Computed tomography (CT) guided transthoracic lung biopsy (TTLB) is a well established method in the diagnosis of intra-thoracic lesions with good diagnostic yield.1 Pneumothorax is the most frequent complication with an incidence varying between 8% and 64%.2
The objective of this study was to evaluate potential risk factors associated with the occurrence of pneumothorax in CT-guided TTLB. We performed a retrospective study of patients undergoing CT-guided TTLB between 2007 and 2012 in Braga Hospital. Clinical data and radiologic images of patients were reviewed.
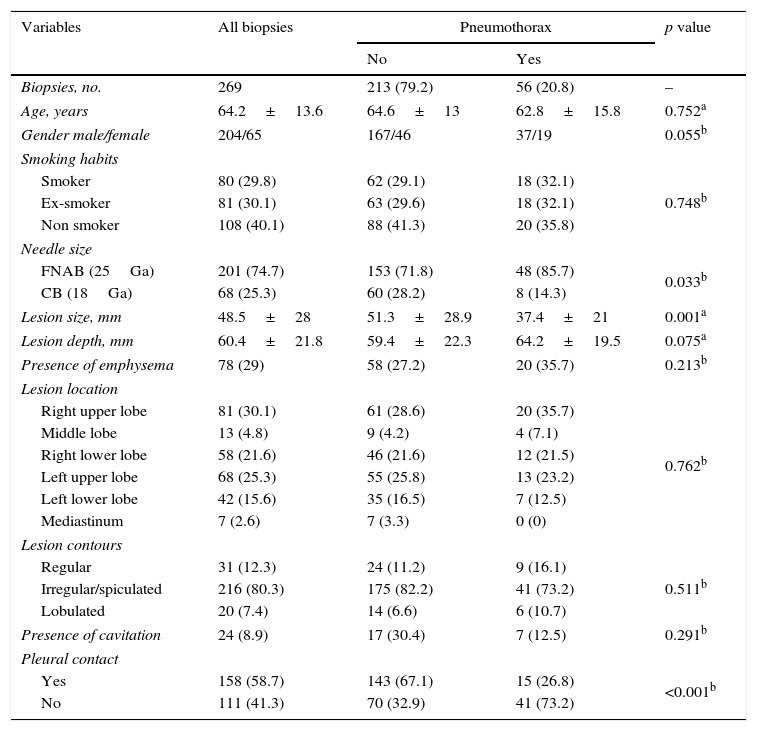
A total of 269 TTLB were performed (201 fine needle aspiration biopsies and 68 core biopsies), in 209 patients with a mean age of 64.2 years, 75.8% male, 60% with smoking habits. Pneumothorax rate was 20.8%. Treatment of pneumothorax with chest drainage was necessary in 10/269 biopsies (3.7%). An initial univariate analysis identified the following risk factors: larger needle size (p=0.033), smaller size of the lesion (p=0.001) and absence of pleural contact (p<0.001) – Table 1. A multiple logistic regression analysis has identified absence of pleural contact (p<0.001; R2 adjusted 0.107) and size of the lesion (p=0.030; R2 adjusted 0.120) as significant independent risk factors for the occurrence of pneumothorax. Pneumothorax occurred in 41/111 (36.9%) biopsies in lesions without pleural contact vs 15/158 (9.5%) with pleural contact. Pneumothorax rate for lesions ≤2cm was 31% compared with 15.4% for lesions >4cm. Age, gender, smoking habits, presence of emphysema, needle size, presence of cavitation, contours, location and depth of lesion were not significantly associated with increased risk of pneumothorax.
Univariate analysis of demographic characteristics of patients and multiple variables of TTLB.
| Variables | All biopsies | Pneumothorax | p value | |
|---|---|---|---|---|
| No | Yes | |||
| Biopsies, no. | 269 | 213 (79.2) | 56 (20.8) | – |
| Age, years | 64.2±13.6 | 64.6±13 | 62.8±15.8 | 0.752a |
| Gender male/female | 204/65 | 167/46 | 37/19 | 0.055b |
| Smoking habits | ||||
| Smoker | 80 (29.8) | 62 (29.1) | 18 (32.1) | 0.748b |
| Ex-smoker | 81 (30.1) | 63 (29.6) | 18 (32.1) | |
| Non smoker | 108 (40.1) | 88 (41.3) | 20 (35.8) | |
| Needle size | ||||
| FNAB (25Ga) | 201 (74.7) | 153 (71.8) | 48 (85.7) | 0.033b |
| CB (18Ga) | 68 (25.3) | 60 (28.2) | 8 (14.3) | |
| Lesion size, mm | 48.5±28 | 51.3±28.9 | 37.4±21 | 0.001a |
| Lesion depth, mm | 60.4±21.8 | 59.4±22.3 | 64.2±19.5 | 0.075a |
| Presence of emphysema | 78 (29) | 58 (27.2) | 20 (35.7) | 0.213b |
| Lesion location | ||||
| Right upper lobe | 81 (30.1) | 61 (28.6) | 20 (35.7) | 0.762b |
| Middle lobe | 13 (4.8) | 9 (4.2) | 4 (7.1) | |
| Right lower lobe | 58 (21.6) | 46 (21.6) | 12 (21.5) | |
| Left upper lobe | 68 (25.3) | 55 (25.8) | 13 (23.2) | |
| Left lower lobe | 42 (15.6) | 35 (16.5) | 7 (12.5) | |
| Mediastinum | 7 (2.6) | 7 (3.3) | 0 (0) | |
| Lesion contours | ||||
| Regular | 31 (12.3) | 24 (11.2) | 9 (16.1) | 0.511b |
| Irregular/spiculated | 216 (80.3) | 175 (82.2) | 41 (73.2) | |
| Lobulated | 20 (7.4) | 14 (6.6) | 6 (10.7) | |
| Presence of cavitation | 24 (8.9) | 17 (30.4) | 7 (12.5) | 0.291b |
| Pleural contact | ||||
| Yes | 158 (58.7) | 143 (67.1) | 15 (26.8) | <0.001b |
| No | 111 (41.3) | 70 (32.9) | 41 (73.2) | |
Data presented as mean±SD or no. (%).
In our study, the absence of pleural contact was the most significant risk factor associated with the occurrence of post-TTLB pneumothorax. These data were corroborated by another retrospective study of Khan et al.3 in which lesions in the lung parenchyma had a higher pneumothorax rate than lesions located in the pleura or thoracic wall. Another significant risk factor identified was lesion size. There seems to be a gradual increase in the risk of pneumothorax to progressively smaller lesions. In a retrospective analysis of 660 biopsies, Yeow et al.4 showed that the risk of pneumothorax was about 11 times higher in lesions ≤2cm than in lesions >4cm.
In conclusion, this study supports the performance of CT-guided TTLB in the study of undetermined lung lesions as a safe method. Although the overall incidence of pneumothorax was 20.8%, the clinically significant pneumothorax rate requiring treatment with chest tube drainage was low (3.7%).
AuthorshipJoão Filipe Cruz conceived this study, collected the data and carried out the statistical analysis. Rui Rolo collected the data, collaborated in the inception of the study and supervised all aspects of its implementation. Lourdes Iglésias and João Cunha contributed to the critical revision of the manuscript. All the authors contributed to the interpretation of the results and the proof reading of the manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare.