Diffuse or metastatic pulmonary calcification is a rare entity of unknown etiology, associated with a wide variety of benign and malignant processes.1
In 1855 Virchow first described metastatic pulmonary calcification. It is usually associated with phosphocalcic metabolism or pH alterations, both at a systemic and local level. Its most common cause is chronic kidney disease (CKD), but other causes include hyperparathyroidism, renal transplantation, hypervitaminosis D, and malignant diseases such as myeloma.2
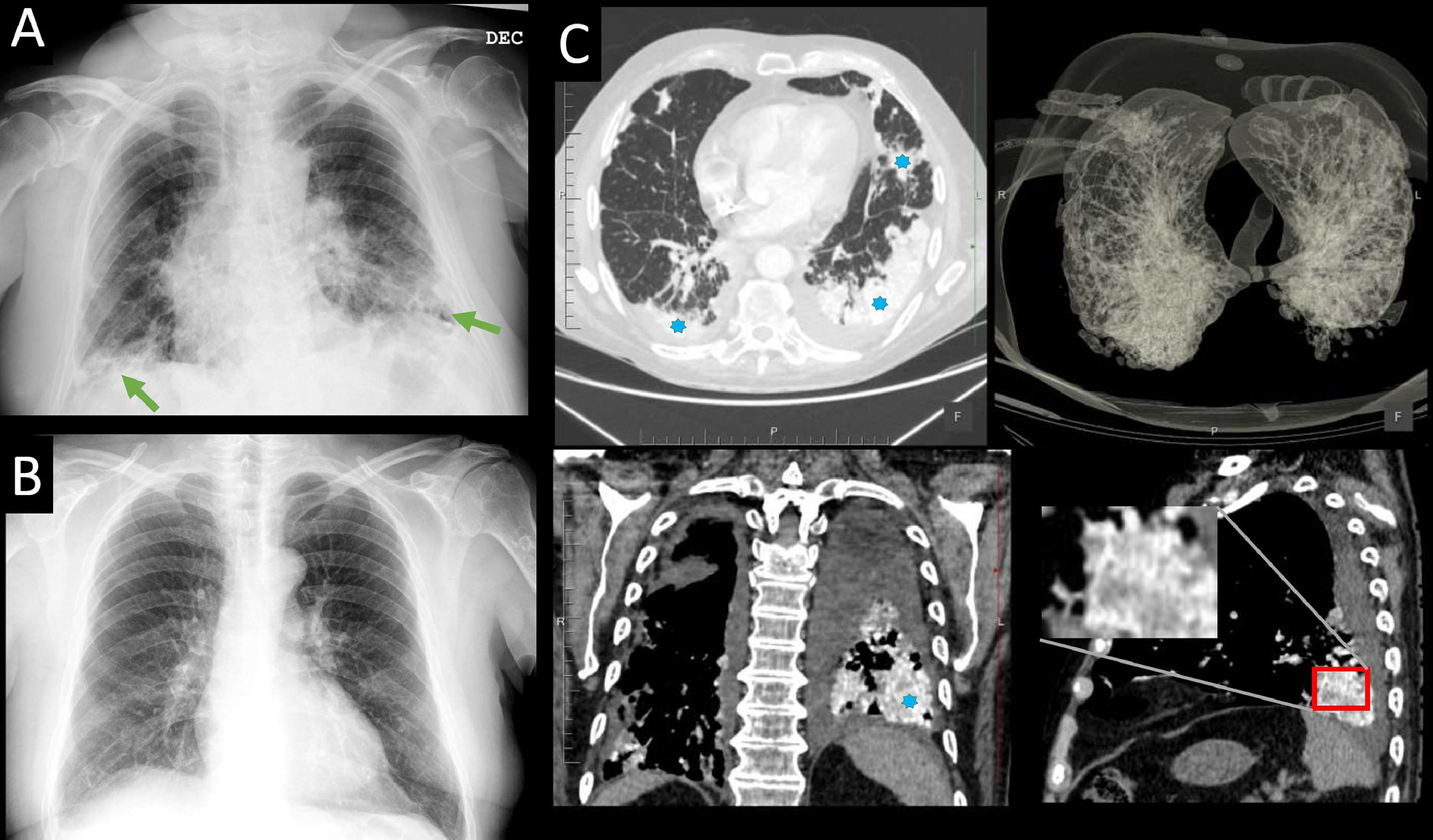
We present the case of a 79-year-old male, non-smoker, who had been a marble worker for fifty years. He had a history of CKD with a histological diagnosis of membranoproliferative glomerulonephritis. He presented to the emergency department with dyspnea, cough, and fever, so a chest X-ray was taken showing a bibasal alveolointerstitial pattern (Fig. 1A), not present in the radiological study performed two years earlier (Fig. 1B). With the suspicion of bacterial pneumonia, antibiotic treatment was administrated without success. During admission his kidney function worsened, requiring hemodialysis. Given the persistence of dyspnea and hypoxemia, a CT pulmonary angiogram was performed. There was no evidence of embolism, but the study showed confluent and markedly hyperdense condensations of bibasal predominance (Fig. 1C).
(A) Chest X-ray performed at the Emergency room showing a bibasal alveolointerstitial pattern (green arrows). (B) Previous X-ray without those findings. (C) CT pulmonary angiogram in axial (up and left), coronal (down left), and sagittal (down right) planes with a 3D-VR reconstruction of the airway (up and right), showing confluent and markedly hyperdense condensations of bibasal predominance (asterisks) because of metastatic calcification.
Phosphocalcic metabolism abnormalities, hyperparathyroidism, or hypervitaminosis D were ruled out. Therefore, based on both clinical and radiological evidence, the diagnosis was metastatic pulmonary calcification in the context of CKD undergoing hemodialysis.
Metastatic calcification appears as a metabolic disorder in which calcium deposits accumulate in tissues outside their usual location.3 Several factors have been implicated in its etiology, although it can also affect patients with normal phosphocalcic metabolism,4 as in this case.
The lung is one of the main sites of metastatic calcium deposition, predominantly in the alveolar walls but also the bronchial wall, pulmonary arteries, and veins.4 In autopsy series, metastatic calcification has been shown in 60–80% of hemodialysis patients,5 although it is rarely detected during the patient's life.
Metastatic pulmonary calcification is a frequently asymptomatic and underdiagnosed condition.5 It should be suspected when dialysis patients develop radiographic changes or unexplained respiratory symptoms,5 which include dyspnea and nonproductive cough. The degree of respiratory distress often does not correlate with the amount of macroscopic calcification.1
Although its evolution and prognosis are generally favorable, it can sometimes progress to irreversible alveolar damage and respiratory failure.3 Visceral calcifications usually persist despite treatment, which is none other than suppressing predisposing factors.2
Since chest radiography is not sensitive enough to demonstrate small amounts of calcium,3 high-resolution computed tomography (HRCT) is the most sensitive and effective test for diagnosing this entity,3,4 and lung biopsy is rarely used.2 Three possible patterns of calcification are described on HRCT: diffusely distributed nodules, patchy areas of ground-glass opacity, and lobular distributed parenchymal consolidation areas.4