Pulmonary sequestration (PS) is a rare congenital malformation. Several reports describe preoperative diagnostic difficulties with this pathology.1–3 The authors report a case of intralobar sequestration (IS) and intend to draw attention to the importance of imaging modalities, including Computed Tomography (CT) with contrast for the diagnosis, in order to reduce the number of patients sent for surgery without an accurate diagnosis.
IS corresponds to 75–90% of all sequestrations consisting of non-functioning lung tissue that falls within the normal lung parenchyma without its own visceral pleura; it is usually unrelated to the tracheobronchial tree. It is irrigated by an abnormal systemic artery derived mainly from the aorta. About 20% of cases are irrigated by more than one artery.1–3
IS presents frequently in adolescents and young adults, but rarely in adults over 40 years, with recurrent infection and hemoptysis; 15% of patients are asymptomatic.1,2
The diagnosis is suggested by the identification of the abnormal blood vasculature in imaging studies. The average rate of reported preoperative misdiagnosis in the literature is high. Angiography used to be considered the method of choice for preoperative diagnosis, has been replaced by non-invasive methods. Conventional CT does not consistently show anomalous arterial supply. Thus, CT with contrast has emerged as the imaging test of choice.1–5
Surgical resection is the treatment of choice.1,2
Case report: Female patient, Caucasian, 64 years old, house cleaner, no smoking or alcohol habits. Referred for pulmonology evaluation because she had asthenia and adynamia with one-year evolution, weight loss (13kg in six months), a CT showing fibrosis areas, traction bronchiectasis and an encysted and loculated left pleural effusion.
In relation to antecedents, the key was anaemia of unknown cause and an episode of respiratory infection which dragged on (one year ago). She did not report any hemoptysis episodes.
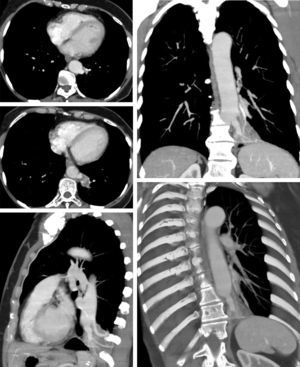
A thoracic CT with contrast was performed and showed a vascular image in the internal basal segment of the left lower lobe, 47mm×47mm, with at least two arteries originating from the lower thoracic aorta; this was suggestive of PS. There were also fibrosis areas and bronchiectasis (Fig. 1).
A left lower lobectomy was performed and the anomalous arteries were joined up. An anatomopathological examination showed a cavitary formation of 5cm, with apparent communication with the bronchial tree and pulmonary condensation of the surrounding parenchyma. Microscopically, this was a cystic lesion lined with respiratory epithelium; adjacent to this, there were many dilated and mucous retention airspaces, tortuous blood vessels and wall thickening, which are consistent with IS.
A diagnostic hypothesis suggested from the first CT (without contrast) was encysted pleural effusion. The performance of CT with contrast was central to the correct diagnosis of preoperative PS.
In this case, the highlights are the unusual age of onset of clinical presentation, nonspecific and uncharacteristic symptomatology, PS irrigated by two arteries and communication with the tracheobronchial tree.