Chronic obstructive pulmonary disease (COPD) is a major public health problem. The aim of this study was to ascertain the prevalence of COPD and whether such prevalence was positively or negatively associated with COPD admissions, using all the data of a regional health care system.
Materials and methodsWe designed a descriptive cross-sectional study which included all subjects aged over 45 years, diagnosed with COPD in primary care in 2013. We also calculated the number of such patients who had a record of hospital admissions due to this disease. COPD prevalence and incidence of admissions were calculated. Poisson regression models were then used to analyse the association between cases with diagnosis of COPD and admissions due to COPD, by sex, adjusting for socio-demographic variables and distance to hospital. Sensitivity subanalyses were performed by reference to the respective municipal rurality indices.
ResultsMedian municipal prevalence of COPD was 5.29% in men and 2.19% in women. Among patients with COPD, 28.22% of men and 16.00% of women had at least one hospital admission. The relative risk of admission per unit of the standardised prevalence ratio was 0.37 (95% CI 0.34–0.41) for men and 0.39 (95% CI 0.34–0.45) for women.
ConclusionsThere is a significant negative association between COPD prevalence and hospital admissions due to this disease. The proportion of admissions is lower in municipalities lying furthest from hospitals. There is considerable municipal variability in terms of COPD prevalence and proportion of admissions. In-depth attention should be given to disease-management training programmes.
Chronic obstructive pulmonary disease (COPD) is a major public health problem, ranking as the 3rd leading cause of death world-wide.1 In Spain, the prevalence of COPD is estimated to be 10.2% in the population aged 40–80 years, it is higher in men than in women, and increases with age.2
COPD is traditionally associated with worse quality of life, and patients frequently suffer from episodes of exacerbations which may require hospital admission.3 The number of exacerbations ranges widely among patients.4 It has been estimated that, in Europe, it accounts for 56% of the cost of all respiratory diseases,5,6 with almost 60% of the overall cost of COPD being attributable to exacerbations.7
The pattern of association between prevalence and exacerbation could yield information on the type of attention being provided in primary care and whether this might somehow have an influence on ensuring more appropriate control of the disease. In principle, greater hospital use would be expected in municipalities with a higher prevalence of COPD, adjusted for patients’ age.
Accordingly, the aim of this study was to ascertain COPD prevalence in a region of Spain, and whether a given municipal prevalence was positively or negatively associated with COPD admissions from that same municipality. Galician health information systems were used for the purpose.
Material and methodsDesign and settingGalicia is situated in north-west Spain. Galicia has a surface area of 29,574km2 and a population of 2,732,347 More than 50% of the population is aged 45 years or over.8 It has 314 municipalities, which is the basic administrative unit in Spain. The region has a universal, free health-care system and only 3% of the population has a private health insurance.
We designed a descriptive cross-sectional study, which included subjects over the age of 45 years, diagnosed with COPD and registered as patients in Galician health information systems. Municipality was used as the level of aggregation, and the study was based on data for the year 2013 for the purpose of admissions due to exacerbation of COPD and 31 December 2013 for prevalence purposes.
Data sourcesThe study data were sourced exclusively from existing health information systems, with data on COPD being drawn from the Galician Health Service databases and data on the reference population of each municipality being drawn from the National Statistics Institute (INE).9
Galicia is a pioneer in the use of electronic medical records, i.e., a unified register of all clinical information on health-related. The information is stored in different databases: for study purposes, we used just two, namely, the primary-care database and the Minimum Basic Data Set (MBDS). The primary-care database contains all data on primary care resources and activity. From this we extracted data on patients shown to have had at least one open active or index episode of COPD in primary care (International Classification of Primary Care/ICPC-2 code R95) at 31 December 2013. The episode of COPD is based on cases which showed up for primary care attention (in principle, symptomatic cases) and not on wide-based spirometric findings. Any patient who is registered with the R95 code by the primary care physician is defined as a COPD case.
The MBDS contains the records of health care activity pursuant to diagnostic coding on admission to public acute hospitals. Information was extracted from this database on patients with COPD registered as the cause of admission or secondary diagnosis during 2013. The codes considered as COPD were International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes 492.8, 491.20, 491.21, 493.22 and 496. The decision to specifically include these codes was taken after a meeting with pneumologists and coders. Duplicate records pertaining to successive admissions were eliminated. COPD cases are patients diagnosed with COPD at December 31, 2013. COPD admission are patients who were admitted at least once during the year 2013.
Galician population data for 2013 were sourced from municipal rolls at INE. All data (COPD and general population) were aggregated by municipality, according to sex and age group (45–64, 65–74, over 74 years).
Socio-demographic data for each municipality were supplied by the Galician Statistics Institute (IGE),8 to enable subsequent statistical adjustment at a municipal level for percentage of illiteracy, percentage of social security affiliations (% of persons who are employed) for each sex, median pension, gross domestic product (GDP) (euros per inhabitant), average number of primary care physicians per inhabitant, percentage of population gainfully employed, and rurality index. Lastly, we considered the distance from each municipality to the nearest hospital.
Statistical analysisCOPD prevalence by sex was calculated on the basis of primary care data, and incidence of admissions due to exacerbation on the basis of the MBDS. We calculated COPD prevalence using as the denominator the population of each municipality older than 45 years. In the calculation of the incidence of admissions, COPD cases were used as the denominator, with the proportion of admissions being calculated by reference to cases of COPD diagnosed per study unit (municipality).
The association between cases with diagnosis of COPD in primary care and admissions due to COPD was analysed by sex, using Poisson regression models with random effects terms (mixed models). In order for COPD cases (primary care) to be taken into account in the model, we previously calculated the standardised prevalence ratio (SPR). To standardise the prevalence, the sum of the total population of all the municipalities was used as reference population. In this way we can compare each municipality with the population that we have considered as a reference. So, we use a measure which enables municipalities to be compared to one another, taking the age structure into account. The dependent variable was observed cases of admissions due to COPD, with expected cases as offset. Observed cases were calculated by means of internal comparison (based on specific rates for each age group and sex of the population), and expected cases were calculated on the basis of cases with diagnosis of COPD in primary care.
The random effects term was district, and the fixed effects were the SPR of COPD, along with the remaining variables of adjustment (socio-demographic data and minimum distance to hospital).
The model takes the following form:
Oi∼Poisson (Eiλi),
log(λi)=α+Σbi→Oi∼SPR+covariates of adjustment+district (random effect)
where λi is the relative risk (RR), Oi is the number of observed cases, Ei is the number of expected cases, α is the intercept, and bi are the effects associated with the remaining covariates.
A sensitivity subanalysis was conducted by reference to the respective municipal rurality indices. The results were expressed as RRs with their 95% CIs. For the estimates, we used integrated nested Laplace approximation (R-INLA) performed with the R programme version 3.1.1.10,11
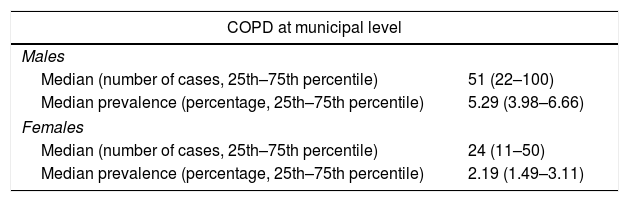
ResultsThere were 53,261 cases of COPD (67.6% men) in Galicia in 2013, with the median municipal prevalence among persons over the age of 45 years being 5.29% in men and 2.19% in women. Among patients with COPD, 28.22% of men and 16.00% of women had a minimum of one hospital admission in 2013. A more detailed description of study participants can be found in Table 1.
COPD cases in primary care and hospital admissions by municipality in 2013.
| COPD at municipal level | |
|---|---|
| Males | |
| Median (number of cases, 25th–75th percentile) | 51 (22–100) |
| Median prevalence (percentage, 25th–75th percentile) | 5.29 (3.98–6.66) |
| Females | |
| Median (number of cases, 25th–75th percentile) | 24 (11–50) |
| Median prevalence (percentage, 25th–75th percentile) | 2.19 (1.49–3.11) |
| Hospital admissions by municipality | |
|---|---|
| Males | |
| Median (number of cases, 25th–75th percentile) | 15 (8–25) |
| Median percentage of hospital admissions in COPD patients (25th–75th percentile) | 28.22 (21.01–40.00) |
| Females | |
| Median (number of cases, 25th–75th percentile) | 4 (2–8) |
| Median percentage of hospital admissions in COPD patients (25th–75th percentile) | 16.00 (9.77–27.50) |
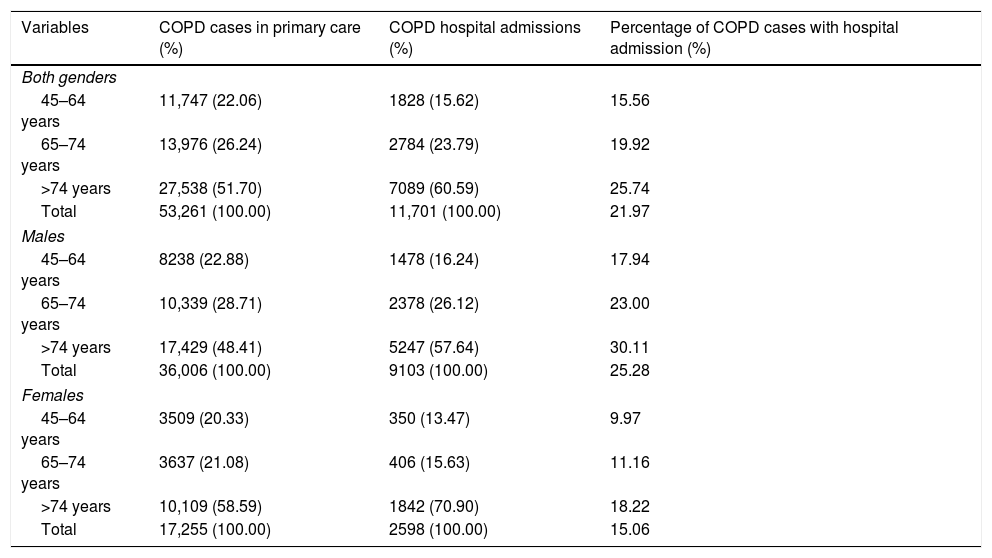
Over 50% of patients were aged over 74 years. The distribution by age was similar in both sexes. A total of 11,701 patients (77.8% men) had a minimum of one admission in 2013. The highest percentage of admissions occurred in the over-74 age group (Table 2).
COPD distribution broken down by age and gender (primary care and hospital admissions) in 2013.
| Variables | COPD cases in primary care (%) | COPD hospital admissions (%) | Percentage of COPD cases with hospital admission (%) |
|---|---|---|---|
| Both genders | |||
| 45–64 years | 11,747 (22.06) | 1828 (15.62) | 15.56 |
| 65–74 years | 13,976 (26.24) | 2784 (23.79) | 19.92 |
| >74 years | 27,538 (51.70) | 7089 (60.59) | 25.74 |
| Total | 53,261 (100.00) | 11,701 (100.00) | 21.97 |
| Males | |||
| 45–64 years | 8238 (22.88) | 1478 (16.24) | 17.94 |
| 65–74 years | 10,339 (28.71) | 2378 (26.12) | 23.00 |
| >74 years | 17,429 (48.41) | 5247 (57.64) | 30.11 |
| Total | 36,006 (100.00) | 9103 (100.00) | 25.28 |
| Females | |||
| 45–64 years | 3509 (20.33) | 350 (13.47) | 9.97 |
| 65–74 years | 3637 (21.08) | 406 (15.63) | 11.16 |
| >74 years | 10,109 (58.59) | 1842 (70.90) | 18.22 |
| Total | 17,255 (100.00) | 2598 (100.00) | 15.06 |
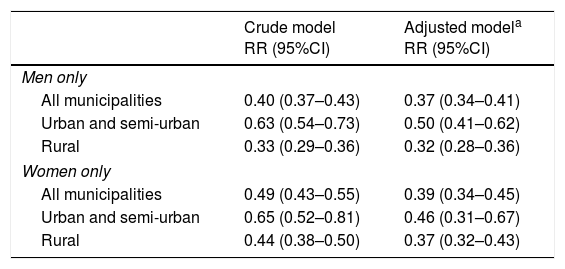
Shown in Table 3 are the RRs of admission according to the number of COPD cases per municipality. The RRs of admission for every increase of one unit in the standardised COPD prevalence ratio were 0.37 (95% CI 0.34–0.41) for men and 0.39 (95% CI 0.34–0.45) for women. In both sexes, the decrease in the probability of admission with the increase in the prevalence of COPD was higher in rural than in semi-urban and urban municipalities.
Relative risk of COPD hospital admissions (by Standardised Prevalence Rate unit).
| Crude model RR (95%CI) | Adjusted modela RR (95%CI) | |
|---|---|---|
| Men only | ||
| All municipalities | 0.40 (0.37–0.43) | 0.37 (0.34–0.41) |
| Urban and semi-urban | 0.63 (0.54–0.73) | 0.50 (0.41–0.62) |
| Rural | 0.33 (0.29–0.36) | 0.32 (0.28–0.36) |
| Women only | ||
| All municipalities | 0.49 (0.43–0.55) | 0.39 (0.34–0.45) |
| Urban and semi-urban | 0.65 (0.52–0.81) | 0.46 (0.31–0.67) |
| Rural | 0.44 (0.38–0.50) | 0.37 (0.32–0.43) |
Adjusted for percentage of illiteracy; social security affiliation by gender; median retirement income by municipality; gross domestic product (municipality) (euros per inhabitant); average number of physicians per inhabitant; percentage of population gainfully employed; rurality index; and minimum distance to hospital.
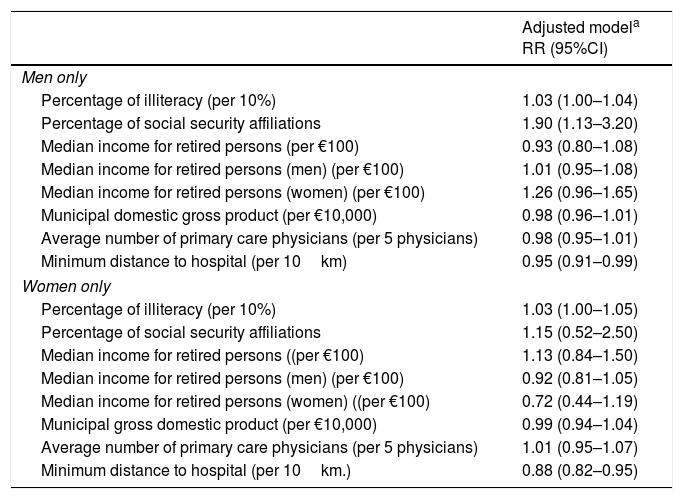
Table 4 sets outs the RRs of admission according to socio-demographic variables. Among men, there was a significant positive association with percentage of illiteracy (RR 1.03; 95% CI 1.00–1.04) and social security affiliations (RR 1.90; 95% CI 1.13–3.20); among women, there was a significant association with percentage of illiteracy (RR 1.03 95% CI 1.00–1.05) but the association was not maintained with social security affiliations. For both men and women there was a significant inverse relationship between number of admissions and distance to hospital, i.e., the greater the distance, the fewer the admissions due to exacerbations of COPD. This effect was more marked in women than in men.
Relative risk of hospital admission-related COPD with socio-economic variables.
| Adjusted modela RR (95%CI) | |
|---|---|
| Men only | |
| Percentage of illiteracy (per 10%) | 1.03 (1.00–1.04) |
| Percentage of social security affiliations | 1.90 (1.13–3.20) |
| Median income for retired persons (per €100) | 0.93 (0.80–1.08) |
| Median income for retired persons (men) (per €100) | 1.01 (0.95–1.08) |
| Median income for retired persons (women) (per €100) | 1.26 (0.96–1.65) |
| Municipal domestic gross product (per €10,000) | 0.98 (0.96–1.01) |
| Average number of primary care physicians (per 5 physicians) | 0.98 (0.95–1.01) |
| Minimum distance to hospital (per 10km) | 0.95 (0.91–0.99) |
| Women only | |
| Percentage of illiteracy (per 10%) | 1.03 (1.00–1.05) |
| Percentage of social security affiliations | 1.15 (0.52–2.50) |
| Median income for retired persons ((per €100) | 1.13 (0.84–1.50) |
| Median income for retired persons (men) (per €100) | 0.92 (0.81–1.05) |
| Median income for retired persons (women) ((per €100) | 0.72 (0.44–1.19) |
| Municipal gross domestic product (per €10,000) | 0.99 (0.94–1.04) |
| Average number of primary care physicians (per 5 physicians) | 1.01 (0.95–1.07) |
| Minimum distance to hospital (per 10km.) | 0.88 (0.82–0.95) |
Adjusted for: percentage of illiteracy; social security affiliation by gender; median retirement income by municipality; gross domestic product (municipality) (euros per inhabitant); average number of physicians per inhabitant; percentage of population gainfully employed; rurality index; and minimum distance to hospital. The model includes the main independent variable (standardised COPD prevalence rate).
There are very few studies which analyse the association between prevalence and COPD admissions, using health information systems. The main finding of this study is that the higher the reported prevalence of COPD, the lower the number of admissions referred to this clinical entity. Although globally the admissions are lower in municipalities with high prevalence, we must consider that there are exceptions in some municipalities. Furthermore, the probability of admission by reference to the standardised prevalence ratio is lower in rural than in urban and semi-urban municipalities. In terms of socio-demographic variables, the greater the distance to hospital, the lower the probability of being admitted due to COPD, which – as above – is true of both men and women.
There are various explanations which could account for the findings obtained. A plausible hypothesis might be that municipalities with a greater case-load carry out bettercontrol of their patients, thus requiring fewer admissions. Furthermore, these municipalities would tend to have less underdiagnosis of mild cases of COPD. It may also happen that municipalities with most cases, tend to be better equipped with the necessary means and resources for attending to COPD patients than do those with fewer patients. We were unable to include this type of adjustment in our analysis, though previous studies in the study area report important differences in the use of spirometers among the various primary care centres,12 something that may therefore support the hypothesis of the existence of a significant degree of variability in health care quality as between one municipality and the next.
While there are no studies that have analysed the association between the two indices (prevalence and admission) directly, there are studies which have linked a decline in COPD mortality to better organisational quality.13 A recent Cochrane review has shown that integrated COPD management programmes improve quality of life and reduce symptoms, hospital admissions and stays.14 Similarly, diverse studies highlight the fact that different interventions undertaken at primary care centres can reduce the number of successive admissions.15–17
Although the real reason why patients from municipalities furthest from a hospital have fewer admissions is unknown, we believe that this may fundamentally be due to two reasons: firstly because patients who live closest to hospitals tend to make greater use of hospital emergency services, thereby increasing the probability of admission; and secondly, because patients who live further away tend to face greater difficulty when it comes to being transferred to hospital, so that the primary care physician may try to control the patient on an ambulatory basis until such a time as admission becomes essential. The differences found in RRs in relation to the rurality index may be linked to distance to hospital, since it is precisely the rural municipalities that are situated furthest away.
The relative risk of admission per unit of the standardised prevalence ratio was 0.37 (95% CI 0.34–0.41) for men and 0.39 (95% CI 0.34–0.45) for women. This means that more women than men are admitted to hospital. These are standardised figures and, therefore, both the age structure and the distribution by sex of each municipality are taken into account.
Municipal COPD prevalence was 5% in men and 2% in women. These differences are in line with the literature. Part of this difference is due to the fact that the main risk factor is smoking.18 This prevalence is lower than that reported in other studies conducted in Spain.2 It should be borne in mind, however, that comparability with published studies is somewhat complicated, owing to the great variability that exists in terms of the designs, diagnostic criteria and age ranges used. This was in fact highlighted in Rycroft et al's review, which reported figures ranging from 0.2% to 37% among the different countries.19 The EPi-SCAN study conducted in Spain from 2006 to 2007 observed a prevalence of 10.2% using the Global Initiative for Chronic Obstructive Lung Disease (GOLD).2 This study, unlike ours, had an observational-cross-sectional design, was population-based, and used a random selection of participants (for study purposes). It was a multicentre study, which had an area in common with ours. In this area, the EPi-SCAN study estimated a prevalence of 8.2% with the GOLD criteria, whereas we observed a prevalence of 4.1%. This difference can be explained in great measure by the high rate of underdiagnosis.20 Indeed, the EPi-SCAN study estimated that this area had a COPD underdiagnosis rate of 69%, something that would support our results.2 These differences can also be explained by the fact that COPD prevalence in our study is based on cases which showed up for primary care attention (in principle, symptomatic cases) and not on wide-based spirometric findings. Therefore, underdiagnosis of COPD in general population might be present but should not affect the correlation with hospital admissions since we expect it to be homogeneous among Galician municipalities.
It is important to implement programmes which serve to reduce underdiagnosis and improve early detection of cases.21 In this connection, some studies urge wider use and availability of spirometry in primary care in order to enhance diagnosis of COPD.22
A total of 33.78% of patients with COPD required a minimum of one admission in 2013, with there being considerable variability among the different municipalities. This variability could be reduced by implementing and improving programmes targeted at early diagnosis of patients with COPD, as well as exacerbation-prevention measures.23
Our data enabled us to ascertain which municipalities had a higher or lower risk of admissions (data not shown). Strategies or factors that contribute to lower hospitalisation rates in some areas should be studied, so as to be able to apply these in areas that maintain a high percentage of admissions.
This study has a series of advantages, the principal of which is that it covered the entire population of Galicia, so that no selection bias should be present. This in turn allows for robust estimates. A second advantage lies in the use of two independent information systems that enabled indicators to be obtained. The third advantage relates to the techniques used in the analysis, in that numerous socio-demographic variables of adjustment as well as distance to hospital were included, thus making it possible to obtain results with a lower likelihood of bias. Similarly, the number of diagnoses of COPD was introduced into the model in the form of an SPR, thereby taking the age structure of the respective municipalities into account. Furthermore, risks were smoothed in accordance with the characteristics of neighbouring municipalities. The fourth advantage lies in the use of municipality as the level of aggregation, since this is a sufficiently small geographical unit to allow for the prevailing environmental and homogeneous socio-economic exposures in each study area to be taken into account.
However, this study also displays a series of limitations. Firstly, the case data were exclusively sourced from public health care. Even so, we feel that this would not seriously affect calculations, since public health care in Galicia accounts for 97% of the total. The second limitation relates to the registration of primary care data. The data came from information recorded by different observers (individual primary care physicians), which might pose a reporting bias. For study purposes, compliance with COPD case reporting was assumed to be uniform across the different municipalities of Galicia. It is less likely that such bias would occur in the MBDS, since far fewer people are tasked with coding these records. In addition, among the different hospitals coding is presumably more uniform, due to the specific training received by the people doing this job. In general, we feel that the information available gives a fairly accurate picture of the current status of COPD in Galicia. Thirdly, we do not know the percentage of COPD admissions on total hospital admissions. Nevertheless, since all hospitals cover areas with similar age distribution, we should expect no differences in the burden of COPD admissions between hospitals. In addition, epidemic peaks due to other diseases (i.e. influenza) that could affect the greater or lesser likelihood of admission due to COPD occur simultaneously in all hospitals because they belong to the same region. We do not have information about the characteristics of hospital admissions, however we do not believe that this affects the results. Finally, we have not performed a sensitivity analysis including only COPD as a primary diagnosis, we do not believe that this is a bias because the number of patients with other primary diagnoses different from COPD is proportional in the different municipalities.
ConclusionsIn conclusion, this study has observed that there is a significant negative association between prevalence of COPD and hospital admissions due to this disease, and also that there are fewer COPD admissions from municipalities situated furthest away from hospitals. Finally, there is wide variability, not only in the prevalence of COPD, but also in the number of COPD admissions at a municipal level, something that reflects the importance of giving in-depth attention to disease-management training programmes, particularly for older patients. Moreover, early diagnosis must be encouraged to combat the high rate of underdiagnosis that exists at present. This study also highlights the enormous potential utility of current health information systems for analysing the epidemiology and management of diseases such as COPD, in addition to many others.
FundingThis study did not receive competitive funding.
Conflicts of interestNone.
We are grateful to the Galician Health Service for having provided us with all the data necessary to perform the present work.