Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is a very useful tool for the diagnosis and staging of lung cancer.1 This technique is also used for diagnosis of other mediastinal diseases that can be accessed through the airways. The use of EBUS has become widespread in recent years, as it is well tolerated, safe, cost-effective and less invasive that mediastinoscopy and core-needle biopsy. Like all diagnostic tests, EBUS is associated with some complications, the most frequent being puncture site bleeding, pneumothorax and respiratory failure.2 We present a rare case of transbronchial puncture needle breakage during EBUS.
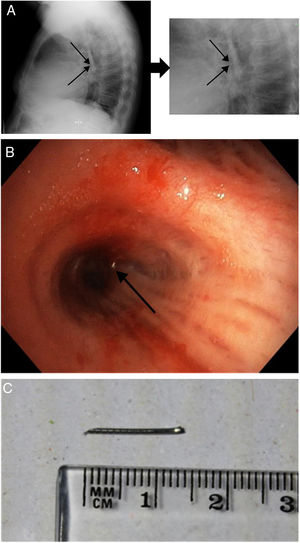
We report the case of a 63 year-old man with a mixed subsolid pulmonary 19-mm nodule (solid component with a ground-glass nodule) in the right lower lobe of the lung and mediastinal adenopathies of significant size [left paratracheal (4L): 13mm; right hiliar (11R): 12mm; and subcarinal (7): 16mm]. During follow-up, all adenopathies remained stable, except for the subcarinal one, which experienced a 5-mm growth (from 11 to 16mm). Positron emission tomography did not show significant enhancement in any of the lesions (SUVmax 3.81). Due to the significant growth of the subcarinal adenopathy, we decided to perform an EBUS under sedation. The procedure was performed using BF-UC180F instrument and a 21G needle (NA-201SX-4021 model). We first punctured the adenopathies located at 7, 4L and 11R level. During the last puncture, real-time ultrasound showed that the distal portion of the needle was placed in the medial wall of the intermediary bronchus and remained motionless despite the proximal portion being extracted. Needle breakage was confirmed on chest X-ray (Fig. 1A) and bronchofibroscopy (Fig. 1B) (which was also used to extract the needle (Fig. 1C)). Histological analysis showed no malignancies. Removal of the pulmonary nodule was high-risk, as the patient had a dilated myocardiopathy with EF 29%. Therefore, we decided to adopt a watchful waiting strategy.
EBUS is a safe technique, with a global rate of complications of 1.4%.2 Within the first 24h, the most common complications include respiratory failure, bleeding, or neumothorax. Thereafter, complications generally are infectious (mediastinitis, sepsis or abscesses). Other potential complications include failure of the working channel or the transbronchial puncture needle.3
The breakage of the needle during EBUS is a rare complication, as only 15 cases were reported in a recent review of a series of 7345 EBUS procedures (0.2%).4 In the first case described,5 the needle broke during the third pass. The needle can be retained inside the adenopathy,6 migrate to a more distal area of the lung or even to another organ.5 Although it can be expelled spontaneously,7 an invasive method may be required when the needle cannot be reached by bronchoscopy. Otherwise, the needle may perforate or migrate to the vascular system or cause chronic inflammation as a response to a foreign object. Only in 7 of the 22 cases reported did the needle break after the adenopathy was punctured [locations 7 (3 patients), 4L (2), 4R (1) and 10R (1)]. The potential causes of needle breakage include7: (1) tangential position of the needle due to the angle required for puncture; (2) harder than usual cartilaginous rings or lymph nodes; (3) manufacturing defects of the needle. To prevent this complication, excessive angulation of the needle should be avoided and its structural integrity should be checked prior to each puncture. The needle can also break and remain retained within the sheath.8 In this case, when the sheath is extracted from the working channel and the stiffening wire is inserted, the broken distal end of the needle will be expelled. Needles generally break prior to the procedure.
The lesson learned from this experience is that, although EBUS is a safe technique, complications – such as transbronchial puncture needle breakage – may arise. The structural integrity of the needles should be checked throughout the procedure and upon completion. The needle must be extracted. If it cannot be recovered by conventional bronchofibroscopy, an invasive method will be required.
AbbreviationsAuthors’ contributionsVR, AG and LV were responsible for the conception and design of the study, and wrote and edited the manuscript. AC contributed to the drafting and revision of the manuscript. All authors read and approved the final manuscript.
FundingThis study was undertaken without funding.
Conflicts of interestThe author has no conflicts of interest to declare.