The six-minute walk test (6MWT) distance could facilitate the assessment of cardiorespiratory fitness (CRF) in clinical practice as recommended. We aimed to develop a CRF classification using the 6MWT distance in asymptomatic adults considering the treadmill maximum oxygen uptake (V˙O2max) as the gold standard method.
MethodsWe evaluated V˙O2max and 6MWT distance in 1295 asymptomatic participants aged 18–80 years (60% women). Age- and sex-related CRF was classified based on the percentiles as very low (<5th percentile), low (5th–25th percentile), regular (26th–50th percentile), good (51st–75th percentile), excellent (76th–95th percentile), and superior (>95th percentile) for both V˙O2max and 6MWT distance. We investigated the 6MWT distance cut-off (%pred.) with the highest sensitivity and specificity for identifying each V˙O2max classification.
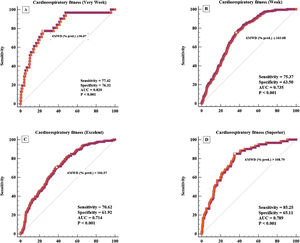
ResultsV˙O2max declined by 8.7% per decade in both men and women. The 6MWT distance declined by 9.3% per decade in women and 9.5% in men. We formulated age- and sex-related classification tables for CRF using the 6MWT distance. Moreover, the 6MWT distance (%pred.) showed excellent ability to identify very low CRF (6MWT distance ≤ 96%; AUC=0.819) and good ability to differentiate CRF as low (6MWT distance=97%–103%; AUC=0.735), excellent (6MWT distance=107%–109%; AUC=0.715), or superior (6MWT distance>109%; AUC=0.790). It was not possible to differentiate between participants with regular and good CRF.
ConclusionThe CRF classification by the 6MWT distance is valid in comparison with V˙O2max, especially for identifying adults with low CRF. It could be useful in clinical practice for screening and monitoring the cardiorespiratory risk in adults.
It has been recommended that cardiorespiratory fitness (CRF) should be considered as a vital sign in cardiovascular health assessment.1,2 The gold standard for CRF expression is the maximum oxygen uptake (V˙O2max) obtained at the end of a cardiorespiratory exercise testing (CPET). In low-resource environments, submaximal and field exercise tests or even CRF estimates should be implemented.1,2 Despite consistent evidence on its relevance, the CRF evaluation has not yet been incorporated as a routine test for cardiovascular risk assessment in clinical practice.2
Field tests are performed when neither sophisticated equipment for direct assessment of V˙O2max nor human resources with a high level of training are available. Among the most appropriate field tests for individuals at higher cardiovascular risk and controlled chronic diseases is the six-minute walk test (6MWT). The 6MWT has been validated in several populations, including asymptomatic individuals,3 and a 6MWT distance has been proven to adequately predict the V˙ O2max obtained in the laboratory.4–6 This characteristic makes the 6MWT a simple and less costly CRF assessment tool. In addition, this test is more representative of activities of daily living than other walking tests.3,4
Tables of normalcy and specific V˙O2max prediction equations could facilitate the use of CRF assessment as a routine test for screening cardiovascular risk in clinical practice. Accordingly, simple field tests that require minimal resources to be performed and equations for the prediction of V˙O2max are essential for the inclusion of CRF evaluation in different clinical settings.1
We hypothesized that the 6MWT is valid for classifying CRF compared to the gold standard (V˙O2max), thereby appropriately identifying adults with low CRF. Accordingly, we aimed to develop a CRF classification table using the 6MWT distance in asymptomatic adults considering the treadmill V˙O2max as the gold-standard criterion. We also evaluated age- and sex-related changes in CRF and the correlation between the 6MWT distance and V˙O2max.
MethodsSample and recruitmentEligible participants were adults over the age of 18 years with no evidence of a self-reported previous medical diagnosis of cardiopulmonary disease, locomotor disorders, electrocardiographic abnormalities at rest or on exertion, or other problems that prevented them from performing physical exercises safely. We recruited participants through social networks, posters at regional universities, and local print media. We excluded participants who presented with spirometry suggesting obstructive ventilatory disturbance (forced expiratory volume in 1s [FEV1]/forced vital capacity [FVC]<0.75), who had severe arrhythmias at rest that could potentially be lethal during CPET, and who presented signs and/or symptoms and stress electrocardiography suggestive of myocardial ischemia. The results suggesting poor effort or operational problems during the CPET were excluded from the study. The ethics committee of our university approved this study (#186.796). All participants signed an informed consent form prior to participation.
Clinical and sociodemographic evaluationBaseline assessments included participants' age, sex, and the presence of self-reported main risk factors for cardiovascular diseases, including older age (≥45 years for men and ≥55 years for women), systemic arterial hypertension, diabetes mellitus, dyslipidemia, current smoking habits, medication use, and a family history of premature coronary heart disease. We also assessed the participants’ physical activity level in daily life using validated triaxial accelerometers (ActiGraph GT3X+, MTI, Pensacola, FL)7–9 as previously described.10 The participants completed seven consecutive days of assessment during waking hours. To be considered valid, it was necessary to have at least ten hours of continuous monitoring, starting from the moment of awakening. The participants used the accelerometer until bedtime, except during the shower and aquatic activities. We considered physically inactive participants to be those with less than 150min of moderate-to-vigorous physical activity or less than 75min of vigorous physical activity per week.11,12
Anthropometric assessmentBody mass and height were measured on a calibrated digital scale with a stadiometer (Toledo Prix 2096PP, Brazil). We calculated the body mass index (BMI) in kg/m2 and defined obesity as a BMI≥of 30kg/m2. We also measured waist and hip circumferences with a non-extensible tape using previously standardized methods.13
SpirometryA forced vital capacity maneuver with a calibrated spirometer (Quark PFT, COSMED, Pavonadi Albano, Italy) was performed according to the criteria established by the American Thoracic Society.14 We quantified the FEV1, FVC, and FEV1/FVC ratio. For those who had FEV1/FVC<0.7 on pre-bronchodilator spirometry, we conducted forced spirometry 15min after the patient inhaled 400μg of salbutamol.15,16
Cardiopulmonary exercise testingFollowing a ramp protocol, we performed CPET on a treadmill (ATL, Inbrasport, Curitiba, Brazil), with individualized speed and inclination increases based on the estimated V˙O2max.9 Metabolic, cardiovascular, and ventilatory responses were measured breath-by-breath using a gas analyzer (Quark PFT, COSMED, Italy). We performed the same altitude, atmospheric pressure, and temperature tests, and a cardiologist supervised all the tests. Oxygen uptake (V˙O2) breath-by-breath was measured and the average V˙O2 was calculated every 15s. The arithmetic average of V˙O2 in the last 15s at the end of the test, just before the recovery phase, was considered representative of V˙ O2max. Maximum effort was defined as a maximum heart rate above 85% of the predicted value (220 – ageyears) and gas exchange rate (V˙CO2/ V˙O2)>1.0. CPET was conducted with continuous monitoring of the electrocardiogram.
Six-minute walk testWe performed the 6MWT according to the guidelines of the American Thoracic Society and European Respiratory Society.3 Since the literature suggests no learning effect of the 6MWT in apparently healthy individuals, we conducted only one test in the present study.17 We instructed individuals to walk the maximum distance possible for six minutes on a 30m long, flat, and straight corridor indoors. Two traffic cones indicated the route, and the hallway was marked every 3m. Standardized instructions and verbal encouragement were provided to the participants every minute. We registered the 6MWT distance in meters and the percentage of the predicted values.17
Statistical analysisWe performed a descriptive analysis of the data presented as mean±standard deviation for continuous variables and frequencies and percentages for categorical variables. We compared the results of men and women using the Student's t-test for independent samples (continuous variables) and the x2 test (categorical variables). We also evaluated the best-fit correlation between 6MWT distance and V˙O2max (e.g., linear, exponential, and quadratic, using the statistical package curve estimation tool).
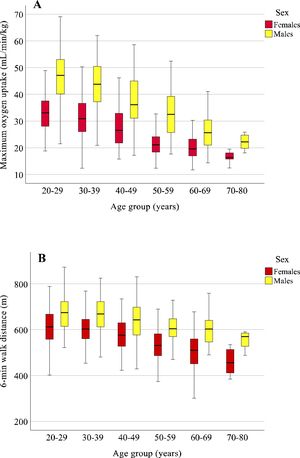
We determined age- and sex-related changes in V˙O2max and 6MWT distance using box plot graphs, wherein we calculated the average decline per decade (18–29, 30–39, 40−49, 50–59, 60−80 years) and sex-related differences were calculated. We evaluated the interaction between sex and age using a two-way analysis of variance (ANOVA) considering the aforementioned age groups and sex as factors.
Descriptive statistics were used to elaborate tables of norms for V˙O2max and 6MWT distance. We calculated the median of the values (50th percentile) and the 5th, 25th, 75th, and 95th percentiles, representing very low, low, regular, good, excellent, and superior CRF.
So that our results could be used in other countries, we developed a CRF classification based on the 6MWT distance, expressed as a percentage of the predicted value.17V˙O2max was used as the gold standard criterion to develop ROC curves, in which we identified the 6MWT distance with the best combination of sensitivity and specificity to predict the classification of V˙O2max. We calculated the areas under the ROC curves and considered those with values>0.80 as excellent and those with values between 0.70 and 0.80 as good.18 The other values were deemed inadequate.
The probability of alpha error was set at 5% for all analyses. Statistical analyses were performed using STATA software, version 14, and MedCalc software, version 19.
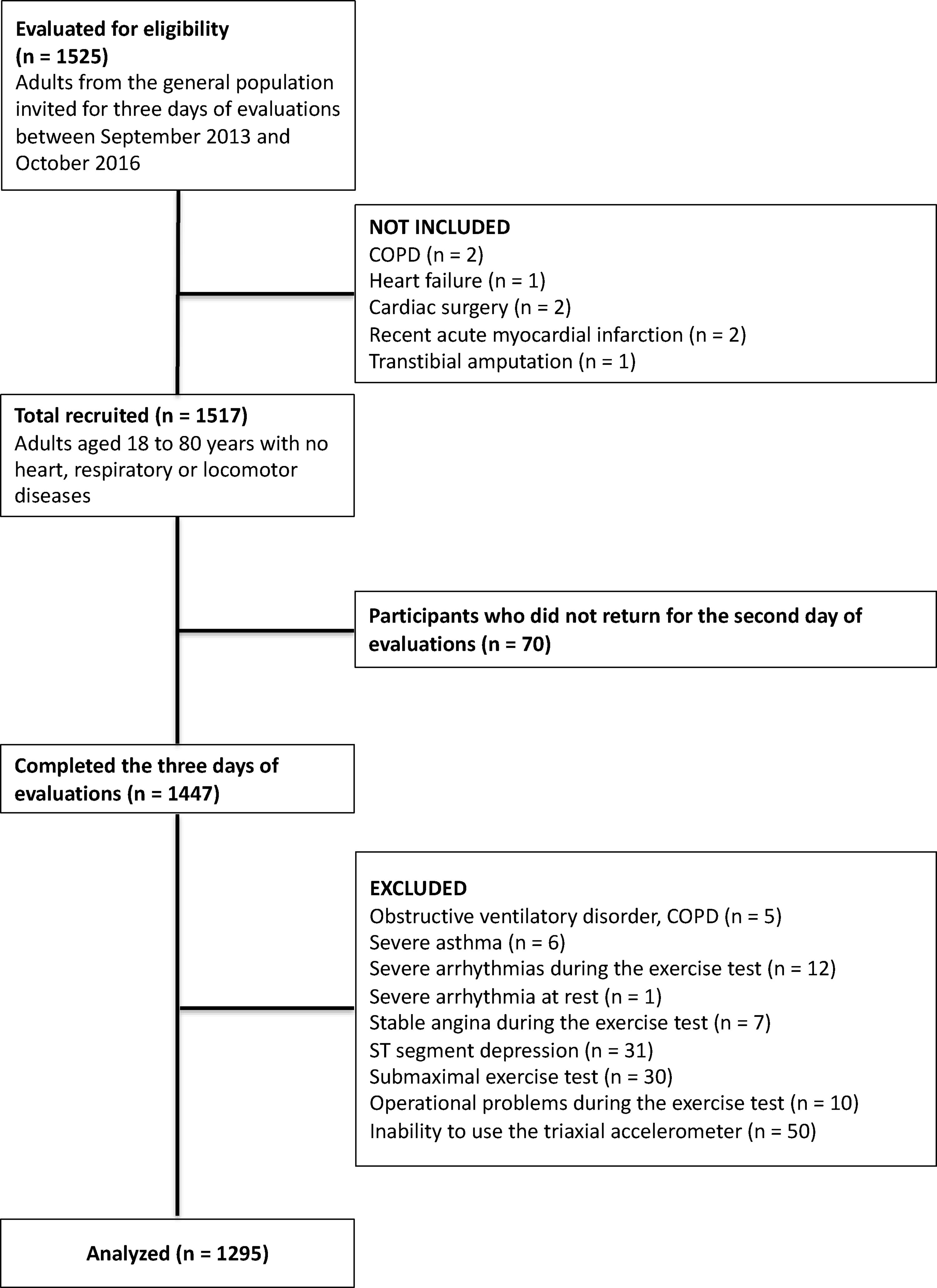
ResultsIn total, 1525 participants were assessed for eligibility, and 1517 met the inclusion criteria. Of these, 1447 participants completed all of the assessments. After exclusion, the results of 1295 men and women aged from 18 to 80 years were analyzed (Fig. 1).
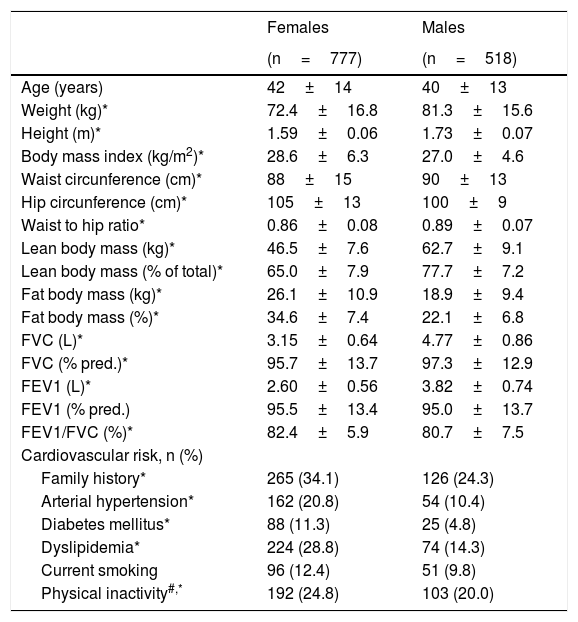
The participants were predominantly women (60%). On average, they were middle-aged and overweight. Women showed a higher cardiovascular risk than men (Table 1).
General characteristics of the studied sample.
| Females | Males | |
|---|---|---|
| (n=777) | (n=518) | |
| Age (years) | 42±14 | 40±13 |
| Weight (kg)* | 72.4±16.8 | 81.3±15.6 |
| Height (m)* | 1.59±0.06 | 1.73±0.07 |
| Body mass index (kg/m2)* | 28.6±6.3 | 27.0±4.6 |
| Waist circunference (cm)* | 88±15 | 90±13 |
| Hip circunference (cm)* | 105±13 | 100±9 |
| Waist to hip ratio* | 0.86±0.08 | 0.89±0.07 |
| Lean body mass (kg)* | 46.5±7.6 | 62.7±9.1 |
| Lean body mass (% of total)* | 65.0±7.9 | 77.7±7.2 |
| Fat body mass (kg)* | 26.1±10.9 | 18.9±9.4 |
| Fat body mass (%)* | 34.6±7.4 | 22.1±6.8 |
| FVC (L)* | 3.15±0.64 | 4.77±0.86 |
| FVC (% pred.)* | 95.7±13.7 | 97.3±12.9 |
| FEV1 (L)* | 2.60±0.56 | 3.82±0.74 |
| FEV1 (% pred.) | 95.5±13.4 | 95.0±13.7 |
| FEV1/FVC (%)* | 82.4±5.9 | 80.7±7.5 |
| Cardiovascular risk, n (%) | ||
| Family history* | 265 (34.1) | 126 (24.3) |
| Arterial hypertension* | 162 (20.8) | 54 (10.4) |
| Diabetes mellitus* | 88 (11.3) | 25 (4.8) |
| Dyslipidemia* | 224 (28.8) | 74 (14.3) |
| Current smoking | 96 (12.4) | 51 (9.8) |
| Physical inactivity#,* | 192 (24.8) | 103 (20.0) |
FVC: forced vital capacity; FEV1: forced expiratory volume in 1s.
The proportion of accelerometer-based physical inactivity was lower (30%) than that described for the general population. The participants used the accelerometer for 884±76min/day. The percentages of total time spent in sedentary behavior, light physical activity, and moderate-to-vigorous physical activity were 73%, 22%, and 5%, respectively.
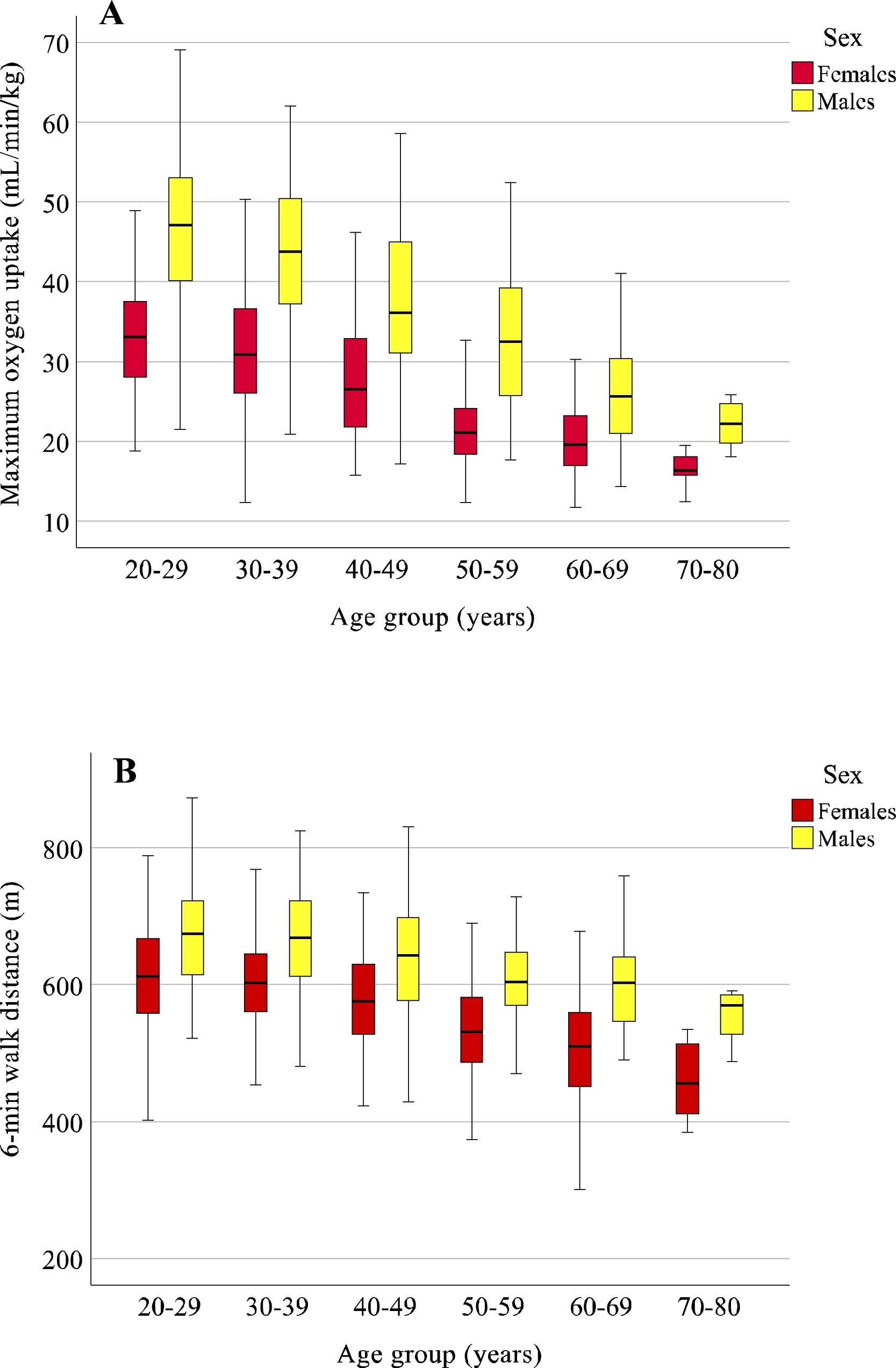
Considering the age groups of 18–29, 30–39, 40−49, 50–59, 60–69, and 70–80 years, V˙O2max declined with advancing age per decade in men by 9.2%, 8.7%, 8.8%, 8.1%, and 8.8%, and women by 9.4%, 8.7%, 7.8%, 9.4%, 8.2%, both averaging 8.7% per decade. There was a significant interaction between age and sex, with V˙O2max always being significantly higher for men. However, such differences decreased progressively with advancing age (Fig. 2A).
Age- and sex-related changes in cardiorespiratory fitness in the studied sample. Maximum oxygen uptake (V˙ O2max) declined with advancing age, per decade, in men (9.2; 8.7; 8.8; 8.1; and 8.8%) and women (9.4; 8.7; 7.8; 9.4; 8.2%) with a significant interaction between sex and age, indicating reduction of the difference with aging (A). The distance covered in the six-minute walk test declined by 9.8, 9.5, 9.1, 9.5 and 8.8% for women and 9.9, 9.4, 9.5, 9.9 and 9.2% for men with a significant interaction between sex and age, indicating increased difference with aging.
Regarding the 6MWT distance in the age groups 18–29, 30–39, 40−49, 50–59, 60–69, and 70–80 years, the decline per decade was 9.8%, 9.5%, 9.1%, 9.5% and 8.8% for women and 9.9%, 9.4%, 9.5%, 9.9%, and 9.2% for men. On average, the 6MWT distance declined by 9.3% and 9.5% per decade for women and men, respectively. Unlike V˙O2max, we observed an interaction between sex and age with considerable differences between men and women with advancing age (Fig. 2B).
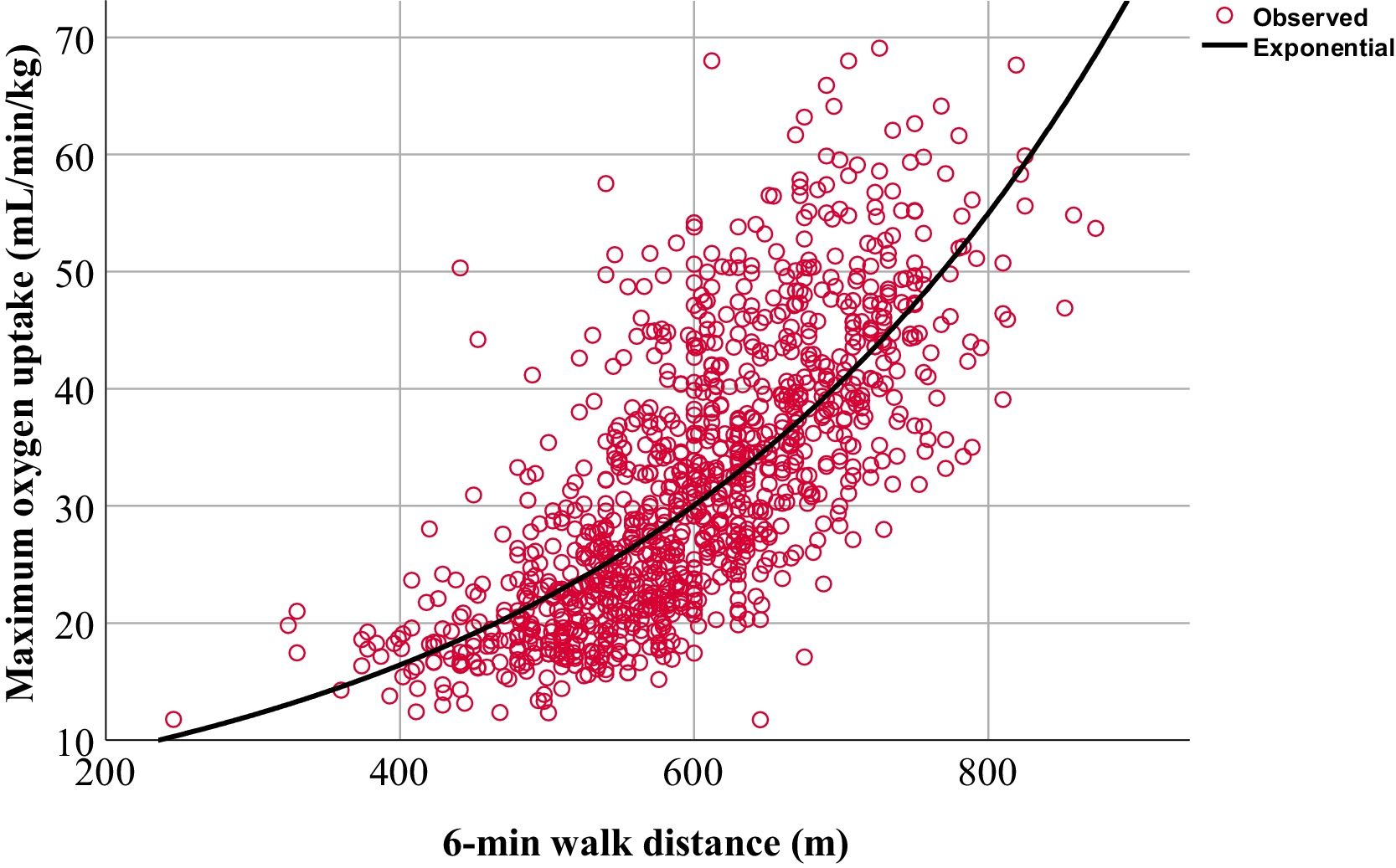
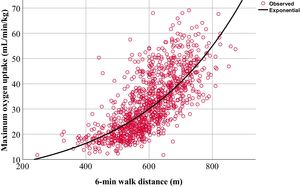
The 6MWT distance showed a significant correlation with V˙O2max, best explained by an exponential equation, with an evident ceiling effect for participants with a higher V˙O2max. The 6MWT distance alone explained approximately 55% of the total V˙O2max variability (Fig. 3).
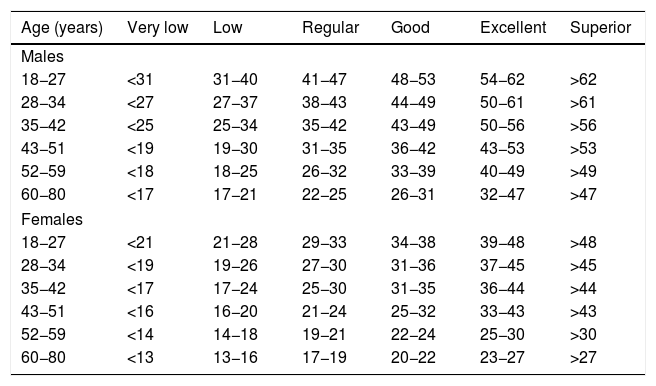
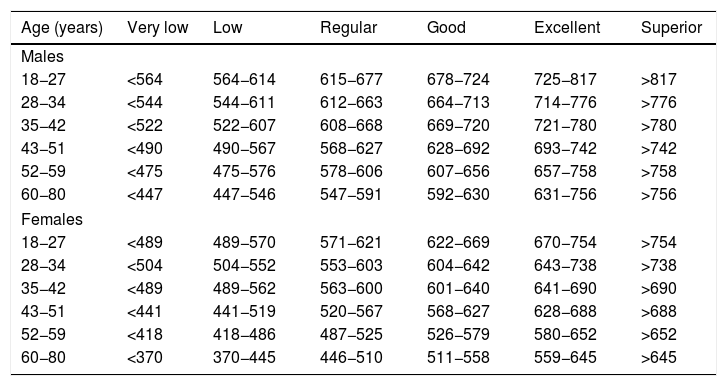
We stratified the CRF classification table as very low, low, regular, good, excellent, and superior considering a balanced proportion of participants in the age groups of 18−27, 28−34, 35−42, 43−51, 52−59, and 60−80 years, according to V˙O2max (Table 2) and 6MWT distance (Table 3).
Classification of cardiorespiratory fitness for men and women based on maximum oxygen uptake (V˙O2max) obtained directly in a cardiopulmonary exercise test on a treadmill following a ramp protocol.
| Age (years) | Very low | Low | Regular | Good | Excellent | Superior |
|---|---|---|---|---|---|---|
| Males | ||||||
| 18−27 | <31 | 31−40 | 41−47 | 48−53 | 54−62 | >62 |
| 28−34 | <27 | 27−37 | 38−43 | 44−49 | 50−61 | >61 |
| 35−42 | <25 | 25−34 | 35−42 | 43−49 | 50−56 | >56 |
| 43−51 | <19 | 19−30 | 31−35 | 36−42 | 43−53 | >53 |
| 52−59 | <18 | 18−25 | 26−32 | 33−39 | 40−49 | >49 |
| 60−80 | <17 | 17−21 | 22−25 | 26−31 | 32−47 | >47 |
| Females | ||||||
| 18−27 | <21 | 21−28 | 29−33 | 34−38 | 39−48 | >48 |
| 28−34 | <19 | 19−26 | 27−30 | 31−36 | 37−45 | >45 |
| 35−42 | <17 | 17−24 | 25−30 | 31−35 | 36−44 | >44 |
| 43−51 | <16 | 16−20 | 21−24 | 25−32 | 33−43 | >43 |
| 52−59 | <14 | 14−18 | 19−21 | 22−24 | 25−30 | >30 |
| 60−80 | <13 | 13−16 | 17−19 | 20−22 | 23−27 | >27 |
*According to the percentiles found: very low, <5th; low, 5th to 25th; regular, 26th to 50th; good, 51st to 75th; excellent, 76th to 95th; higher >95th. V˙O2max values presented in mL/min/kg.
Classification of cardiorespiratory fitness for men and women based on the distance covered in a six-minute walk test.
| Age (years) | Very low | Low | Regular | Good | Excellent | Superior |
|---|---|---|---|---|---|---|
| Males | ||||||
| 18−27 | <564 | 564−614 | 615−677 | 678−724 | 725−817 | >817 |
| 28−34 | <544 | 544−611 | 612−663 | 664−713 | 714−776 | >776 |
| 35−42 | <522 | 522−607 | 608−668 | 669−720 | 721−780 | >780 |
| 43−51 | <490 | 490−567 | 568−627 | 628−692 | 693−742 | >742 |
| 52−59 | <475 | 475−576 | 578−606 | 607−656 | 657−758 | >758 |
| 60−80 | <447 | 447−546 | 547−591 | 592−630 | 631−756 | >756 |
| Females | ||||||
| 18−27 | <489 | 489−570 | 571−621 | 622−669 | 670−754 | >754 |
| 28−34 | <504 | 504−552 | 553−603 | 604−642 | 643−738 | >738 |
| 35−42 | <489 | 489−562 | 563−600 | 601−640 | 641−690 | >690 |
| 43−51 | <441 | 441−519 | 520−567 | 568−627 | 628−688 | >688 |
| 52−59 | <418 | 418−486 | 487−525 | 526−579 | 580−652 | >652 |
| 60−80 | <370 | 370−445 | 446−510 | 511−558 | 559−645 | >645 |
*According to the percentiles found: very low, <5th; low, 5th to 25th; regular, 26th to 50th; good, 51st to 75th; excellent, 76th to 95th; higher >95th. Six-minute walk distance values presented in meters.
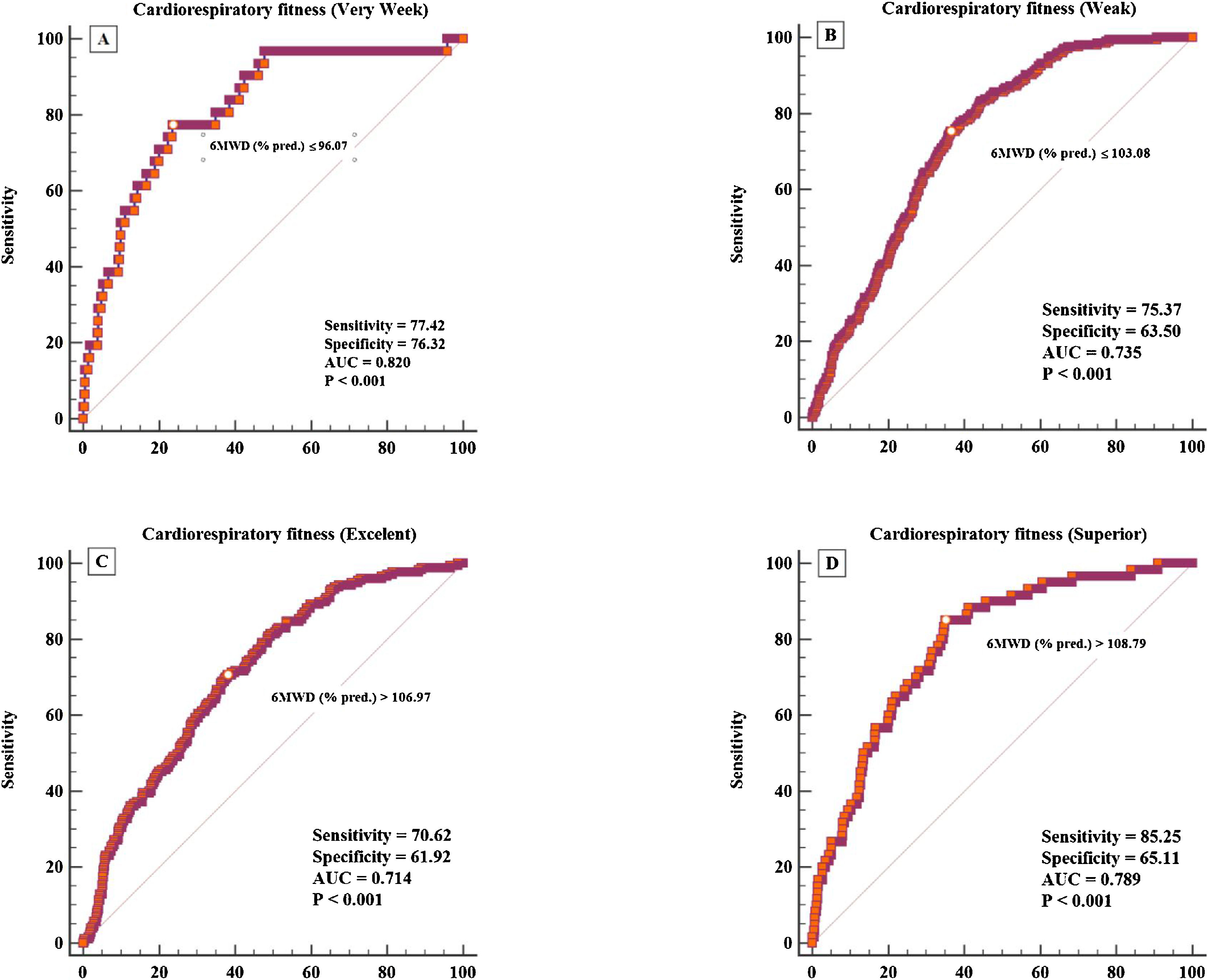
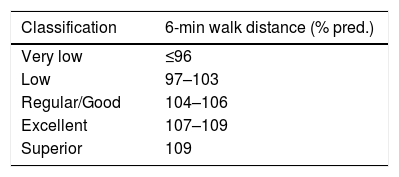
The percentage of the predicted 6MWT distance showed excellent ability to predict very low CRF, considering the CRF classification obtained using V˙ O2max as the gold standard. It was also able to predict low, excellent, and superior CRF well, although it could not differentiate between regular and good CRF (Fig. 4). Based on the cut-off values obtained through ROC curves, we classified the CRF based on the 6MWT distance as a percentage of the predicted (Table 4).
Receiver operational curves (ROC) for assessing the sensitivity and specificity of the distance covered in the six-minute walk test to identify individuals with the following percentiles of cardiorespiratory fitness classification: very low (A), < 5th; low (B), 5th to 25th; excellent (C), 76th to 95th; and superior (D) > 95th, according to the maximum oxygen uptake obtained in the treadmill cardiopulmonary exercise test.
AUC: area under the ROC curve.
Classification of cardiorespiratory fitness based on the distance covered in the six-minute walk test compared to the maximum oxygen uptake obtained in the cardiorespiratory exercise test (gold standard criterion).
| Classification | 6-min walk distance (% pred.) |
|---|---|
| Very low | ≤96 |
| Low | 97–103 |
| Regular/Good | 104–106 |
| Excellent | 107–109 |
| Superior | 109 |
% predicted by Iwama et al.10
To the best of our knowledge, this is the first study to formulate CRF classification tables using the 6MWT distance rather than the gold standard (V˙O2max). We present CRF classification tables based on a simple, valid, reliable, reproducible, and responsive field test to express CRF. The 6MWT distance classification was valid for mainly identifying individuals with low CRF. Our results will allow a more straightforward screening of cardiovascular risk in the clinical setting.
The 6MWT can be performed in corridors as short as 20m, and, in case of mild outdoor temperature, outdoors, which opens up varying prospects for using the 6MWT in clinical practice as a routine strategy. We observed that the relationship between the 6MWT distance and V˙ O2max was not linear. Our results indicate what has already been described as a ceiling effect, i.e., after a certain distance, minimal increases in the 6MWT distance are associated with substantial changes in V˙O2max.19 Therefore, we believe that our research meets the current AHA recommendations regarding the importance of routinely assessing and improving CRF in the clinical setting.1
One of the most relevant results of the present study was the creation of a CRF classification table based on the 6MWT distance, facilitating the interpretation of CRF assessments via field tests in different clinical settings. Normal values were calculated and ROC curves were used to validate our data valid for identifying people with different CRF classifications. Therefore, if the 6MWT distance is expressed as a percentage of the predicted value, we may assume that our results will be valid internationally.
Considering the AHA's recommendations on the importance of identifying people with low CRF to prevent cardiovascular diseases,1 our study makes it possible to estimate and interpret CRF in a straightforward, inexpensive, and effective way for clinical practice. We identified, with excellent sensitivity and specificity, very low CRF. In addition, we verified that a 6MWT distance <96% is a critical point for identifying individuals with CRF below the normal range. Sperandio et al.20 obtained the same cut-off point to identify physically inactive individuals evaluated using accelerometers. These results indicate that a 6MWT distance below 96% is equally crucial for identifying low physical activity levels and fitness levels.
There are several equations to predict the 6MWT distance in our population.21–24 Britto et al.’s24 equation has been suggested as the most suitable.25 However, we have been using the equation proposed by Iwama et al.17 for several years. In addition to not offering significantly different results, both for healthy individuals23 and patients with chronic lung disease,26 the equation proposed by Iwama et al.17 has some advantages. First, due to its adequate cross-validation performed in another research center with different researchers.27 Second, information on physical activity levels was evaluated using a validated instrument.28 Third, the equation was developed for adults of a wide age range (18–84 years). Lastly, we calculated the 6MWT distance values obtained in the present study as the percentage of the predicted values using the equations of Brito et al.23 and Iwama et al.,17 resulting in a difference of only 1±6% between the equations, which would hardly compromise the interpretation of the data described here.
We assessed the age- and sex-related changes in the 6MWT distance in adults over a wide age range sample size. The decline in V˙O2max per decade found in the present study is very consistent with that previously described in Brazil and other countries.29–32 Our results also reinforce previous data, indicating a decrease in CRF across the lifespan irrespective of sex.33 Even so, the sex-related differences in CRF seem to be more pronounced earlier in life and begin to narrow in older adults.
Unlike V˙ O2max, for which sex-related differences decreased with advancing age, the 6MWT distance showed differences between men and women progressively increasing with advancing age.29–32 Advanced age compromises the levels of anabolic hormones and the number of type II muscle fibers, more pronounced than in young men. Considering that the CPET is a maximal test, it requires the recruitment of fast-twitch motor units during a significant part of the test, justifying the lower advantage of men in the most advanced age groups. On the other hand, the 6MWT is a submaximal test that requires much less contribution from type II muscle fibers. The dynamic V˙O2 behavior during the 6MWT is monoexponential, with a tendency to stabilize after the third minute of the test.19,24,34 Thus, the most considerable differences between men and women in older age occurred because 6MWT is performed mainly with oxidative metabolism in energy production.
Several studies have developed predictive models for V˙O2max using non-exercise variables. In summary, these studies showed that regardless of the standard error of the estimate described, the models improved the prediction of cardiovascular risk.35 Therefore, considering the standard error of the exponential equation that we have proposed here to estimate V ̇O2max based on the 6MWT distance, we believe that our results will be beneficial for routine CRF assessment in clinical practice.
This study has practical implications for health. First, the normality tables for the 6MWT can help assess and monitor CRF in the general population and patients with chronic diseases, improving overall cardiovascular risk screening. The strength of this study is that it provides a CRF classification table using a simple field walking test compared to a treadmill ramp protocol CPET in the Brazilian population. Further, despite its development in a specific population, we defined the CRF classification using 6MWT distance as % predicted, which opens up the opportunity to use our results internationally.
As limitations, we could cite the cross-sectional design as one of them, mainly considering the age- and sex-related changes in V˙O2max and 6MWT distance. However, it should be recognized that the decline mentioned above obtained in longitudinal investigations may introduce bias from the loss of participants with lower levels of physical activity and fitness to follow-up. While the convenience sample could be a limitation, our main objective was to elaborate tables for CRF classifications; thus, the broad range of physical activity and fitness level becomes a potential instead. In addition, our sample's sociodemographic characteristics are quite similar to those of the general population in Brazil, apart from the level of education.
We conclude that the classification of CRF using the 6MWT distance is valid compared to the directly evaluated CRF (V˙O2max), especially for identifying adults with low CRF. Altogether, our results could be used in clinical practice to better screen and monitor cardiovascular risk in adults in the general population and in patients with chronic diseases.
Author contributionsVD is the guarantor of the study and takes responsibility for the accuracy of the data. VD and RN played the most crucial roles in this study and were responsible for study design and conception, statistical analysis, interpretation of the results, drafting, writing, and submission of the manuscript. MS, VL, AG, MR, and RA contributed to the study's conception and design, data collection, interpretation of the results contributed to drafting the article and critically revised it for relevant intellectual content. RA also contributed to exercise test supervision and was the main factor responsible for granting our participants' safety. ST and IG contributed to interpreting the results, article drafting, and critical revisions for prominent intellectual content.
FundingSão Paulo Research Foundation (FAPESP) granted this project (2011/07282-6; 2018/11817-1; and 2018/21536-0); however, it did not influence the interpretation of the results and conclusions obtained in the present study.
Conflicts of interestThe authors have no conflicts of interest to declare.
We dedicate this work to Dr. Antônio Ricardo de Toledo Gagliardi (in memoriam), who passed away after carrying out this research. Dr. Gagliardi was an extremely competent endocrinologist and researcher. During the last ten years, his partnership was a cornerstone for the quality of the research carried out at the Loboratory of Epidemiology and Human Movement (EPIMOV) at UNIFESP. We thank the Angiocorpore Institute of Cardiovascular Medicine (Santos, Brazil) for providing the infrastructure needed to conduct cardiopulmonary exercise tests, including physician supervision. We would also like to thank all the students/researchers, and personnel from the lab for their professional assistance with data collection.