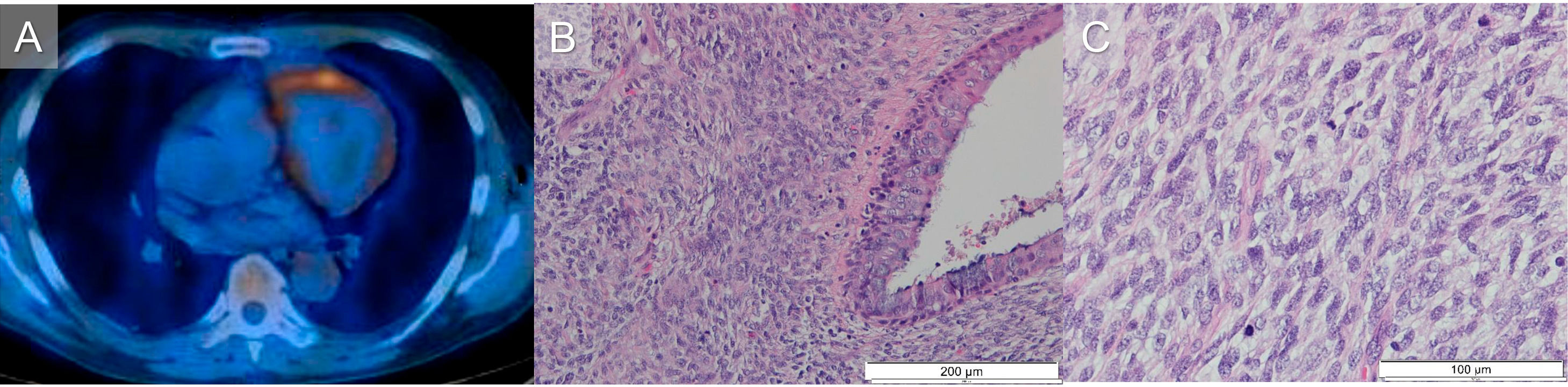
The positron emission tomography (PET) revealed a high accumulation of fluorodeoxyglucose (FDG) in the mass (Fig. 1A). Bronchofibroscopy did not show endobronchial lesions. Two transbronchial lung biopsies were performed: the first one had a small amount of material but revealed a probably neuroendocrine tumor; the second biopsy showed only necrosis. The patient underwent an upper left lobectomy and systematic lymph node dissection by thoracotomy; no evidence of invasion of the thoracic wall was found.
Surgical specimen histology revealed a spindle cell tumor, with infiltration of bronchial structures (Fig. 1B), and atypical neoplastic cells, with frequent mitotic figures (Fig. 1C). On immunohistochemical study, tumoral cells expressed vimentin and B-cell lymphoma 2 (BCL2). There was loss of tri-methylation of lysine 27 on histone H3 protein (H3K27me3) expression in the tumoral cells. Pancytokeratins (AE1-AE3), S100 protein, desmin, cluster of differentiation 34 (CD34) and Melan A were negative. There was no translocation t(x,18). MPNST was the suggested diagnosis.
After 3 months, the patient started chemotherapy (doxorubicin). At this time, he already presented metastatic lesions on the pectoralis major. He died after 3 years, with a hilar mass with invasion of the mediastinum, which caused complete occlusion of the left main bronchus (LMB). In his last two years, the patient was submitted to at least 5 rigid bronchoscopies, for mechanical release, and one prosthesis was placed at the LMB one year before he died.
Immunohistochemical and molecular studies are essential to diagnose of MPNSTs.2,3
MPNSTs are highly invasive, with a low survival rate, but surgery significantly improves disease-free survival.4 Chemotherapy is most used in unresectable or metastatic malignancies, like in our patient, but there are no formal treatment or palliative care guidelines.5 Rare tumors are associated with difficulties in diagnosis and evidence-based treatments are lacking. Therefore, every case is a challenge. Despite being rare, MPNSTs must be kept in mind.
Ethical considerationsWritten informed consent was obtained from the patient guardian for publication of the article.