Early diagnosis is necessary for the success of the tuberculosis (TB) program. Goal: To identify factors associated with diagnosis delay of TB in Huambo, Angola.
Material and methodsCross-sectional study carried out in patients diagnosed with TB at the Huambo Anti-Tuberculosis Dispensary (ATD) in the period between October 2015 and January 2016.
ResultsThe 247 patients included in the analysis had a median age of 27 years and a median diagnosis delay of 64 days. In the univariate analysis, age, consumption of alcoholic beverages, living in a residence further than 10km from a healthcare unit, and looking for any other health unit than the emergency unit were associated with longer diagnosis delay. In the multivariate analysis model, to be between 30 and 44 years of age (p=0.018), to live in a residence more than 10km from a healthcare unit (p=0.006) and to turn to traditional medicine as the first healthcare option (p<0.001) were factors that led to greater time delay before diagnosis.
ConclusionsIn the Huambo province, age, distance to healthcare facility and the first healthcare service consulted were associated with diagnosis delay of TB.
Tuberculosis (TB) is a public health problem that affects millions of people worldwide1 especially in sub-Saharan Africa where the burden of TB is greater.2 For an effective TB control program it is essential to obtain early diagnosis, immediately begin appropriate treatment and ensure its continuity.3
Time delay in the diagnosis of TB plays an important role in the increase of infectivity, mortality risk and transmission of the disease in the community.4,5 It is estimated that an untreated patient with positive microscopy for TB bacillus can infect, on average, 10–15 community contacts within a year.6
The factors that contribute to the time delay in the diagnosis and treatment of TB may be related to the patient himself as well as the healthcare service.7–12 Sex, age, educational level, occupation, distance from home to the healthcare institution, co-morbidities and poor knowledge about TB, were some of the factors related to the patient.13–16 Lack of diagnosis resources, such as chest radiology, negative microscopy result, waiting time and the first healthcare unit consulted were associated to the system delay.8,10,15–17
In Angola, TB is one of the main reasons for visits to healthcare services. In 2015, the incidence of TB was 93 per 100,000 inhabitants.18 In 1981, the Angolan Ministry of Health established the National Tuberculosis Program (NTP), whose priority was the establishment of TB diagnosis and treatment services throughout the country.8 Huambo province is located on the central plateau of Angola, with an area of 35,771km2 and 2,019,555 inhabitants, corresponding to 7.8% of the total population of the country, according to the final results of the population census of 2014.19 The province's healthcare network consists of 11 municipal hospitals, 1 General/Provincial hospital, 1 Sanatorium hospital, 1 Anti-Tuberculosis Dispensary (ATD), 50 healthcare centers and 165 health posts (report from the provincial directorate of health, 2016). For the diagnosis and treatment of TB, the province has 12 outpatient units, some of which are linked to municipal hospitals. In these units, pulmonary TB diagnosis is based on sputum microscopy performed on three patient-provided samples, clinical history and chest radiography. For extrapulmonary TB (EPTB), the diagnosis is based on microscopy of biological products depending on the infected organ or only on the symptoms of the disease, the clinical history and the radiography, at the doctor's discretion. Patients with criteria for hospitalization due to complications of TB or requiring further intervention are referred to the sanatorium hospital, since it is the reference unit. Patients without criteria for hospitalization are directed to the ATD. Treatment is provided under directly observed treatment (DOT) during the intensive phase. In the maintenance phase, the patient is entrusted to a relative.
The Sanatorium hospital, with its ambulatory dependency ATD, is considered the reference center for TB in the region. The Sanatorium Hospital/ATD possesses a bacteriology laboratory for microscopy exams and a radiology section.
The Huambo province has a regional mycobacteriology laboratory that performs culture tests and antibiotic sensitivity tests (TSA) in the case of a negative microscopy, therapeutic failures or resistance to antibiotics in the Central South region.
The purpose of this study was to identify the factors associated with TB diagnosis delay in the population of Huambo, Angola.
MethodologyStudy designCross-sectional study including patients diagnosed with TB in the Huambo ATD, between October 2015 and January 2016.
Inclusion and exclusion criteriaAll patients diagnosed with TB of all forms, who appeared in the Huambo ATD, at the time of application of the questionnaires, participated in the survey regardless the time of treatment. Included in this study (new and previous treatment) are all ages and both gender. Patients without complete information for the time delay variable were excluded from the analysis.
Place of studyThe study was conducted at the ATD, and at the Sanatorium Hospital of Huambo.
Data collectionData was collected through the distribution of questionnaires. Patient files and TB treatment cards were also reviewed. A questionnaire was developed for data collection and filled out by the patients at the time of their monthly follow-up appointments and by hospitalized patients if they were diagnosed in the study period. This task was performed over the course of 22 days by the technicians working in the TB area, who received a specific training seminar by the researcher. Patients were individually questioned in a closed environment on the unit's premises, to maintain patient privacy, after the clarification on the study and informed consent. The questionnaire included socio-demographic information, risk factors for the disease and clinical characteristics. The clinical information was collected in the patients’ files as well as some additional sociodemographic information contained therein, obtained before and after to survey.
Sample464 patients were diagnosed during the study period and 353 responded to the survey. Of the subjects surveyed, 247 patients were selected for this study.
Definition of variablesThe diagnosis of TB refers to the recognition by health workers of an active case, to a patient with current disease due to M. tuberculosis.20
Diagnosis delay was defined as the time between the onset of signs and symptoms of TB and the diagnosis (patient delay+healthcare delay).
In the municipality variable patients were split into those who lived in Huambo city and those who lived outside, including the other ten municipalities of the Huambo province and those from other provinces in Angola.
Age was categorized into four classes: <15 years, 15–29 years, 30–44 years and >45 years. Occupation was defined as regular occupation and included individuals with fixed employment, retired (since they have regular pensions) and students. Individuals without fixed employment or with irregular services such as street vendors, peasants and others were considered as having non-regular occupation.
The clinical presentation of TB was defined as pulmonary and extrapulmonary TB.
Statistical analysisUnivariate and multivariate linear regressions were performed with the response being the logarithmic transformation of the time delay. For the multivariate analysis the complete model was determined based on a selection of variables, using the stepwise regression method that minimizes the AIC (Akaike Information Criterion). All data analysis was performed with R version 3.3.2 software and p-value <0.05 was considered significant.
Ethics approvalThe study was approved by the General Directorate of the Sanatorium Hospital of Huambo, Angola and the Ethics Committee of the São João Hospital Center and the Faculty of Medicine of the University of Porto, Portugal.
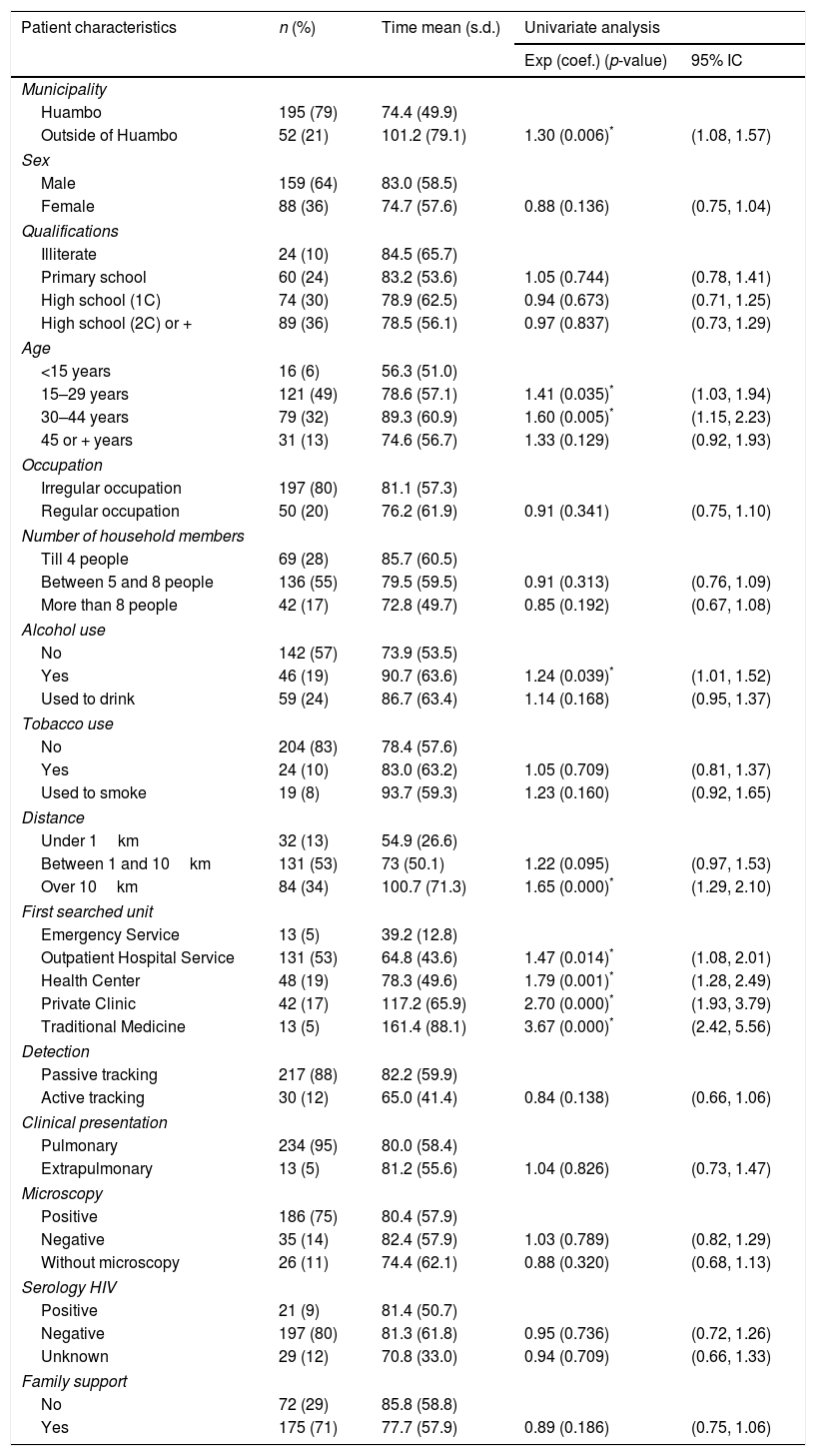
ResultsOf the 353 respondents, 247 patients were included in this study. Their median age was 27 years old, 159 (64%) were males, 197 (80%) had irregular occupations, 136 (55%) had a household size of 5–8 people, 151 (57%) patients did not consume alcoholic beverages and 204 (83%) did not smoke (Table 1).
Sociodemographic and clinical characteristics associated with the time delay until TB diagnosis in the Huambo Province, Angola.
| Patient characteristics | n (%) | Time mean (s.d.) | Univariate analysis | |
|---|---|---|---|---|
| Exp (coef.) (p-value) | 95% IC | |||
| Municipality | ||||
| Huambo | 195 (79) | 74.4 (49.9) | ||
| Outside of Huambo | 52 (21) | 101.2 (79.1) | 1.30 (0.006)* | (1.08, 1.57) |
| Sex | ||||
| Male | 159 (64) | 83.0 (58.5) | ||
| Female | 88 (36) | 74.7 (57.6) | 0.88 (0.136) | (0.75, 1.04) |
| Qualifications | ||||
| Illiterate | 24 (10) | 84.5 (65.7) | ||
| Primary school | 60 (24) | 83.2 (53.6) | 1.05 (0.744) | (0.78, 1.41) |
| High school (1C) | 74 (30) | 78.9 (62.5) | 0.94 (0.673) | (0.71, 1.25) |
| High school (2C) or + | 89 (36) | 78.5 (56.1) | 0.97 (0.837) | (0.73, 1.29) |
| Age | ||||
| <15 years | 16 (6) | 56.3 (51.0) | ||
| 15–29 years | 121 (49) | 78.6 (57.1) | 1.41 (0.035)* | (1.03, 1.94) |
| 30–44 years | 79 (32) | 89.3 (60.9) | 1.60 (0.005)* | (1.15, 2.23) |
| 45 or + years | 31 (13) | 74.6 (56.7) | 1.33 (0.129) | (0.92, 1.93) |
| Occupation | ||||
| Irregular occupation | 197 (80) | 81.1 (57.3) | ||
| Regular occupation | 50 (20) | 76.2 (61.9) | 0.91 (0.341) | (0.75, 1.10) |
| Number of household members | ||||
| Till 4 people | 69 (28) | 85.7 (60.5) | ||
| Between 5 and 8 people | 136 (55) | 79.5 (59.5) | 0.91 (0.313) | (0.76, 1.09) |
| More than 8 people | 42 (17) | 72.8 (49.7) | 0.85 (0.192) | (0.67, 1.08) |
| Alcohol use | ||||
| No | 142 (57) | 73.9 (53.5) | ||
| Yes | 46 (19) | 90.7 (63.6) | 1.24 (0.039)* | (1.01, 1.52) |
| Used to drink | 59 (24) | 86.7 (63.4) | 1.14 (0.168) | (0.95, 1.37) |
| Tobacco use | ||||
| No | 204 (83) | 78.4 (57.6) | ||
| Yes | 24 (10) | 83.0 (63.2) | 1.05 (0.709) | (0.81, 1.37) |
| Used to smoke | 19 (8) | 93.7 (59.3) | 1.23 (0.160) | (0.92, 1.65) |
| Distance | ||||
| Under 1km | 32 (13) | 54.9 (26.6) | ||
| Between 1 and 10km | 131 (53) | 73 (50.1) | 1.22 (0.095) | (0.97, 1.53) |
| Over 10km | 84 (34) | 100.7 (71.3) | 1.65 (0.000)* | (1.29, 2.10) |
| First searched unit | ||||
| Emergency Service | 13 (5) | 39.2 (12.8) | ||
| Outpatient Hospital Service | 131 (53) | 64.8 (43.6) | 1.47 (0.014)* | (1.08, 2.01) |
| Health Center | 48 (19) | 78.3 (49.6) | 1.79 (0.001)* | (1.28, 2.49) |
| Private Clinic | 42 (17) | 117.2 (65.9) | 2.70 (0.000)* | (1.93, 3.79) |
| Traditional Medicine | 13 (5) | 161.4 (88.1) | 3.67 (0.000)* | (2.42, 5.56) |
| Detection | ||||
| Passive tracking | 217 (88) | 82.2 (59.9) | ||
| Active tracking | 30 (12) | 65.0 (41.4) | 0.84 (0.138) | (0.66, 1.06) |
| Clinical presentation | ||||
| Pulmonary | 234 (95) | 80.0 (58.4) | ||
| Extrapulmonary | 13 (5) | 81.2 (55.6) | 1.04 (0.826) | (0.73, 1.47) |
| Microscopy | ||||
| Positive | 186 (75) | 80.4 (57.9) | ||
| Negative | 35 (14) | 82.4 (57.9) | 1.03 (0.789) | (0.82, 1.29) |
| Without microscopy | 26 (11) | 74.4 (62.1) | 0.88 (0.320) | (0.68, 1.13) |
| Serology HIV | ||||
| Positive | 21 (9) | 81.4 (50.7) | ||
| Negative | 197 (80) | 81.3 (61.8) | 0.95 (0.736) | (0.72, 1.26) |
| Unknown | 29 (12) | 70.8 (33.0) | 0.94 (0.709) | (0.66, 1.33) |
| Family support | ||||
| No | 72 (29) | 85.8 (58.8) | ||
| Yes | 175 (71) | 77.7 (57.9) | 0.89 (0.186) | (0.75, 1.06) |
The median diagnosis delay was 64 days (IQR: 37–95 days).
In the univariate analysis, living outside of Huambo (p=0.006), being aged between 15 and 29 (p=0.035) or 30–44 (p=0.005), consuming alcoholic beverages (p=0.039) and living in a residence more than 10km from a healthcare unit (p=0.001) were associated with longer diagnosis delay. Using the emergency unit as a reference, it was found that the patients who first sought out any other healthcare unit took more time until diagnosis (p≤0.014) (Table 1).
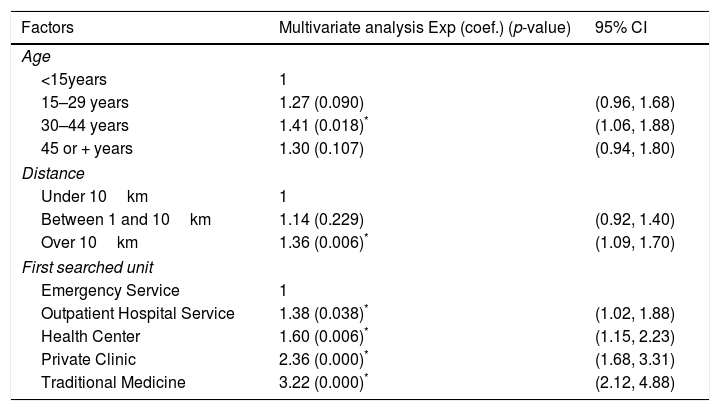
The multivariate analysis model indicated that individuals aged between 30 and 44 years (p=0.018), living at a distance greater than 10km from a healthcare unit (p=0.006), and not going to the emergency unit, especially if they first used traditional medicine (p<0.001), had longer diagnosis delay (Table 2).
Factors associated with the time delay until TB diagnosis in the Huambo Province, Angola.
| Factors | Multivariate analysis Exp (coef.) (p-value) | 95% CI |
|---|---|---|
| Age | ||
| <15years | 1 | |
| 15–29 years | 1.27 (0.090) | (0.96, 1.68) |
| 30–44 years | 1.41 (0.018)* | (1.06, 1.88) |
| 45 or + years | 1.30 (0.107) | (0.94, 1.80) |
| Distance | ||
| Under 10km | 1 | |
| Between 1 and 10km | 1.14 (0.229) | (0.92, 1.40) |
| Over 10km | 1.36 (0.006)* | (1.09, 1.70) |
| First searched unit | ||
| Emergency Service | 1 | |
| Outpatient Hospital Service | 1.38 (0.038)* | (1.02, 1.88) |
| Health Center | 1.60 (0.006)* | (1.15, 2.23) |
| Private Clinic | 2.36 (0.000)* | (1.68, 3.31) |
| Traditional Medicine | 3.22 (0.000)* | (2.12, 4.88) |
One hundred and six patients were excluded from the analysis because they did not know the date of the onset of their symptoms, which meant that the time delay until the diagnosis could not be calculated. The median age of these patients was 25 years and 75 (71%) were male. Excluded patients differed from the included ones especially in tobacco use (lower proportion of non-smokers, p=0.005), qualifications (higher proportion of illiterate and primary educated, p<0.001) and the first healthcare unit sought (higher proportion of Health Center and Emergency Service, p<0.001).
DiscussionIn this study the time delay of 247 diagnosed patients at the Huambo ATD, between October 2015 and January 2016 was evaluated.
The median diagnosis delay was 64 days. Our findings do not differ from other studies in Nepal,21 Ethiopia,10 India,12 Yemen,22 and Zambia23 where the median delay was 60–63 days. On the other hand, Tanzania24 had a considerably longer median time of 136 days and Portugal25 a shorter one of 36 days. A previous study conducted in Luanda, Angola, had a median diagnosis delay of 45 days.8 The factors associated with delaying the diagnosis of TB may be different between Huambo and Luanda, considering the greater concentration of the population in the country's capital (72% living in urban area).
In the univariate analysis, we found that living outside of Huambo city, being between 15 and 29 or 30–44, consuming alcoholic beverages, living in a residence more than 10km from a healthcare unit and seeking health care outside of the emergency service system were associated with longer diagnosis delay.
Based on the multivariate analysis results encountered, belonging to the 30–44 years old age group was associated with a longer time delay until diagnosis. Age has been associated with diagnosis delay in other studies.9,10,14–16,24,25 Several social factors such as work schedule and difficulty in organizing working time to visit healthcare services have been given as explanations for a greater delay in this age group.15
Regarding the distance to the healthcare service, in the studies carried out in Ethiopia and Tanzania, the patients who lived more than 10km away from the healthcare institutions had a longer time delay until the diagnosis of TB, when compared to those living within a 10km radius.17,24 Other studies have found a relationship between longer walking distance to a healthcare facility and patient delay in Nepal,14 Nigeria,16 Odisha, India11 and south India.12 These studies corroborate our findings, in which the distance from the healthcare service was considered a factor in diagnosis delay due to unavailability and lack of access to TB diagnosis and treatment units in rural areas.
The first healthcare service consulted was identified as the risk factor for longest delay until diagnosis, particularly if it was a private clinic or a traditional healer. Though most patients (78.9%) lived in the Huambo municipality, we cannot say whether the demand for these units is attributable to patients living in rural or urban areas. Although the number of patients that consulted the health center (17%) and traditional healer (5%) is low, there is a longer delay time. Similar results were also verified in the previous study in Luanda. This was also confirmed in previous studies, where longer diagnosis delays were obtained when private healthcare facilities and traditional healers,11,12,17,24,26 were the first healthcare unit used. On the other hand, in the Huambo province, poor availability and accessibility of the primary health care, lack of public transport for some communities and socioeconomic conditions of the patients can be considered in the diagnosis delay.
Our study had some limitations. It was performed in an area with insufficient resources. Patients who appeared at the weekend were not questioned. Other limitations of our study were mainly related to the exclusion of the population that did not remember the date of the onset of their symptoms. However, despite the fact that the excluded patients differ in their smoking habits, literary qualifications and first healthcare unit used, there were no differences between the two groups in any of the other analyzed variables that were significant in the diagnosis delay. We cannot exclude memory bias in the responses. We assume that the delay time was calculated based on the dates declared by the patients, which may have been subject to error.
Despite the limitations presented, the strengths of this study are relevant. The study was carried out in the reference unit that covers the region, with good adherence and it is the first study on TB diagnosis delay in the Huambo province.
ConclusionIn the Huambo province, age, distance to healthcare units and the first healthcare service used were associated with tuberculosis diagnosis delay. To reduce delays and improve access to health care, efforts should be made to expand public health institutions in rural communities, to decentralize health services. The government, via Ministry of Health, should create policies involving the private sector in TB care. This will provide a key basis for TB control and health coverage for people living in areas of poor access. The community should also be informed on how to recognize the symptoms of TB through lectures, and healthcare professionals should be better trained, in order to reduce the patient's delay time until diagnosis and initiate treatment as early as possible, interrupting TB transmission.27 Although sputum microscopy is the favoured method used in the province, new diagnostic techniques like Xpert MTB/Rifampin should be implemented, because they contribute to the rapid diagnosis and effective detection of TB disease and drug resistance.28,29
Conflicts of interestThe authors have no conflicts of interest to declare.
Our thanks go to the Erasmus Mundus DREAM project for the scholarship granted. We also thank the collaboration of the Provincial Directorate of Health, General Direction of the Hospital Sanatorio of Huambo, for the permission for this study and to the collaborators: Marcos Nguvulo, Esmeralda Santos, Jack Osvaldo and Georgina Tavares. Ó. Felgueiras was partially supported by CMUP (UID/MAT/00144/2013), which is funded by FCT with national (MCTES) and European structural funds through the programs FEDER, under the partnership agreement PT2020.