Remarkable mortality and increasing reports of prolonged morbidity have been observed worldwide since the beginning of the coronavirus disease 2019 (COVID-19) pandemic.1 Hundreds of thousands of individuals have managed to recover from the disease,2 and functional and psychological sequelae in these people have been described in the literature.3 The Post-COVID-19 Functional Status (PCFS) is a simple and rapid self-report scale that allows monitoring of the functional impact of the disease, adding value beyond binary outcomes such as mortality.3 The PCFS was recently validated by Machado et al.,4 who demonstrated its construct validity in a large sample of adults with confirmed or presumed COVID-19. However, so far it is unknown whether this scale is able to discriminate between patients with different characteristics. The aim of the present study was, at the time of hospital discharge following acute recovery from a SARS-CoV-2 infection, to compare fatigue, health-related quality of life (HRQoL) and functional performance between people classified according to the different grades of the PCFS scale. Moreover, predictors of poor functional status were investigated.
This was a cross-sectional study carried out in two Brazilian hospitals; one in Fortaleza-CE and the other in Brasília-DF, after recruiting convenience samples. The study was conducted partially following the protocol for the Life AFTER covid-19 (LATER-19) study (from Australia).5 Inclusion criteria were: individuals over 18 years of age admitted with a confirmed COVID-19 diagnosis and ability to provide informed consent. Individuals with pre-existing conditions that affected the assessment results were excluded (e.g. neuromuscular disorders, mental illness or if they had significant communication or cognitive impairment). All participants provided written informed consent. The study was approved by the Ethics Committees of the recruiting institutions (approval numbers: 4.105.468, 4.324.0069). Participants were recruited to the study between June 2020 and January 2021.
The following variables and outcomes were assessed in this study at the time of hospital discharge: sociodemographic, anthropometric, and clinical characteristics (including self-reported regular physical activity); fatigue symptoms via the Fatigue Severity Scale (FSS),5 HRQoL via the EuroQol 5 dimensions – 5 response level (EQ-5D-5L),5,6 and functional performance via the 1-minute sit-to-stand test (1STS).7 Functional status after COVID-19 was assessed using the PCFS scale, which has four questions to classify each patient into one of five categories with different degrees of functional limitation.3,4
The Shapiro-Wilk test was used to assess the distribution of the data. The chi-square, one-way ANOVA or Kruskal-Wallis tests were used to compare outcomes across the PCFS groups. A logistic regression model with calculation of the odds ratio (OR) and 95% confidence intervals (95% CI) was undertaken to identify the predictors of poorer functional status at hospital discharge (i.e. PCFS grade 3-4). Variables related to the pre-hospitalization period and the hospital length of stay (LOS) were included in the univariate models, and those that reached p<0.20 were subsequently included in the multivariate model. The statistical program SPSS version 22.0 (IBM, Armonk, NY, USA) was used, and the significance level adopted was p<0.05.
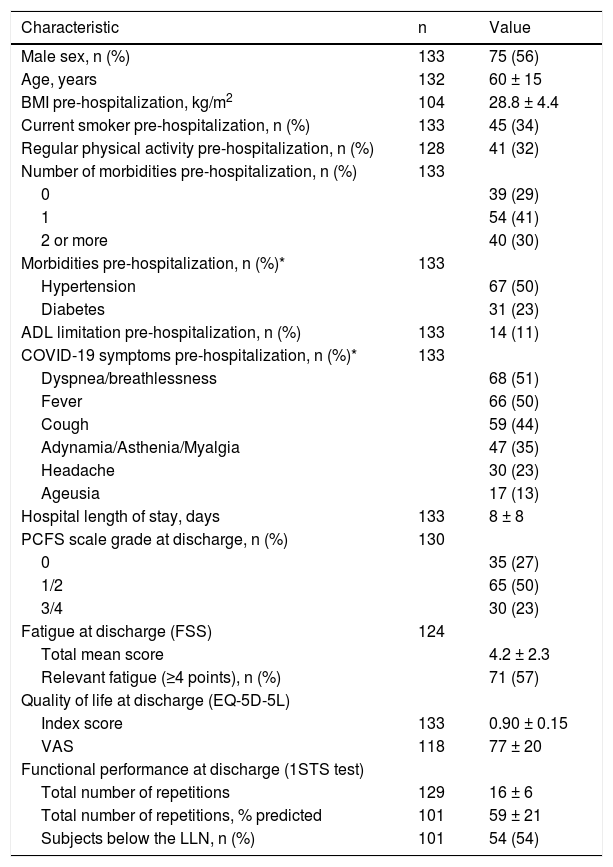
One hundred and thirty-three individuals with a confirmed diagnosis of COVID-19 were included (75 from Fortaleza-CE and 58 from Brasília-DF). Table 1 shows the characteristics of the participants. The mean age was 60 ± 15 years, and they were on average overweight. The majority of the sample had at least one comorbidity, and the most prevalent comorbidities were hypertension (50%) and diabetes (23%). Due to the small number of individuals in each category of the PCFS, participants were divided in three PCFS scale grade groups: (i) grade 0 (no functional limitations), 27%; (ii) grade 1-2 (negligible or mild functional limitations), 50%; and (iii) grade 3-4 (moderate or severe functional limitations), 23%.
Sociodemographic, anthropometric and clinical characteristics, physical and psychological function of participants at hospital discharged following a COVID-19 hospitalization (n=133).
| Characteristic | n | Value |
|---|---|---|
| Male sex, n (%) | 133 | 75 (56) |
| Age, years | 132 | 60 ± 15 |
| BMI pre-hospitalization, kg/m2 | 104 | 28.8 ± 4.4 |
| Current smoker pre-hospitalization, n (%) | 133 | 45 (34) |
| Regular physical activity pre-hospitalization, n (%) | 128 | 41 (32) |
| Number of morbidities pre-hospitalization, n (%) | 133 | |
| 0 | 39 (29) | |
| 1 | 54 (41) | |
| 2 or more | 40 (30) | |
| Morbidities pre-hospitalization, n (%)* | 133 | |
| Hypertension | 67 (50) | |
| Diabetes | 31 (23) | |
| ADL limitation pre-hospitalization, n (%) | 133 | 14 (11) |
| COVID-19 symptoms pre-hospitalization, n (%)* | 133 | |
| Dyspnea/breathlessness | 68 (51) | |
| Fever | 66 (50) | |
| Cough | 59 (44) | |
| Adynamia/Asthenia/Myalgia | 47 (35) | |
| Headache | 30 (23) | |
| Ageusia | 17 (13) | |
| Hospital length of stay, days | 133 | 8 ± 8 |
| PCFS scale grade at discharge, n (%) | 130 | |
| 0 | 35 (27) | |
| 1/2 | 65 (50) | |
| 3/4 | 30 (23) | |
| Fatigue at discharge (FSS) | 124 | |
| Total mean score | 4.2 ± 2.3 | |
| Relevant fatigue (≥4 points), n (%) | 71 (57) | |
| Quality of life at discharge (EQ-5D-5L) | ||
| Index score | 133 | 0.90 ± 0.15 |
| VAS | 118 | 77 ± 20 |
| Functional performance at discharge (1STS test) | ||
| Total number of repetitions | 129 | 16 ± 6 |
| Total number of repetitions, % predicted | 101 | 59 ± 21 |
| Subjects below the LLN, n (%) | 101 | 54 (54) |
Data presented as absolute (relative frequency) or mean ± standard deviation. BMI: body mass index; ADL: activities of daily living; COVID-19: coronavirus disease 2019; PCFS: post-COVID-19 functional status; FSS: fatigue severity scale; EQ-5D-5L: EuroQol 5 dimensions – five response level; VAS: visual analogue scale; 1STS: 1-minute sit-to-stand; LLN: lower limit of normal.
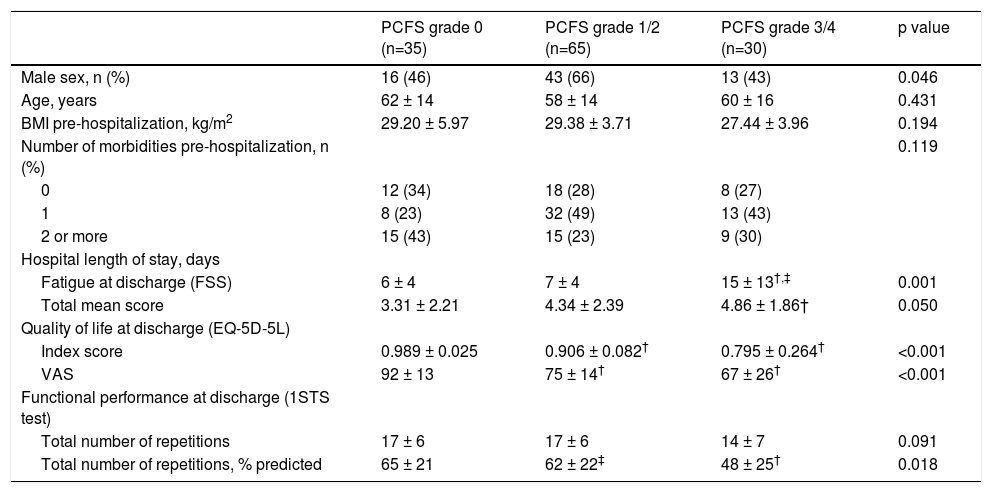
Table 2 shows the comparison of sex, age, body mass index (BMI), number of previous diseases, and hospital LOS across groups according to the PCFS scale. There was a greater proportion of males (66%) in the PCFS grade 1-2 group, and a greater LOS in the PCFS grade 3-4 group. Participants who had a PCFS grade 3-4 presented with more symptoms of fatigue, poorer HRQoL and worse functional performance than those with PCFS grade 0. In addition, participants with PCFS grade 1-2 reported poorer HRQoL than those with PCFS grade 0, and better functional performance than those with PCFS grade 3-4. The following variables were identified as potential predictors of poorer functional status (i.e. PCFS 3-4) in univariate models: sex, physical activity status, diabetes before hospitalization, and hospital LOS. In the multivariate model, only the hospital LOS remained a statistically significant predictor (OR 1.17 [95% CI 1.07 – 1.27]).
Comparison of sociodemographic, anthropometric and clinical characteristics, physical and psychological function between Post-COVID-19 Functional Status scale grades in participants at hospital discharged following a COVID-19 hospitalization (n=133).
| PCFS grade 0 (n=35) | PCFS grade 1/2 (n=65) | PCFS grade 3/4 (n=30) | p value | |
|---|---|---|---|---|
| Male sex, n (%) | 16 (46) | 43 (66) | 13 (43) | 0.046 |
| Age, years | 62 ± 14 | 58 ± 14 | 60 ± 16 | 0.431 |
| BMI pre-hospitalization, kg/m2 | 29.20 ± 5.97 | 29.38 ± 3.71 | 27.44 ± 3.96 | 0.194 |
| Number of morbidities pre-hospitalization, n (%) | 0.119 | |||
| 0 | 12 (34) | 18 (28) | 8 (27) | |
| 1 | 8 (23) | 32 (49) | 13 (43) | |
| 2 or more | 15 (43) | 15 (23) | 9 (30) | |
| Hospital length of stay, days | ||||
| Fatigue at discharge (FSS) | 6 ± 4 | 7 ± 4 | 15 ± 13†,‡ | 0.001 |
| Total mean score | 3.31 ± 2.21 | 4.34 ± 2.39 | 4.86 ± 1.86† | 0.050 |
| Quality of life at discharge (EQ-5D-5L) | ||||
| Index score | 0.989 ± 0.025 | 0.906 ± 0.082† | 0.795 ± 0.264† | <0.001 |
| VAS | 92 ± 13 | 75 ± 14† | 67 ± 26† | <0.001 |
| Functional performance at discharge (1STS test) | ||||
| Total number of repetitions | 17 ± 6 | 17 ± 6 | 14 ± 7 | 0.091 |
| Total number of repetitions, % predicted | 65 ± 21 | 62 ± 22‡ | 48 ± 25† | 0.018 |
Data presented as absolute (relative frequency) or mean ± standard deviation. COVID-19: coronavirus disease 2019; PCFS: post-COVID-19 functional status; BMI: Body mass index; FSS: fatigue severity scale; EQ-5D-5L: EuroQol 5 dimensions – five response level; VAS: visual analogue scale; 1STS: 1-minute sit-to-stand.
This study showed that the PCFS scale is a simple and rapid self-report instrument which is valuable for discriminating between groups with various physical and psychological health outcomes. In addition, variables that could predict a poorer functional status and potentially, the need for rehabilitation at the time of hospital discharge, were identified.
Machado et al.4 also compared the EQ-5D-5L scores and the intensity of fatigue symptoms between PCFS grades and observed similar results. However, functional performance was not investigated in their study.4 Our study supports the validity of the PCFS scale by showing that individuals in higher PCFS grades showed a lower 1STS (expressed as % predicted) than those in lower grades. The fact that there was no significant difference in functional performance at discharge when assessed by the 1STS test total number of repetitions, but there was a significant difference when using the 1STS test % predicted, can be explained by the larger proportion of male subjects in the group of participants with PCFS grade 1/2. This larger proportion of males might have led to a greater number of 1STS repetitions in this group, which prevented the comparison of total number of repetitions to reach statistical significance. Another study suggests that the PCFS tracks responses to pulmonary rehabilitation, as six out of 10 patients with perceived restrictions due to COVID-19 at baseline showed no restrictions (i.e. PCFS 0) in the post-rehabilitation assessment.8
We also confirmed that LOS was the only predictor of a higher PCFS grade and reduced function at hospital discharge in a multivariate model. That is, our findings suggest that an increase of one day in hospital LOS is associated with a 17% increased risk of presenting with poor functional status at the time of hospital discharge. Our findings also reinforce the compounding influence of COVID-19 severity and detrimental impact of increasing duration of hospitalization on the patient's functional status, and further highlight the importance of applying preventive interventions such as early mobilization. The main limitations of this study are the cross-sectional design, which prevents a cause-and-effect analysis, the small sample size from only two centers, and the absence of a non-hospitalized group. Moreover, we were not able to characterize the sample regarding the type of treatment received during hospitalization (e.g. mechanical ventilation). Future studies including the repeated application of the PCFS after discharge are warranted to determine, define and compare the duration to functional recovery after COVID-19 and similar illnesses resulting in hospitalization.
In conclusion, the PCFS scale was demonstrated to be a discriminatory instrument for groups with measured varying degrees of fatigue, HRQoL, and functional performance. In addition, hospital LOS was the only predictor of a poorer functional status at hospital discharge.
No funding.