João Santos Silva contributed in elaboration of the idea and study design, data base creation, manuscript writing and revision. Ana Rita Costa contributed to the database creation and gathering data. Paulo Calvinho contributed in elaboration of the idea, manuscript revision and supervision.
First described in 1959 by Carlens,1 mediastinoscopy has been the gold standard in lung cancer staging and evaluation of mediastinal lymphadenopathies.2,3
Recently endobronchial (EBUS-FNA) and endoscopic (EUS-FNA) ultrasound guided biopsy with fine needle aspiration have been gaining popularity as an alternative.
The need to assess the quality of our department's performance motivated this paper; this is a report on our ten-year experience and aims to demonstrate the safety and diagnostic accuracy of mediastinoscopy and compare with the literature.
A retrospective study was performed after including all patients who underwent mediastinoscopy in our institution from January 2006 to November 2017 – 430 cases. 41 patients were excluded due to lack of records.
Videomediastinoscopy was introduced at our institution in early 2008. Before that period we report 41 mediastinoscopies performed by classic methods.
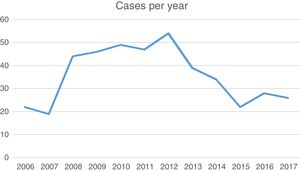
Patient characteristics are reported in Table 1 and yearly distribution in Fig. 1.
Indications were staging of lung cancer and evaluation of mediastinal lymphadenopathies or mass. Lymph nodes tissue was obtained from all patients except two cases of inaccessible mediastinum due to fibrosis. Staging mediastinoscopy was performed accessing routinely stations 4R, 7 and 4L, with two or more stations biopsied in 93.9% of cases. Diagnostic mediastinoscopy was performed as indicated by the suspected pathology.
Average hospital stay was 1.3 (±1.9) days, with 88% discharged on day 1 postoperative. No outpatient-based procedures are performed at our institution.
Complications occurred in 7 patients (1.8%) and 3 died (0.8%), as Table 2 describes.
.
| Complications | Patients (n) | (%) |
|---|---|---|
| Morbidity | ||
| Bleeding requiring sternotomy | 4 | 1.0 |
| Wound infection | 0 | 0 |
| Traqueal injury | 1 | 0.25 |
| Transient laryngeal nerve injury | 4a | 15.4a |
| Permanent laryngeal nerve injury | 0 | 0 |
| Unexpected readmissions | 0 | 0 |
| Mortality | ||
| Postoperative | 3 | 0.8 |
| After discharge | 0 | 0 |
aDue to lack of digital records, data referring only to year 2017.
176 patients underwent diagnostic mediastinoscopy. Most common histopathological results were granulomatous disease (52%) and metastatic carcinoma (20%).
213 patients underwent mediastinoscopy for lung cancer staging. 41 had positive and 172 negative lymph nodes. 25 patients (11.7%) were excluded due to loss in follow-up, exploratory thoracotomy or neoadjuvant chemotherapy for local invasiveness. The remaining 147 patients underwent lung resection surgery with systematic lymph node dissection, on average, 22 days (1–68) after mediastinoscopy.
The overall incidence of false negative mediastinoscopy was 6.8% (10/147). Sensitivity of mediastinoscopy was 80.39% (95% CI, 66.88–90.18%) and negative predictive value was 93.20%. Accuracy was 94.68%.
Nowadays, the popularity of mediastinoscopy is declining due to the increase in EBUS and EUS-FNA. However, revised guidelines for preoperative mediastinal lymph node staging by European Society of Thoracic Surgeons state that EBUS/EUS-FNA is the first option in experienced centers due to its minimal invasiveness and its sensitivity to ruling out mediastinal disease but mediastinoscopy is indicated when negative in patients with suspected N2/N3 disease.4
Several studies confirm sensitivity up to 95% with EBUS to confirm mediastinal disease,5 however other studies reveal false negative rates as high as 16%.3 Regarding complications, rates as low as 0.15% in dedicated centers are reported but up to 1.23% in the community.6
However, the number of EBUS/EUS is expected to rise and the decrease we have witnessed in the number of mediastinocopies performed in our center since its peak in 2012 may be due to this. Fewer mediastinocopies may jeopardize the quality of training programs and safety rates may worsen.
In our country, EBUS is performed by pulmonologists, EUS by gastroenterologists and mediastinoscopies by thoracic surgeons and the decision to perform a mediastinoscopy may be biased by the accessibility to the preferred method by thoracic oncology teams. Surgical teams offer mediastinoscopy when there is no possibility of arranging an EBUS in time.
In our study we conclude that mediastinoscopy is safe with 1.8% complication rate and 0.8% mortality rate, comparable with larger series reporting complication rates of 1.3–3.7% and mortality rates of 0–0.6%.2,7
False negative rate was 6.8%, comparable with larger series results of 5.5–8.8%.2,7 Sensitivity was 80.39%, comparable to rates of 85–89.8% in larger series.2,7
In terms of limitations, our study was retrospective. Secondly, comparison with pre-operative imaging like CT scan or PET/CT was beyond the scope of this article. Also, PET/CT was introduced in clinical practice at our institution in 2015, and only a small part of our cohort had previously had PET/CT scan. Thirdly, results were not compared to EBUS or EUS because it is done in a different institution and access to records is limited. Most centers in Portugal are performing EBUS alone and are not certified centers, and waiting times are variable. The choice of mediastinal invasive staging remains a matter of preference of oncology teams.
In conclusion, we believe mediastinoscopy will remain a tool of extreme value and an everyday practice in most thoracic surgery centers in our country which should be mastered by any dedicated thoracic surgeon. The results reported, comparable to other published series, prove mediastinoscopy to be safe and accurate.
International studies report similar rates with EBUS/EUS in mediastinal staging for lung cancer and we strongly encourage further studies comparing our results with other less invasive modalities. Furthermore, the role of EBUS/EUS in diagnosis of mediastinal adenopathies is even less studied.
Conflicts of interestThe authors have no conflicts of interest to declare.