Chronic obstructive pulmonary disease (COPD) increases resting energy expenditure (REE)1 due to chronic inflammation and greater effort for breathing.2 REE is the major component of total energy expenditure and the correct measurement of REE is essential to offer a proper nutritional management and consequently prevent or treat malnutrition. Up till now, there has been no consensus about which REE equation is the best to use in clinical practice to match the energy intake of older adults with COPD. Therefore, we aimed to compare predictive equations of REE with indirect calorimetry (IC) in older adults with COPD.
We evaluated 20 older adults with COPD (16 men and 4 women) and all subjects were selected from a pulmonary rehabilitation program of a private health service. The details of sample selection and recruitment have been previously described.1
Demographic and anthropometric data were used to calculate the REE using gender-specific predictive equations3: Mifflin St. Jeor equation, Harris & Benedict, World Health Organization (WHO)1, WHO2, Owen et al., and de Oliveira et al.
Indirect calorimetry (Metalyzer 3B – R2 (Cortex), breath by breath) was used for determining REE after calibration of barometric pressure (960mbar) and room air (O2: 20.93/CO2: 0.03vol%) using a known gas mixture (White Martins, O2: 15.94/CO2: 5.01vol%) and volume (3-L Hans Rudolph syringe, V=3.0L). REE was determined by Weir4 equation after measurement of oxygen consumption (VO2) and production of carbon dioxide (VCO2). The participants were asked to use a mask and remain silent until the steady state condition was reached over a 5-min period and 20% variation of VO2, 12% variation of VCO2 and 10% variation of RQ. Both room temperature (25.0±2.0°C) and relative humidity (47.0±4.5%) were controlled. None of the individuals presented flu, cold or cough during the assessment and all individuals were asked to avoid exercise and caffeinated or alcoholic beverages consumption during the 48h that preceded the assessment. The REE evaluation was performed after an overnight fast and all individuals came to the lab in the morning.
Weight (kg) and height (cm) were measured for determining body mass index (BMI). Waist circumference (WC), absolute fat, fat-free mass (FFM), and muscle mass were also measured, as described previously.1
In statistical analyses, data were presented as mean±standard derivation and percentage. ANOVA one-way was used to compare the differences between REE values from equations and indirect calorimetry, then Scheffe post hoc test was used to identify which equation value was equal to the REE value measured by IC. Intraclass correlation coefficient and Bland–Altman were applied to compare the differences between REE values from IC and tested equations. The software STATISTICA 6.0 was used for the statistical analyses and significance level was at p<0.05.
Regarding sociodemographic characteristics, the sample consisted of older adults, white (85%), not workers and mostly male gender (80%). The anthropometric data showed high adiposity with suboptimal muscle mass, as described previously.1
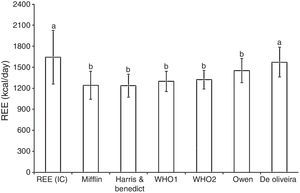
All equations, except de Oliveira et al., underestimated the values of REE measured by indirect calorimetry (indirect calorimetry=1643±383kcal/day, Mifflin St. Jeor equation=1243±197kcal/day (p<0.05), Harris and Benedict=1237.3±161kcal/day (p<0.05), WHO1=1300±144kcal/day (p<0.05), WHO2=1322±131kcal/day (p<0.05), Owen=1453±171kcal/day (p<0.05) and de Oliveira=1572.2±213kcal/day (p>0.05)) (Fig. 1).
Furthermore, after Bland and Altman analysis, Owen and de Oliveira equations were significantly associated with indirect calorimetry, whereas Owen et al. underestimated the REE in −190.2 (−343; −37.5)kcal/day or −9.9 (−20.1; 0.2)% and de Oliveira overestimated the REE in 302.3 (198.5; 406.3)kcal/day or 19.6 (12.4; 26.7)% (Table 1).
Coefficient analysis of intra-class correlation coefficient (ICC) and Bland and Altman of to estimate REE.
| Equations | ICC | ICC CI 95% | d | CI 95%/d | DP/d | CL 95% | d% | CI 95%/d% | SD/d% | CL 95%/d% |
|---|---|---|---|---|---|---|---|---|---|---|
| Mifflin | 0.18 | −0.28; 0.58 | −401.2 | −552.9; −249.5 | 324.2 | −1036.6; 234.1 | −25.9 | −35.3; −16.6 | 19.9 | −65.1; 13.2 |
| Harris | 0.01 | −0.44; 0.45 | −404.5 | −568.2; −242.8 | 347.5 | −1086.7; 275.6 | −25.7 | −36.2; −15.3 | 22.4 | −69.7; 18.2 |
| WHO | 0.07 | −0.39; 0.50 | −342.3 | −502.8; −181.7 | 343.1 | −1114.7; 330.1 | −20.1 | −31.4; −10.2 | 22.9 | −65.6; −46.9 |
| WHO2 | 0.13 | −0.34; 0.54 | −321.1 | −481.6; −160.6 | 342.9 | −993.2; 350.9 | −19.0 | −29.4; −8.7 | 22.1 | −62.3; 24.3 |
| Owen | 0.37* | −0.08; 0.70 | −190.2 | −343.0; −37.5 | 326.3 | −829.9; 449.4 | −9.9 | −20.1; 0.2 | 21.7 | −52.5; 32.5 |
| de Oliveira | 0.47* | 0.04; 0.76 | 302.3 | 198.5; 406.3 | 222.1 | −132.8; 737.5 | 19.6 | 12.4; 26.7 | 15.2 | −10.2; 49.4 |
ICC=intra-class correlation coefficient; ICC CI 95%=confidence intervals for ICC; d=mean difference; CI 95%/d=confidence intervals for mean difference; SD=standard derivation; CL 95%=concordance limits for the mean difference; d% percentage difference.
Although de Oliveira equation showed similar mean values compared to IC, and an association was found between IC and de Oliveira and Owen equation, we noted high intervals of agreements between these equations and IC. For example, de Oliveira overestimated the REE in 302kcal and Owen underestimated in 190kcal, which can result in high or low energy intake, respectively. Hence, we suggest that none of the equations tested in the present study should be used in clinical practice for older adults with COPD because it is equally undesirable to overestimate energy expenditure as to underestimate it. Both extremes are counterproductive and might have consequences for the patient because overfeeding leads to higher carbon dioxide production which increases the work of breathing5; and low energy and protein intake can result in muscle mass loss6 that is associated with higher mortality in older adults7 and in COPD patients.8 Thus, none of the equations was ideal for estimating REE in older adults with COPD and there is a need to create new equations for this specific population.
The main limitation of the present study was that the small sample size constituted mainly by male patients does not permit speculation about these results in general COPD population and more studies evaluating higher number of older adults with COPD are needed.
Therefore, we concluded that the majority of equations underestimated the REE and all equations showed low association with IC. Therefore, we suggest that the REE equations used at present study should not be used in older adults with COPD.
Conflicts of interestThe authors have no conflicts of interest to declare.
FAPEMIG and CAPES for financial support.