Patients with chronic obstructive lung diseases often remain symptomatic even though optimal standard care, including pharmacological and non-pharmacologic treatment such as oxygen therapy and pulmonary rehabilitation, is provided.1 Recent studies in these patients demonstrated that several music interventions, such as singing, listening and playing music, resulted in improvement in psychological outcomes (quality of life, dyspnea and anxiety) and mixed results in physiological outcomes.2 From the pathophysiological stand point, among patients with obstructive lung diseases, the use of wind musical instruments may be an appropriate intervention as their use replicates one of the traditional standardized treatments, the pursed lips breathing technique. This is especially so for instruments that utilize low breathing pressure, such as the harmonica, recorder or flute.3,4
The aim of the study was to investigate the impact of collective teaching and practice of transverse flute, as a component of a pulmonary rehabilitation program (PRP), on respiratory functional capacity and quality of life among patients with chronic obstructive lung diseases.
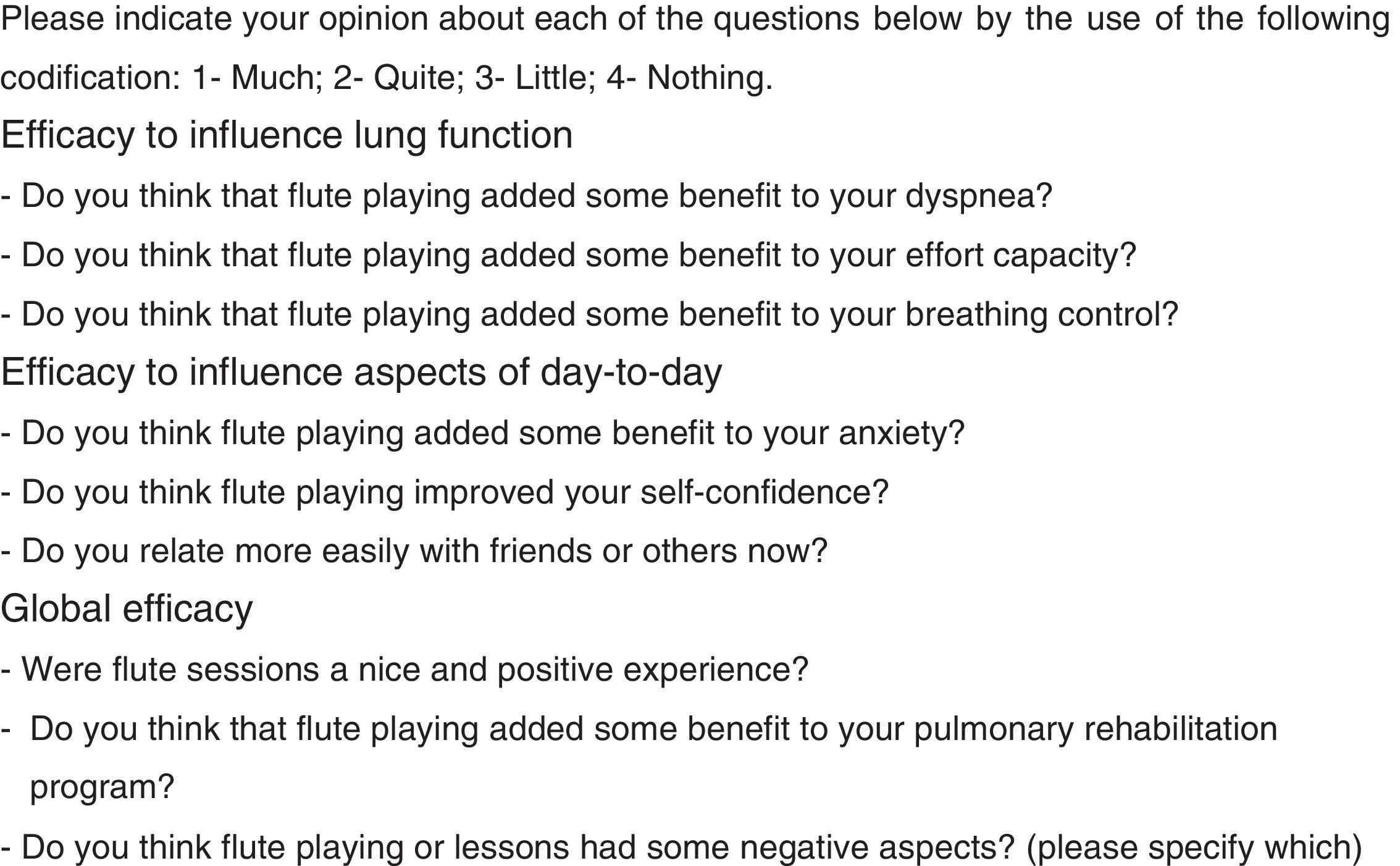
A prospective study was conducted, between October 2015 and April 2016 (28 sessions), at the Physical Medicine and Rehabilitation Department of the Hospital Pedro Hispano – Portugal. Patients with clinically stable chronic obstructive lung diseases who had participated in at least six weeks of a PRP and with availability for the project were selected; written informed consent was obtained from each patient. The patients then enrolled in weekly classes, coordinated by a flute teacher, each class lasting approximately 1h. Initially, the patients learned the music notes and how to play the transverse flute. Subsequent classes consisted of warm-up exercises with single notes, followed by playing songs of increasing difficulty. The patients were encouraged to practice at home during the week. Patient demographics and clinical histories were recorded, and patients were evaluated at the beginning and at the end of the study period with a six minute walk test (6MWT), maximal respiratory pressures and several questionnaires: Saint George's Respiratory Questionnaire, COPD Assessment Test, EuroQoL-5D Test, Hospital Anxiety and Depression Scale, London Chest Activity of Daily Living Scale and Medical Research Council Dyspnea Questionnaire. On the final evaluation, patients also responded to a self-perceived efficacy questionnaire drawn up by the researchers (Fig. 1). A descriptive analysis was then performed.
Six patients were selected to participate in the study, of which one died due to an extrapulmonary cause. Of the five patients who finished the study, two had one acute exacerbation, and one had a new diagnosis of hypothyroidism during the period of the study.
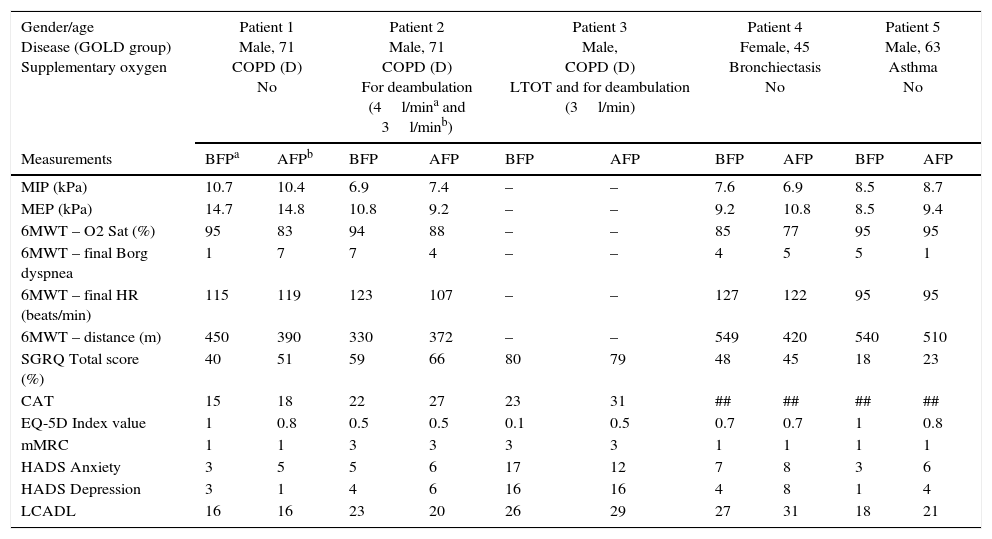
The sample characterization and results are listed in Table 1.
Pulmonary function tests, symptoms and health-related quality of life questionnaires before and after the program.
| Gender/age Disease (GOLD group) Supplementary oxygen | Patient 1 Male, 71 COPD (D) No | Patient 2 Male, 71 COPD (D) For deambulation (4l/mina and 3l/minb) | Patient 3 Male, COPD (D) LTOT and for deambulation (3l/min) | Patient 4 Female, 45 Bronchiectasis No | Patient 5 Male, 63 Asthma No | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Measurements | BFPa | AFPb | BFP | AFP | BFP | AFP | BFP | AFP | BFP | AFP |
| MIP (kPa) | 10.7 | 10.4 | 6.9 | 7.4 | – | – | 7.6 | 6.9 | 8.5 | 8.7 |
| MEP (kPa) | 14.7 | 14.8 | 10.8 | 9.2 | – | – | 9.2 | 10.8 | 8.5 | 9.4 |
| 6MWT – O2 Sat (%) | 95 | 83 | 94 | 88 | – | – | 85 | 77 | 95 | 95 |
| 6MWT – final Borg dyspnea | 1 | 7 | 7 | 4 | – | – | 4 | 5 | 5 | 1 |
| 6MWT – final HR (beats/min) | 115 | 119 | 123 | 107 | – | – | 127 | 122 | 95 | 95 |
| 6MWT – distance (m) | 450 | 390 | 330 | 372 | – | – | 549 | 420 | 540 | 510 |
| SGRQ Total score (%) | 40 | 51 | 59 | 66 | 80 | 79 | 48 | 45 | 18 | 23 |
| CAT | 15 | 18 | 22 | 27 | 23 | 31 | ## | ## | ## | ## |
| EQ-5D Index value | 1 | 0.8 | 0.5 | 0.5 | 0.1 | 0.5 | 0.7 | 0.7 | 1 | 0.8 |
| mMRC | 1 | 1 | 3 | 3 | 3 | 3 | 1 | 1 | 1 | 1 |
| HADS Anxiety | 3 | 5 | 5 | 6 | 17 | 12 | 7 | 8 | 3 | 6 |
| HADS Depression | 3 | 1 | 4 | 6 | 16 | 16 | 4 | 8 | 1 | 4 |
| LCADL | 16 | 16 | 23 | 20 | 26 | 29 | 27 | 31 | 18 | 21 |
COPD, chronic obstructive pulmonary disease; GOLD group, group according the Global Initiative for Chronic Obstructive Lung Disease; LTOT, Long-term oxygen therapy; MIP, maximal inspiratory pressure; MEP, maximal expiratory pressure; 6MWT (O2 Sat), oxygen saturation at the end of six minutes walk test; 6MWT (final Borg dyspnea), Modified Borg scale for dyspnea at the end of six minutes walk test; 6MWT (final HR), heart rate at the end of six minutes walk test; 6MWT (distance/meters), distance walked at the end of six minutes walk test. SGRQ, St. George's Respiratory Questionnaire; CAT, COPD Assessment Test; EQ-5D, EuroQoL-5 dimensions test, descriptive system; mMRC, Modified Medical Research Council Dyspnea Scale; HADS Anxiety, Hospital Anxiety and Depression Scale, punctuation for anxiety; HADS Depression, Hospital Anxiety and Depression Scale, punctuation for depression; LCADL, London Chest Activity of Daily Living Scale.
One of the patients was not able to perform the functional tests. Of the remaining four, the maximum inspiratory pressures (MIP) increased after the flute program in two patients and decreased in the other two. The maximum expiratory pressures (MEP) increased in three of the four patients who performed the test. In the 6MWT, we observed an increase in the distance walked only for “patient 2”; the others showed a decreased distance. Before the flute program, only one patient had final oxygen saturation below 90%; afterwards, three patients desaturated below 90%.
In the questionnaires, we found that globally, and from baseline enrolment, these were symptomatic patients, for whom the disease had negative impact on their quality of life. After the flute program, only “patient 3” presented improved values in three questionnaires (Saint George's Respiratory Questionnaire, EuroQoL-5D Test and Hospital Anxiety Scale). The remaining patients maintained their initial scores or experienced a slight deterioration of scores.
With respect to the self-perceived efficacy questionnaire (Fig. 1), relative to functional and day-to-day aspects, all patients considered that the flute sessions helped “much” or “quite”, except two patients who reported “little” effect on anxiety control. Globally, all patients thought the experience was “much” pleasant and positive, namely in terms of respiratory rehabilitation, and negative aspects were not mentioned.
The study's limitations, namely the small number of patients and lack of a control group, compromise the ability to draw conclusions from the study. However, the patients with worsening results after the flute program were the two patients who had exacerbations and the one with recently diagnosed hypothyroidism, which may have influenced the inconsistent results obtained in the pulmonary function tests. In the questionnaires of symptoms and quality of life, the results were highly variable, but, in the subjective analysis, the flute program was perceived as a very positive experience.
Despite its limitations, this is a pioneering program, in which an musical instrument of greater technical complexity was used compared to previously published work.3,5 Beyond the physiopathological plausibility of its use as a component of a PRP, the preliminary results demonstrated a perceived good experience by the patients via subjective analysis. More research, with larger samples, longer duration and a control group, is needed to build up and strengthen the conclusions.
Conflicts of interestThe authors have no conflicts of interest to declare.
A special thanks to the flute teacher, Fátima Seabra, and to health professionals of Physical Medicine and Rehabilitation Department of Hospital Pedro Hispano, for all dedication.