Incidental pulmonary nodules are a diagnostic challenge for both radiologists and pulmonologists.
We report a case of a 47-year-old female, with invasive oral squamous cell carcinoma of the tongue, that presented with multiple bilateral peri centimetric pulmonary nodules revealed on a Cervicothoracic Computed Tomography (CT) scan, requested for tumor staging. The patient underwent hemiglossectomy and was referred to our Pulmonary Oncology clinic.
Clinical evaluation revealed a one-month history of non-productive cough and dyspnea with moderate effort, as well as an exposure to parakeets for about 3 months. She was a non-smoker and denied hemoptysis, recent weight loss, fever, or any other constitutional symptoms. Bronchofibroscopy showed no signs of endobronchial malignancy and bronchial aspirate was amicrobial. Transthoracic biopsy was also performed, which showed a disappearance of dominant nodules, only centrilobular micronodules remaining. Initial diagnosis was of hypersensitivity pneumonitis secondary to aviary exposure and conservative treatment with clinical and imagological surveillance was decided on.
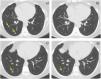
After 9 months, an increase in the size of all the nodules was detected, some now with cavitation (Fig. 1 c). A transthoracic biopsy was therefore proposed, which revealed histologic findings consistent with a benign metastatic leiomyoma (Fig. 2). Subsequently, the patient underwent a total hysterectomy with bilateral adnexectomy, later confirming the diagnosis of uterine leiomyomas. Computer scan images requested 4 months after surgery revealed partial regression of the nodules. The patient remains under follow-up and the lesions were stable at last reevaluation, 2 years after surgery (Fig. 2 c and d).
(a–d): Computed tomography axial images at middle (a, b) and lower lung (c, d) before (a, c) and after hysterectomy (b, d). The patient presented multiple bilateral well-defined and non-calcified lung nodules with a centrilobular distribution (arrows in a; nodules on the left not shown). During follow-up, nodules varied in size, and some developed cavitation (arrow in c). There was no interstitial lung disease, cystic lesions, pleural effusion, or mediastinal lymphadenopathy. After hysterectomy, some nodules completely disappeared (b) and cavitated nodules lost their solid component (arrow in d).
(a–f): Pulmonary nodule transthoracic biopsy - BML lung lesions consist of well-circumscribed nodules ranging in size from few millimeters to several centimeters in diameter.1 These tumors are composed of well-differentiated proliferative smooth muscle cells that form intersecting fascicles, without atypia, necrosis or mitotic figures. The figure shows a pulmonary nodule (a - H&E staining) and immunohistochemical staining. The nodule is positive for SMA (Anti-Smooth Muscle Antibody – b). The cells show positive immunoreactivity toward desmin (figure e) and estrogen receptors (figure d) and have a negative imuunireactivity toward TTF1 (figure c) and CD34 (figure f).
Benign metastatic leiomyoma (BML) is a rare entity of unknown prevalence; a 2017 review reports 161 cases described in the literature between 1 January 1965 to 10 April 2016, only 10 in women who have not undergone prior surgery.1 The first reported case described a patient who died due to extensive pulmonary metastasis later identified as leiomyomas present in the uterus.2
Benign metastatic leiomyoma usually affects women with a history of uterine leiomyomas, metastasizing to extrauterine sites. The most frequent sites of metastasis are the lung and lymph nodes, with the most common presentation being multiple pulmonary nodules composed of smooth muscle cells.3 Benign metastatic leiomyomas have also been detected in the mediastinum, retroperitoneum, vascular channels, bone, heart, skeletal muscle, and soft tissues.3
The diagnosis usually occurs incidentally in a chest radiography, or postmortem. Clinical course is generally indolent and most patients are asymptomatic. However, some may present with cough, wheezing, dyspnea, or chest pain.3,4
The mean age at time of diagnosis is 47 years old.1 BML is more frequent in women who have undergone previous myomectomies or hysterectomies, one of the theories being the possibility of peritoneal seeding at the time of surgery, with subsequent metastasis.1 This theory is not consensual, because there are rare, reported cases in which women did not have a history of uterine interventions. The etiology of the disease remains unknown.
Imaging findings of BLM are nonspecific and overlap with other entities, making the diagnosis by imaging alone almost impossible. On thoracic CT, BML typically presents as multiple bilateral well-defined non-calcified solid nodules of variable size, without a predominant distribution pattern.5 Unilateral or solitary nodules can occur but are less common. Other rarely described features include associated interstitial lung disease, a miliary pattern, cystic lesions, and cavitation.6,7 Uptake on FDG-PET is usually weak or absent7 and there is no associated pleural effusion or mediastinal lymphadenopathy.5
Treatment is not standardized due to the rarity of the disease. Lung tumors may revert after menopause and during or after pregnancy, supporting a role for estrogen in BML pathophysiology.3 Surveillance, oophorectomy or hormonal treatment with antiestrogenic therapy are options described in the literature. Lung lesions usually remain stable, with some cases of regression after treatment.
The presented case is relevant due to the rarity of the disease and the symptomatic presentation, in a patient with a recent diagnosis of a head and neck cancer and no history of previous myomectomies or hysterectomies. The differential diagnosis is broad and includes metastatic disease or a primary lung cancer, and both infectious and non-infectious causes of granulomas (tuberculosis, granulomatosis with polyangiitis, etc.). The recent bird exposure, and the reduction of size of the nodules during follow-up, added the possibility of a subacute hypersensitivity pneumonitis. In this case, the exposure to birds was detected after bronchoscopy, so bronchoalveolar lavage had not been performed. It was a challenging case and is an example of the importance of a multidisciplinary discussion. In high-risk patients for metastatic lung disease, it can be difficult to consider benign causes of multiple lung nodules. Nonetheless, radiologists must be familiarized with BML given that it is associated with a very specific demographic and can be easily included or excluded in a differential.7 It's important to highlight the importance of a thorough clinical history and physical examination even in cases that may seem straightforward at first.
Ethical considerationsWritten informed consent was obtained from the patient for publication of this article.