After the first description in China, Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) spread all over the world, reaching also the poorest countries of sub-Saharan Africa. Despite several authors and organizations raising issues and fears about the potentially devastating effects of SARS-CoV-2 in Africa and unpreparedness of African Health Systems to face Coronavirus Disease 2019 (COVID-19),1 the real effects in this continent are far from being established.
COVID-19 is posing several challenges in the richest areas of the world which were unable to deal promptly with shortages of intensive care units, health personnel and personal protective equipment2 leading to hundreds of thousands of severe outcome and deaths.
Whereas, in Africa, while COVID-19 cases and deaths are increasing, other major killers are still there. Tuberculosis (TB) is still the number-one infectious disease killer in the world and containing it during the COVID-19 pandemic is seriously at risk.
Appropriate TB management comprises prompt diagnosis of active TB cases, identification of people exposed and infected people, access to treatment and drug-adherence control. With the rising number of multidrug-resistant TB (MDR), direct observed therapy (DOT) is pivotal to ensuring that people regularly take medications. For appropriate care, a close link between the health centres and patients is needed. However, after the arrival of COVID-19 in Africa, this connection is at risk.
Several African countries are declaring lockdown to prevent contagions. In poor settings, quarantine has heavy economic implications and people are losing their daily income. For most families, this generates difficulties in paying transport fees to reach health centres. In Sierra Leone, the government allowed health facilities to provide patients with enough TB medication for weeks, aiming to reduce movement and flatten the COVID-19 curve. This may lead to low treatment adherence with potential consequences for TB cure rates, development of drug resistant TB and spread in the community.
Importantly, many sub-Saharan peripheral health centres are experiencing a reduction in clinical visits.3 Matilda Yamba, a community health worker from Bureh Town, Sierra Leone, declared that “people do not seek medical care for two reasons: they are either scared of getting SARS-CoV-2 infection in the health facilities, or are scared of being diagnosed with it”. Africa knows well the social stigma associated with infectious diseases, HIV and TB being historical models, and it is not unexpected to be scared of being recognized as COVID-19 patients and blamed for spreading the virus in the community.4
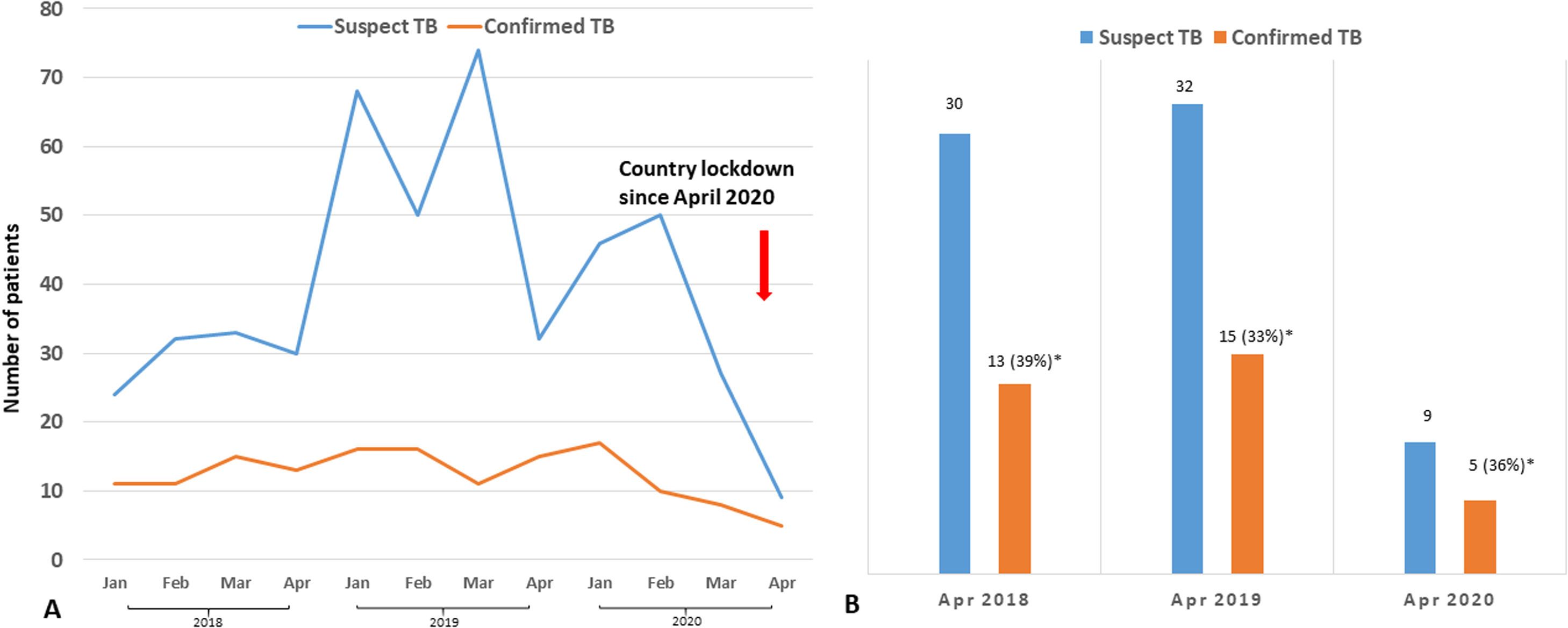
To understand the impact of COVID-19 on TB care, we evaluated the gross numbers of patients assessed for presumptive TB in the Community Health Post of Tombo, a village of Western Rural Area in Sierra Leone, with a government recognized TB outpatient unit, referral for an area of about 5000 people. Presumptive TB patients undergo sputum smear for Acid Fast Bacilli (AFB) and receive free TB-medications if the diagnosis is confirmed. We collected the number of patients tested and confirmed AFB-positive during the first 4 months of the year 2020 (January, February, March, April), and compared it with the cases reported in 2018 and 2019. The study was approved by the authorities for the TB unit of the local health centre (J.S.B.).
In Sierra Leone, the first COVID-19 presumptive cases were documented at the end of March 2020 and lockdown declared in April 2020. On May 6th, 225 COVID-19 cases and 14 deaths were confirmed by the government in Sierra Leone.
As shown in Fig. 1, on April 2020, a significant drop of confirmed TB cases was documented. Also, the number of TB presumptive cases, that might have other respiratory diseases, gradually decreased in March and April 2020. Similarly, no DOTs were administered in April 2020. No cases of COVID-19 and TB co-infections have been detected. Although our study has several limitations, due to its retrospective and descriptive nature and reference to a specific epidemiological area, this is the first description of an indirect impact of COVID-19 on TB care in a low-resource high-TB burden setting. Conversely, it is difficult to obtain data about TB in children during this pandemic. In poor, peripheral settings, paediatric TB is diagnosed on a clinical basis according to medical history and clinical assessment, since children are not able to expectorate and gastric lavages cannot be performed. For this reason, paediatric TB has been historically considered a neglected condition, since it is difficult to obtain microbiological identification of the disease and children, who usually have a paucibacillary illness, do not significantly spread the infection. Since in poor settings they are usually evaluated after an adult member is diagnosed with active TB, now, with the COVID-19 pandemic and ongoing restrictive measures, child TB is disappearing. Paradoxically, now, children with TB may be at risk of being forgotten, not only neglected.
Number of presumptive TB and confirmed TB cases in Tombo Health Centre, Sierra Leone. While a stable trend in TB diagnosis during the first months of 2018, 2019 and 2020 was observed (a), a significant drop was reported in April 2020 (b), after lockdown was declared by the government. * Proportion of TB cases over the total patients enrolled as “presumptive TB patients” coming to the outpatient TB unit of Tombo, Western Rural Area, Sierra Leone.
In this context, the International Community is called on to provide massive support to poor countries. Before COVID-19, African health systems were struggling to provide appropriate care, although improvements have been made since the last Ebola outbreak. Now, Africa is not only having to face the historical enemies, but has to deal with both the direct costs of COVID-19 and the indirect consequences of COVID-19. While rich countries are now gaining more experience about the direct effects of COVID-19 on human health, the consequences on the major killers in poor countries are far from being understood. Here, endemic diseases that can present with symptoms similar to COVID-19 (TB, measles, pneumococcal disease and others), must not be forgotten.5 Importantly, in these settings where advanced forms of TB frequently occur and are caused by drug-resistant strains of M. tuberculosis, higher mortality rates due to both TB and COVID-19 can be expected in young individuals.6,7 Africa needs support not only to strengthen promptness of response to COVID-19 pandemic in hospitals and health centres but also appropriate communication strategies, basic instruments for telemedicine, economic support for patients and healthcare workers, are all needed tools to guarantee TB care. Otherwise, all results achieved in recent years in the fight against TB, may be lost.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Delia Goletti is a professor at Saint Camillus International University of Health and Medical Sciences in Rome.
We are grateful to all our colleagues that supported the development of local health services and training of community health workers in the Western Rural Area of Sierra Leone and, in particular, Ismail Jaber, Matilda Yamba, Prince Williams, Memunatu N. Kallon, Nee Turay, Pietro Sollena, Francesca Vassallo, Vittorio Sabatino, Mara Caramia, Gregory Leeb, Valeria Pansini, Filippo Bruno, Andrea Deidda, Arianna Cafarotti, Davide Guglielmi, Maria Giulia Conti, Jessica Balerna, Francesco Madeddu, Mattia Belardinelli, Daniele Barbuto, Luigi Torricelli, Rachel Mannings, Surf4Children Onlus.
The study was partially supported by the Italian Ministry of Health, Ricerca Corrente Linea 1 and 3.