A clinical case of severe respiratory distress due to a mediastinal bronchogenic cyst (BC) that was managed exclusively by a minimally invasive approach is here presented.
Case reportA 2-year-old boy was referred to the pediatric intensive care unit in acute respiratory distress. He was febrile and presented tachypnea, dyspnea, stridor, global chest retraction and hypoxia. Over the previous 25 days, he had been admitted twice due to cough, wheeze and mild respiratory distress with poor response to medical treatment. Thoracic computed tomography scan revealed a well-circumscribed, bilobed cyst (48 × 46 × 30 mm) in the superior and posterior mediastinum, causing displacement of the supra-aortic vessels, and compressing the esophagus and the trachea; there was a cervical extension, contiguous to the left thyroid lobe and common carotid artery (Fig. 1A, B).
Due to the severe respiratory distress, in an attempt to stabilize the patient condition and improve ventilation, a decision was made to perform percutaneous cyst drainage.
Under ultrasound and fluoroscopic guidance, an 8 Fr pigtail catheter was inserted into the cyst with aspiration of 40 cc of fluid, which resulted in near complete collapse of the cyst and immediate clinical improvement (Fig. 1C). Elective thoracoscopic excision of the mass was then planned.
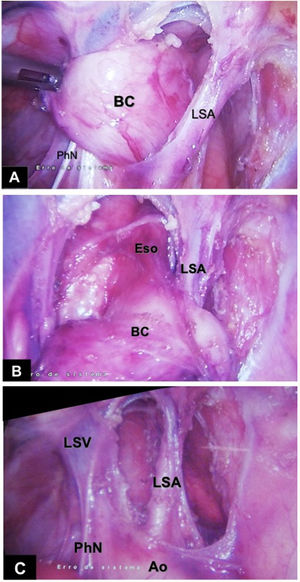
With the patient in modified right lateral decubitus, three 5 mm trocars were inserted. The cyst was identified posterior to the left subclavian artery (Fig. 2A–C); because of the intimate relation with the esophageal wall, an intra-operative upper endoscopy was performed to assist the dissection. The cystic mass was then removed en bloc, the resulting muscle defect of esophageal wall being closed with interrupted absorbable sutures; a thoracic tube was left in place through one port.
The postoperative course was uneventful. After removal of the thoracic tube, the child was discharged home on postoperative day 1. Histological examination revealed a uniloculated cyst lined by respiratory type epithelium with underlying fascicles of smooth muscle, respiratory-type mucous glands and cartilage, consistent with a bronchogenic cyst.
At 2-year follow-up, the child is doing well with no digestive or respiratory symptoms; the scars are almost imperceptible.
CommentForegut cystic malformations are rare congenital entities. Bronchogenic cysts (BC) in the mediastinum form early in fetal development from abnormal buds of tracheobronchial tree. Most of them are asymptomatic in the early stages, thus they are rare in infancy and often recognized in young adults. In fact, most diagnoses occur when the BC become infected or grow large enough to compress adjacent organs.1,2
The treatment of asymptomatic BC is not consensual. In adults, conservative management under close long-term follow-up is an option.3 In children, both symptomatic and asymptomatic cysts should be surgically excised because of risk of enlargement/compression (due to secreting mucosa or infection), erosion/perforation, bleeding, and malignant degeneration. As these lesions do not regress, it is probably more appropriate to resect asymptomatic BC not only in children but also in the young and in the healthy adult in order to prevent life threatening complications such as the present case illustrates.2,3
Drainage of symptomatic BC is a minimally invasive procedure when performed by percutaneous access under ultrasound guidance or by endobronchial ultrasound-guided fine needle aspiration (EBUS-FNA).1,4–6 The latter has been used mainly for diagnostic purpose, but several experts have applied it successfully to BC drainage1,6; unfortunately, there is no bronchoscopy with EBUS-FNA available for young children. Drainage can be used in patients who are nonsurgical candidates, but it is a less than optimal definitive treatment because the risk of infection or cyst recurrence remains. In addition to the rapid resolution of respiratory distress, the drainage should be viewed as a first step to facilitate the subsequent cyst excision due to the reduction of size and inflammation.5
Surgical excision of mediastinal BC is demanding because of vicinity and possible adhesions to surrounding vital organs, with potentially life threatening complications.5,7 In addition, some patients do not tolerate thoracoscopy well, thus thoracotomy is the procedure usually performed.5 Video-assisted thoracoscopic surgery (VATS) has been increasingly used to excise BC and is the preferred “minimally invasive technique” for most thoracic surgeons.1,5 However, a purely thoracoscopic procedure (not VATS) is even less invasive, with a more rapid recovery and better cosmesis. As the present case illustrates, it is viable despite the tight space available, particularly for suturing, a more pronounced issue in young children. So, if the patient can tolerate a “purely” thoracoscopic procedure, it should be endeavored.
In summary, this unique report demonstrates the feasibility of strict minimally invasive techniques to decompress and to excise a BC, which were crucial for the excellent outcome.
Conflicts of interestThe authors have no conflicts of interest to declare.