A 59-year-old woman presented to the Department of Thoracic Surgery with an anterior mediastinal mass detected on routine physical examination. The patient had no respiratory symptoms or signs of myasthenia gravis. The patient did not have a family history of any disease or malignancy. Chest computed tomography (CT) revealed a nodular soft tissue density shadow in the anterior mediastinum of about 21 mm × 14 mm × 11mm. We performed an enhanced CT scan, and in the arterial phase of the enhanced CT we did not see significant enhancement, whereas in the venous phase we could see significant enhancement. With CT values of 27,31 in the plain and arterial phases, 71 HU in venous phase (Fig. 1A–C).
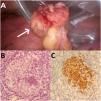
Laboratory examination results showed no abnormalities. Cranial MRI showed no osteolytic changes in the skull. CT of the whole abdomen as well as the results of bone marrow aspiration did not reveal any other systemic involvement. After a multidisciplinary MDT discussion in the hospital, we considered this disease as single-system Langerhans cell histiocytosis(LCH), we then performed a thoracoscopic exploration and resection of the mass (Fig. 2A). The mass was grayish-yellow tissue, with 20 × 15 × 10 mm grayish-white tough areas visible in section, and the rest of the section was grayish-yellow and soft. Histopathological examination led to the diagnosis LCH (Fig. 2B and C) with the following immunohistochemical staining observations: Langerhans cells CD68(+),S-100(+),CD1α(+),CD4(+),Ki-67(3 %,+),CD21(dendritic cells +),P53(60 % of positive cells),CyclinD1(scattered +). Since the patient's pathology was langerhans histiocytosis, we used a fluorescence quantitative PCR method to do genetic testing on her, and the results showed the BRAFV600E mutation(+). At the 1-month postoperative follow-up, the patient's symptoms did not recur.
Surgically removed tissue (arrow, A). Hematoxylin and eosin-stained images showed tumor cell nuclei of renal or coffee bean shape with complex folded nuclear membranes and obvious nucleoli, accompanied by a large number of eosinophilic infiltration(B). Immunohistochemical staining showed that Langerhans' tissue cells express CD1a(C).
LCH is a rare systemic disease characterized by aggregates of CD1a+/Langerin+ LCH cells and widespread organ involvement.1 LCH is more common in children than in adults and is especially rare in adult women.1,2 LCH usually involves the whole body and develops multisystemic disease, the most common sites of involvement being bone and skin,2 whereas in this case it was a case of LCH that involved the thymus alone and was not associated with other malignancies. There are few reports in the literature that LCH involving the thymus isolated has special manifestations on CT images, so it is easy to misdiagnose it as a thymoma. In this case, there was no significant difference in the arterial phase of the CT scan and enhanced CT, but there was significant enhancement in the venous phase, and the CT value was significantly higher. However, in thymoma, there is obvious enhancement in all phases of CT, which may be the imaging differentiation point of potential LCH and thymoma. Confirmation of the diagnosis of LCH requires positive immunohistochemical staining by CD1a, CD207, and S-100 proteins, with CD1a and CD207 being more specific. Positive expression of CD68 has also been reported in the literature and is also suggestive of LCH.2 In this article this patient had the excised pathological tissue immunohistochemically suggestive of CD1a (+), CD68 (+), and S-100 protein (+), consistent with what has been reported in the literature.
Due to the rarity of adult cases of LCH and the patient involvement limited to the thymus, there is currently no established standard treatment protocol available. A study conducted on single-system LCH patients demonstrated that initial treatment was surgical resection alone, and no other treatment, such as chemotherapy, performed, will not progress to multi-system LCH.3 Other research has indicated that for single-system lesions, surgical resection alone yields a favorable prognosis. Despite these promising overall survival outcomes, the development of a safe and effective standardized treatment approach for adult LCH remains an urgent challenge.4
CRediT authorship contribution statementQ. Xu: Data curation, Writing – original draft, Writing – review & editing. H. Tian: Data curation, Writing – original draft, Writing – review & editing. L. Feng: Data curation. L. Li: Data curation. J. Tang: Data curation.
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.