This retrospective cohort study was conducted in two teaching hospitals over a 3-month period (March 2010–June 2020) comparing severe and critical COVID-19 patients admitted to Respiratory Intensive Care Unit for non-invasive respiratory support (NRS) and subjected to awake prone position (PP) with those receiving standard care (SC). Primary outcome was endotracheal intubation (ETI) rate. In-hospital mortality, time to ETI, tracheostomy, length of RICU and hospital stay served as secondary outcomes. Risk factors associated to ETI among PP patients were also investigated.
ResultsA total of 114 patients were included, 76 in the SC and 38 in the PP group. Unadjusted Kaplan–Meier estimates showed greater effect of PP compared to SC on ETI rate (HR = 0.45 95% CI [0.2−0.9], p = 0.02) even after adjustment for baseline confounders (HR = 0.59 95% CI [0.3−0.94], p = 0.03). After stratification according to non-invasive respiratory support, PP showed greater significant benefit for those on High Flow Nasal Cannulae (HR = 0.34 95% CI [0.12−0.84], p = 0.04). Compared to SC, PP patients also showed a favorable difference in terms of days free from respiratory support, length of RICU and hospital stay while mortality and tracheostomy rate were not significantly different.
ConclusionsProne positioning in awake and spontaneously breathing Covid-19 patients is feasible and associated with a reduction of intubation rate, especially in those patients undergoing HFNC. Although our results are intriguing, further randomized controlled trials are needed to answer all the open questions remaining pending about the real efficacy of PP in this setting.
The Severe Acute Respiratory Syndrome CoronaVirus 2 (SARS-CoV-2) pandemic infection has dramatically increased the number of patients admitted to hospital who developed pneumonia and acute respiratory failure (ARF) (COVID-19 disease) to be treated with non-invasive ventilatory support.1,2 Although potentially beneficial and safe for trained healthcare operators,3 non-invasive respiratory support (NRS) still presents high failure rates (27–90%),1–6 particularly in patients complicating with acute respiratory distress syndrome (ARDS) (20–41%).7,8 When ceiling of treatment is excluded, upgrade to endotracheal intubation (ETI) and mechanical ventilation (MV) may be required to assist these patients, rapidly saturating the availability of intensive care unit (ICU) beds and potentially leading to increased mortality.6
Innovative approaches such as awake prone position (PP) have been therefore considered to improve the performance of NIRS in COVID-19 pneumonia, in order to spare ICU resource utilization and to reduce mortality. The ultimate guidelines from the European Society of Intensive Care Medicine suggest using PP for at least 12 h in patients with COVID-19 and moderate to severe ARDS subjected to MV9 with the aim of reducing lung ventilation/perfusion mismatching and shunt fraction and to improve hypoxemia.10 Evidence from non-COVID19 ARDS patients have showed that due to gravitational effects and anatomical shape matching of the lung to the thoracic cavity, PP relieves the dependent lung regions from the compressive forces exerted by heart weight, improves lung aeration from dorsal to ventral areas, generates a more uniform strain distribution, and enhances lung perfusion.11,12
To date, small studies conducted in patients with ARF and assisted with non-invasive ventilation (NIV) or High Flow Nasal Cannulae (HFNC) showed that PP improves oxygenation and reduces the rate of ETI.13,14 In non-intubated patients with COVID-19 pneumonia, preliminary findings demonstrated only physiological benefits (increase in oxygenation or a decrease in respiratory rate and/or dyspnea) following awake PP was associated to NRS.15–22
Although the available evidence is weak and mainly reports physiological advantages deriving from the PP strategy under MV, it might be arguable that at least a selected subset of spontaneously breathing COVID-19 patients are going to obtain significant clinical gains from PP. With this retrospective multicenter analysis we aimed at investigating the potential clinical benefits following early awake PP under NRS in a cohort of patients with severe and critical COVID-19 pneumonia.
Materials and methodsStudy setting and designThis retrospective, multicenter observational cohort study was carried out in the Respiratory Intensive Care Units (RICUs) of the University Hospitals of Modena (Italy) and Bologna (Italy). The study has been approved by the regional Ethical Committee of Emilia Romagna (CE N. 453/2020 and 715/2020) and trial registered on clinicaltrial.gov (number: NCT04649658).
Patients selection and case definitionAll patients aged 18 ≥ 80 year admitted to both RICUs for severe/critical COVID-19 pneumonia between March 1st and June 1st 2020 were selected. SARS-CoV2 infection was confirmed by PCR method with nasopharyngeal swab. COVID-19-related pneumonia was defined as severe by the presence of a respiratory rate (RR) ≥30 breaths per minute (bpm), peripheral blood oxygen saturation (SaO2) ≤93%, PaO2/FiO2 ratio <300 mmHg breathing room air, and lung infiltrates >50% of the lung filed early at admission,23,24 and critical according to criteria of either WHO25 and the National Health Commission of China24 for COVID-19-induced ARDS which aligns with the Berlin Definition.26
Patients with endotracheal intubation (ETI) performed within the first 24-h from admission, ceiling of escalation, do not intubate (DNI) order as expressed by patient’s will or upon clinical judgement, missing core data at medical record analysis (i.e. clinical characteristics at baseline, pronation data, type and time of ventilatory support, mortality, need for tracheostomy, length of RICU and hospital stay) were not considered for analysis.
Patients included were then divided into two groups: (1) those undergoing awake PP maneuvers (PP) in addition to standard care; (2) those performing standard care only (SC).
Standard careStandard of care was in agreement with the Italian Society of Infectious Diseases’ Guidelines (SIMIT)27 and started shortly after admission. This included:
- -
oxygen supply and (NRS) to target SaO2 > 90%;
- -
hydroxychloroquine (400 mg bis in die (BID) on day 1 followed by 200 mg BID on days 2–5 eventually adjusted for creatinine clearance estimated by a chronic kidney disease algorithm);
- -
azithromycin (500 mg daily for 5 days) at physician’s discretion when suspecting a bacterial respiratory superinfection;
- -
low molecular weight heparin for prophylaxis of deep vein thrombosis according to body weight and renal function unless counterndicated.
A proportion of patients received off-label treatment with Tocilizumab,28,29 a recombinant humanized monoclonal antibody of the IgG1 class directed against both the soluble and membrane-bound forms of the interleukin-6 (IL-6) receptor. NRS were adopted using an inspiratory fraction of delivered oxygen (FiO2) increased up to a target transcutaneous oxyhemoglobin saturation >90%. Settings of each NRS have been adjusted by the attending physician based on the continuous monitoring of the cardiorespiratory parameters and included:
- -
Non-invasive ventilation (NIV) with patients connected through a conventional circuit with a sized oronasal mask (BluestarTM, KOO Medical Equipment, Shanghai, PRC) to a high-performance ventilator (GE Healthcare Engstrom CarestationTM, GE Healthcare, Finland or Mindray SynoVent E3, Mindray Medical, Italy) in pressure support pre-set mode. Positive end expiratory pressure (PEEP) was initially set at 8 cmH2O and subsequently fine-tuned according to clinical parameters and ventilator waveforms. Pressure support (PS) was set at 10 cmH2O, and then progressively modified, according to tidal volume, waveforms, and respiratory drive.
- -
High Flow Nasal Cannulae (HFNC) with patients connected to a high flow device (Optiflow™and AIRVO™, Fisher & PaykelHealthcare Ltd, Auckland, New Zealand) deliveredoxygen through different sized nasal cannulae. Flow delivery was initially set at 60 L/min and temperature at 37 °C then adjusted according to the patient’s tolerance.
- -
Continuous Positive Airway Pressure (CPAP) with patients were connected through a helmet interface (Helmet Starmed, Intersurgical SpA, Mirandola, Italy) designed for pandemics. PEEP was initially set at 8 cmH2O and subsequently fine-tuned according to clinical parameter. This was obtained by connecting a blender system to the available oxygen source to achieve adequate FiO2 levels.
Once admitted to RICU a non-randomly subset of patients enrolled was subjected to early awake PP in addition to the standard care. In particular, PP treatment was assigned to consecutive patients in the charge of two specific physicians when they were on duty at the RICUs (namely, RT in Modena and VC in Bologna), given their experience in pronation maneuvers. Patients assigned to all the other doctors were instead submitted to standard care. PP treatment was started soon after admission. Patients eligible for PP were aged 18–80 years and had been admitted to RICU with indication for NRS therapy, whereas exclusion criteria for pronation were those previously reported by Coppo et al.19 Thos eligible were taught by RICU staff on how to achieve PP and then encouraged to maintain pronation for at least 3 -h before being helped back to supine in bed. However, they were free to resume their supine position or to maintain pronation at their own discretion. Number of daily PP sessions varied from a minimum of 1 to a maximum of 4 based on the physician’s judgment and/or the patient’s preference.
Covariate variablesChart review, medical record, and archived data collection wereconductedin each center. The following variables were then inserted into an electronic database: demographics, relevant comorbidities, clinical characteristics (arterial blood gases-PaO2/PaCO2/pH, PaO2/FiO2 ratio, respiratory rate-RR, blood lactate level, dyspnea grade by BORG scale, mean arterial pressure-MAP), laboratory tests (blood count, renal function, C-reactive protein-CRP, procalcitonin-PCT, D-dimer) on admission, type and duration of required NRS, rate and time of ETI, mortality, need for tracheostomy, length of RICU and hospital stay. Radiographic appearance on available computed tomography (CT) scan performed on admission was assessed by an expert radiologist blinded to the study purpose. Radiographic presentation of COVID-19 lung involvement was classified according to the number of lobes involved, the presence of bilateral abnormalities, the predominant distribution (diffuse, peripheral, patchy) and the main pattern (interstitial versus consolidative).
Outcome variablesPrimary purpose was to evaluate the impact of awake PP on ETI rate in patients with severe and critical COVID-19 pneumonia admitted to RICU to be assisted with NRS. In both hospitals the decision as to whether proceed to ETI was taken according to the best clinical practice by the attending staff. Criteria for ETI included: (a) PaO2/FiO2 ratio unchanged or worsened despite use of NRS, (b) need to protect airways due to neurological deterioration or massive secretions, (c) hemodynamic instability or major electrocardiographic abnormalities, (d) unchanged or worsened dyspnea and persistence of respiratory distress despite NRS (i.e. RR > 35 bpm, gasping for air, psychomotor agitation requiring sedation, abdominal paradox). Secondary scope was to compare time to ETI, mortality, NRS-free-days (i.e. days spent without HFNC, NIV, CPAP, or invasive mechanical ventilation at 1-month), tracheostomy, length of RICU and hospital stay between PP and SC groups. Furthermore, potential risks (among the epidemiological, clinical and radiographic factors) associated to ETI were investigated in the PP group.
Statistical analysisSample size calculation was performed assuming an estimated ETI rate of 70% for the study cohort1,30 and a presumed reduction by 40% in those receiving pronation (data derived from an exploratory analysis in 30 patients). Assuming α = 0.05, power 80% and an enrollment ratio of 1:2 (proportion of patients subjected to pronation or to standard care, respectively) a sample of 93 patients was considered sufficient to confidently perform analysis on the primary outcome.
To test whether baseline covariates were balanced and did not significantly affect treatment a post-hoc propensity score was allocated. We ran logistic regression using prone position as the dependent variable with all baseline features as covariates. Propensity scores were obtained by calculating the fitted value from the logistic model for each patient and then comparing, showing that allocation to treatment was not significantly affected by baseline condition (Fig. S1, supplementary material). Baseline characteristics were compared in PP and SC groups; continuous variables were expressed as median and interquartile ranges (IQR) and compared by t test and Wilcoxon-Mann–Whitney test, whereas categorical variables were reported as numbers and percentages (%) and compared by χ2 test or Fisher’s exact test.
The time to ETI analysis was performed with participants’ follow-up accrued from the date of admission until ETI. Time to ETI was compared using unweighted Kaplan–Meier curves and analyzed through a cumulative incidence function model using Fine-Grey competing risk model31 with baseline fixed covariates considering mortality as competing risk. The effect of pronation on ETI was shown by means of unadjusted and adjusted hazard ratio (HR) with 95%CI. Age, PaO2/FIO2 ratio, pH value and respiratory rate were identified as 4 key confounders, and then used for adjustment. In order to test the hypothesis that the difference between groups might vary according to the type of NRS, we formally included an interaction term in the Fine-Grey regression model. Results were then showed after categorizing the population into two strata using categorical separation. The association of the two different treatments with pre-specified secondary outcomes was further carried out through Fisher’s exact test and Wilcoxon–Mann–Whitney test.
In patients undergoing PP univariate and multivariate logistic regression were then performed to detect predictors of ETI among all of the available factors recorded at admission.
The time course of PaO2/FiO2 ratio before and after pronation according to ETI within the first 7 days from RICU admission was assessed through ANOVA analysis. Then a post-hoc Bonferroni-Dunn’s multiple test was used to perform the pairwise comparison of means for each group.
A two-sided test of less than 0.05 was considered statistically significant. Statistics were performed using SPSS version 25.0 (IBM Corp.New York, NY, USA) and Graphpad prism version 8.0 (Graphpad Software, Inc. La Jolla, Ca, USA) unless otherwise indicated.
ResultsPopulationOne-hundred-fourteen patients were included 1:2 in the analysis (38 PP: 76 SC) among all those patients diagnosed with severe and critical COVID-19 and referred to the two RICUs over the period considered. Study chart is shown in Fig. S2 (Supplementary material).
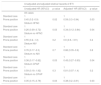
Epidemiological, clinical and respiratory characteristics are presented in Table 1. The vast majority of patients were male (70%) and more than a third of them presented ARDS (37%), while the median PaO2/FIO2 ratio was 149 (78–232) mmHg. Time from disease onset to admission was comparable between the two groups (median 8 [4–12] days for PP and 9 [4–13] for SC, p = 0.5).
General and clinical features of the study population presented as a whole and according to prone position manoeuvre.
| Variable | Overall | Standard care (SC) | Prone position (PP) | p value |
|---|---|---|---|---|
| n = 114 (100) | n = 76 (67) | n = 38 (38) | ||
| Age, years (IQR) | 67 (32−80) | 70 (33−80) | 61 (32−75) | 0.03 |
| Male sex, n (%) | 80 (70) | 55 (73) | 25 (66) | 0.5 |
| Smoker, n (%) | 33 (29) | 22 (29) | 11 (29) | 0.9 |
| BMI, Kg/m2 | 27.5 (19−37) | 28 (20−37) | 26 (19−36) | 0.3 |
| SAPS II, score (IQR) | 25 (12−46) | 25 (12−41) | 27 (14−46) | 0.4 |
| APACHE II, score (IQR) | 10 (4−22) | 10 (4−20) | 11 (4−22) | 0.7 |
| SOFA, score (IQR) | 4 (2−7) | 4 (2−6) | 4 (2−7) | 0.8 |
| Time from disease onset to RICU admission, days (IQR) | 9 (4−13) | 9 (4−13) | 8 (4−12) | 0.5 |
| ARDS, n (%) | 42 (37) | 30 (39) | 12 (32) | 0.6 |
| Comorbidities | ||||
| Systemic hypertension, n (%) | 92 (81) | 60 (79) | 32 (84) | 0.6 |
| COPD, n (%) | 17 (15) | 11 (15) | 6 (16) | 0.9 |
| ILD, n (%) | 3 (3) | 2 (2) | 1 (3) | 0.9 |
| Asthma, n (%) | 3 (3) | 2 (2) | 1 (3) | 0.9 |
| Cancer, n (%) | 12 (11) | 8 (11) | 4 (11) | 0.9 |
| Ischemic heart disease, n (%) | 16 (14) | 10 (13) | 6 (16) | 0.8 |
| Type 2 diabetes, n (%) | 22 (19) | 14 (18) | 8 (23) | 0.6 |
| Arrhythmia, n (%) | 17 (15) | 12 (16) | 5 (13) | 0.8 |
| Renal failure, n (%) | 10 (9) | 8 (10) | 2 (6) | 0.7 |
| Immunodeficiency, n (%) | 10 (9) | 6 (8) | 4 (10) | 0.9 |
| Hepatitis, n (%) | 8 (7) | 4 (5) | 4 (10) | 0.4 |
| Charlson index, score (IQR) | 2 (0−9) | 2 (0−9) | 2 (0−8) | 0.9 |
| Symptoms on admission | ||||
| Fever, n (%) | 110 (96) | 74 (98) | 36 (94) | 0.3 |
| Cough, n (%) | 55 (48) | 34 (45) | 21 (55) | 0.4 |
| Dyspnea, n (%) | 108 (95) | 71 (94) | 36 (94) | 0.9 |
| Fever + cough, n (%) | 55 (48) | 37 (48) | 18 (48) | 0.9 |
| Fever + dyspnea, n (%) | 106 (93) | 70 (92) | 36 (94) | 0.9 |
| Cough + dyspnea, n (%) | 49 (40) | 34 (45) | 15 (39) | 0.7 |
| Fever + cough + dyspnea (%) | 49 (40) | 34 (45) | 15 (39) | 0.7 |
| Physiological parameters on RICU admission | ||||
| Dyspnea, BORG scale score (IQR) | 5 (1−10) | 5 (1−10) | 6 (2−10) | 0.7 |
| Kelly, score (IQR) | 1 (1−2) | 1 (1−2) | 1 (1−2) | 0.9 |
| Body T, °C (IQR) | 37.4 (36.0–39.6) | 36.9 (36.0–39.2) | 37.4 (36–39.6) | 0.3 |
| RR, bpm (IQR) | 29 (15−45) | 27 (15−40) | 34 (18−46) | 0.02 |
| HR, bpm (IQR) | 95 (50−140) | 96 (51−125) | 95 (50−140) | 0.7 |
| MAP, mmHg (IQR) | 93 (77−113) | 94 (85−113) | 91 (77−103) | 0.1 |
| pH, value (IQR) | 7.46 (7.30–7.58) | 7.45 (7.30–7.56) | 7.47 (7.31–7.58) | 0.02 |
| PaCO2, mmHg (IQR) | 32 (20–72) | 32 (22–72) | 32 (20–62) | 0.3 |
| PaO2/FIO2, mmHg (IQR) | 149 (78–232) | 153 (84–232) | 141 (73–223) | 0.03 |
| HCO3−, mmol/L (IQR) | 21 (19−28) | 21.2 (20.8−28.3) | 19.8 (18.7−27.6) | 0.1 |
| Lactate, mmol/L (IQR) | 1.4 (1−2) | 1.3 (1−2) | 1.6 (1−2) | 0.9 |
| Non-invasive support | ||||
| HFNC, n (%) | 69 (61) | 46 (61) | 23 (61) | 0.9 |
| CPAP, n (%) | 25 (22) | 16 (21) | 9 (23) | 0.9 |
| NIV, n (%) | 19 (17) | 13 (17) | 6 (16) | 0.9 |
| Pharmacological treatment | ||||
| Systemic steroids, n (%) | 80 (70) | 55 (73) | 25 (66) | 0.5 |
| Hydroxychloroquine, n (%) | 94 (82) | 64 (84) | 30 (79) | 0.8 |
| Azithromycin, n (%) | 74 (65) | 47 (62) | 28 (71) | 0.3 |
| Heparin (Prophylactic dose), n (%) | 57 (50) | 35 (46) | 22 (58) | 0.3 |
| Heparin (Treatment dose), n (%) | 46 (40) | 33 (43) | 13 (34) | 0.4 |
| Lopinavir/ritonavir, n (%) | 26 (23) | 17 (22) | 9 (24) | 0.9 |
| Darunavir/cobicistat, n (%) | 24 (21) | 18 (24) | 5 (16) | 0.2 |
| Tocilizumab, n (%) | 41 (36) | 29 (38) | 12 (32) | 0.5 |
| Laboratory tests | ||||
| White cells count, n*109/L (IQR) | 7.4 (2.1–24.9) | 7.5 (2.7–22.2) | 6.8 (2.1–24.9) | 0.5 |
| Hemoglobin, g/L (IQR) | 12.5 (5.1–17.4) | 13.0 (5.1–17.4) | 12.4 (7.3–15.4) | 0.3 |
| Lymphocytes, 109/L (IQR) | 1.08 (0.06–20.0) | 1.0 (0.1–12.0) | 1.3 (0.1–20.0) | 0.1 |
| Platelets, 109/L (IQR) | 210 (80–472) | 220 (80–472) | 179 (116–318) | 0.4 |
| C-Reactive Protein, mg/dL (IQR) | 5.9 (0.1–36.4) | 6.1 (0.2–35.4) | 4.8 (0.1–36.4) | 0.4 |
| D-Dimer, µg/L (IQR) | 2.16 (0.28–15.0) | 1.89 (0.29–15.0) | 3.90 (0.28–12.1) | 0.1 |
| Albumin, g/L (IQR) | 32 (14–56) | 31 (14–45) | 32 (23–56) | 0.1 |
| LDH, U/L (IQR) | 333 (144–982) | 318 (144–964) | 355 (179–982) | 0.1 |
| BUN, mg/dl (IQR) | 35 (16–132) | 35.5 (16.0–132.0) | 32.5 (23.0–68.0) | 0.3 |
| Creatinine, mg/dl (IQR) | 0.9 (0.3–4.7) | 0.92 (0.6–4.7) | 0.85 (0.27–2.02) | 0.2 |
Data are presented as number and percentage for dichotomous values or median and interquartile range (IQR) for continuous values.
Abbreviations: IQR = inter quartile range; COPD = chronic obstructive pulmonary disease; ILD = interstitial lung disease; RR = respiratory rate; HR = heart rate; MAP = mean arterial pressure, ARDS = acute respiratory distress syndrome; APACHE II = acute physiology and chronic health evaluation II score; SAPS II = simplified acute physiology score; SOFA = subsequent organ failure assessment score, HFNC = high flow nasal cannula; CPAP = continuous positive airways pressure; NIV = non-invasive mechanical ventilation; LDH = lactic dehydrogenase; BUN = blood urea nitrogen.
Patients in the PP group came out significantly younger than in SC (61 VS 70 years old, p = 0.03), while no differences were observed in terms of severity scores, comorbidities and biochemical markers. PP patients showed a worse PaO2/FIO2 ratio, higher RR and pH value at baseline. No inter-groups difference was observed in the received standard treatment, in either drugs or NRS.
No adverse events were reported when proning maneuvers were applied to these patients.
OutcomesOverall ETI rate was 32.5%; 7 (18%) and 30 (39.5%) patients were subjected to MV in PP and SC groups respectively. Time to ETI did not differ between groups (5 [3–5] days and 4 [3–5] days for PP and SC, p = 0.7). Unadjusted Kaplan–Meier estimates (supplementary Figure 3, panel A) and Cox regression analysis showed the beneficial effect of PP compared with SC on ETI (HR = 0.45 95CI [0.2−0.92], p = 0.02). After adjusting for the key confounders, results again confirmed the group difference (HR = 0.59 95CI [0.3−0.94], p = 0.04); however, the stratified analyses showed that this difference varied according to the use of NRS even after adjusting confounders (Table 2).In particular, awake PP significantly reduced the risk of ETI in patients undergoing HFNC, but not NIV or CPAP.
Hazard ratios from fitting a Fine-Grey regression model.
| Unadjusted and adjusted relative hazards of ETI | ||||
|---|---|---|---|---|
| Unadjusted HR (95%CI) | p value | Adjusted* HR (95%CI) | p value | |
| All cases | ||||
| Standard care | 1 | 1 | ||
| Prone position | 0.45 (0.2−0.9) | 0.02 | 0.59 (0.3−0.94) | 0.03 |
| Stratum HFNC | ||||
| Standard care | 1 | 1 | ||
| Prone position | 0.26 (0.09−0.72) | 0.03 | 0.34 (0.12−0.84) | 0.04 |
| Stratum no HFNC | ||||
| Standard care | 1 | 1 | ||
| Prone position | 0.55 (0.2−1.3) | 0.2 | 0.6 (0.6−1.81) | 0.4 |
| Stratum NIV | ||||
| Standard care | 1 | 1 | ||
| Prone position | 0.76 (0.17−3.3) | 0.7 | 0.86 (0.35−3.9) | 0.8 |
| Stratum no NIV | ||||
| Standard care | 1 | 1 | ||
| Prone position | 0.38 (0.17−0.82) | 0.03 | 0.43 (0.27−0.93) | 0.04 |
| Stratum CPAP | ||||
| Standard care | 1 | 1 | ||
| Prone position | 0.59 (0.18−1.92) | 0.3 | 0.81 (0.07−1.4) | 0.2 |
| Stratum no CPAP | ||||
| Standard care | 1 | 1 | ||
| Prone position | 0.35 (0.15−0.79) | 0.03 | 0.38 (0.2−0.81) | 0.03 |
Data are presented as HR and 95% CI.
Abbreviations: HR = hazard ratio; CI = confidence interval; ETI = endotracheal intubation, HFNC = high flow nasal cannula; CPAP = continuous positive airways pressure; NIV = non-invasive mechanical ventilation.
Tracheostomy and mortality rate were similar (p = 0.4 and p = 0.4) between PP and SC; Kaplan–Meier curve analysis did not show any difference in 30-day survival between groups (Fig. S3, panel B). Number of days free from NRS was higher (20 and 15 days respectively, p = 0.03), and length of stay in RICU (10 vs 15 days, p = 0.02) and in hospital (20 vs 24 days, p = 0.03) were shorter in PP than in SC group at 30-day. See the overall results in Table 3.
Clinical outcomes of the study population presented as a whole and according to prone position manoeuvre.
| Outcome | Cohort | OR | p-value | ||
|---|---|---|---|---|---|
| Total | Standard care | Prone position | |||
| n = 114 | n = 76 | n = 38 | |||
| 30 days mortality, n (%) | 22 (19) | 17 (23) | 5 (13) | 0.5 (0.2−1.6) | 0.4 |
| Respiratory support free days at day 30, n (IQR) | 17 (2−24) | 15 (2−22) | 20 (2−24) | – | 0.03 |
| Tracheostomy, n (%) | 21 (18) | 16 (21) | 5 (13) | 0.6 (0.2−1.8) | 0.4 |
| RICU stay, days (IQR) | 13 (3−26) | 15 (3−26) | 10 (3−21) | – | 0.02 |
| Hospital stay days, n (%) | 23 (3−45) | 24 (3−45) | 20 (3−41) | – | 0.03 |
The data are presented as a numbers and percentage value for dichotomic variables and as median and interquartile ranges for continuous variables. The statistical significance was set for p < 0.05.
OR = odds ratio; IQR = interquartile range; RICU = respiratory intensive care unit.
Table 4 reports the results derived from the univariate and the multivariate analysis in patients proned. In the univariate analysis, those patients proned and intubated were older, had a higher prevalence of ARDS, maintained awake proning for less time/day, showed greater perceived dyspnea, mainly received NIV, and displayed a diffuse distribution of lung CT scan abnormalities. In the multivariate analysis, less time spent when proning, presence of ARDS, use of NIV, and diffuse pattern at chest CT scan were factors independently associated with ETI.
General and clinical features of the PP cohort according to ETI and associated risk.
| Variable | No ETI | ETI | Univariate OR | 95%CI | p value | Multivariate | 95%CI | p value |
|---|---|---|---|---|---|---|---|---|
| n = 31 (82) | n = 7 (18) | OR | ||||||
| Age, years (IQR) | 60 (34−68) | 70 (52−75) | 1.8 | 1.4−7.9 | 0.03 | |||
| Male sex, n (%) | 20 (65) | 5 (71) | 1.4 | 0.2−7.7 | 0.9 | |||
| Smoker, n (%) | 9 (29) | 2 (29) | 1 | 0.2−5.5 | 0.9 | |||
| BMI, Kg/m2 | 25.6 (19−31) | 27.7 (22−35) | 1.5 | 0.2−8.9 | 0.6 | |||
| SAPS II, score (IQR) | 25 (12−40) | 28 (14−46) | 1.8 | 0.3−21 | 0.4 | |||
| APACHE II, score (IQR) | 10 (4−21) | 13 (4−22) | 1.4 | 0.4−12 | 0.5 | |||
| SOFA, score (IQR) | 4 (2−6) | 4 (2−7) | 1.2 | 0.1−15 | 0.8 | |||
| ARDS, n (%) | 7 (23) | 5 (71) | 8.6 | 1.2−47 | 0.02 | 3 | 1.3−21 | 0.04 |
| Time from disease onset to RICU admission, days (IQR) | 8 (4−11) | 8 (4−12) | 1.1 | 0.2−8 | 0.8 | |||
| Prone position time/day, hours (IQR) | 6 (1−12) | 3 (1−5) | 0.4 | 0.3−0.8 | 0.02 | 0.7 | 0.2−0.9 | 0.04 |
| Comorbidities | ||||||||
| Systemic hypertension, n (%) | 26 (84) | 6 (86) | 1.2 | 0.2−16 | 0.9 | |||
| COPD, n (%) | 5 (16) | 1 (14) | 0.9 | 0.1−6.5 | 0.9 | |||
| ILD, n (%) | 1 (4) | 0 (0) | 0.01 | 0−40 | 0.9 | |||
| Asthma, n (%) | 1 (4) | 0 (0) | 0.01 | 0−40 | 0.9 | |||
| Cancer, n (%) | 3 (10) | 1 (14) | 1.6 | 0.1−12 | 0.9 | |||
| Ischemic heart disease, n (%) | 5 (16) | 1 (14) | 0.9 | 0.1−6.5 | 0.9 | |||
| Type 2 diabetes, n (%) | 7 (23) | 1 (14) | 0.6 | 0.04−4.3 | 0.9 | |||
| Arrhythmia, n (%) | 4 (12) | 1 (14) | 1.2 | 0.1−9.1 | 0.9 | |||
| Renal failure, n (%) | 1 (3) | 1 (14) | 5 | 0.3−97 | 0.3 | |||
| Immunodeficiency, n (%) | 3 (10) | 1 (14) | 1.6 | 0.1−12 | 0.9 | |||
| Hepatitis, n (%) | 3 (10) | 1 (14) | 1.6 | 0.1−12 | 0.9 | |||
| Charlson index, score (IQR) | 2 (0−8) | 2 (0−8) | 1 | 0.3−6 | 0.9 | |||
| Symptoms on admission | ||||||||
| Fever, n (%) | 30 (97) | 6 (86) | 0.3 | 0.01−4.4 | 0.3 | |||
| Cough, n (%) | 16 (52) | 5 (71) | 2.3 | 0.4−13 | 0.4 | |||
| Dyspnea, n (%) | 30 (97) | 6 (86) | 0.3 | 0.01−4.4 | 0.4 | |||
| Fever + cough, n (%) | 14 (45) | 4 (57) | 1.6 | 0.4−7.2 | 0.7 | |||
| Fever + dyspnea, n (%) | 30 (97) | 6 (86) | 0.3 | 0.01−4.4 | 0.4 | |||
| Cough + dyspnea, n (%) | 12 (39) | 3 (43) | 1.2 | 0.3−5.1 | 0.9 | |||
| Fever + cough + dyspnea (%) | 12 (39) | 3 (43) | 1.2 | 0.3−5.1 | 0.9 | |||
| Physiological parameters on RICU admission | ||||||||
| Dyspnea, BORG scale score (IQR) | 5 (2−8) | 8 (6−10) | 2.7 | 1.6−18 | 0.01 | |||
| Kelly, score (IQR) | 1 (1−2) | 1 (1−2) | 0.9 | 0.01−24 | 0.9 | |||
| Body T, °C (IQR) | 37.5 (36–39.3) | 37 (35.7–39.6) | 1.2 | 0.2−19 | 0.8 | |||
| RR, bpm (IQR) | 34 (20−45) | 32 (18−40) | 0.7 | 0.3−11 | 0.6 | |||
| HR, bpm (IQR) | 93 (50−136) | 100 (60−140) | 1.3 | 0.1−14 | 0.7 | |||
| MAP, mmHg (IQR) | 90 (77−90) | 93 (81−103) | 1.1 | 0.01−10 | 0.9 | |||
| pH, value (IQR) | 7.48 (7.34–7.58) | 7.45 (7.31–7.51) | 0.8 | 0.4−7.9 | 0.6 | |||
| PaCO2, mmHg (IQR) | 31 (19–58) | 34 (20–62) | 1.3 | 0.4−11 | 0.5 | |||
| PaO2/FIO2, mmHg (IQR) | 138 (75–210) | 150 (84–226) | 1.2 | 0.3−7.5 | 0.4 | |||
| HCO3−, mmol/L (IQR) | 18.9 (18.7−26) | 21.2 (19.5−27.6) | 1.3 | 0.2−9.8 | 0.7 | |||
| Lactate, mmol/L (IQR) | 1.6 (1−1.8) | 2.1 (0.7−2.2) | 1.5 | 0.4−14 | 0.4 | |||
| Non-invasive support | ||||||||
| HFNC, n (%) | 22 (71) | 1 (14) | 0.1 | 0.01−0.6 | 0.01 | 0.3 | 0.04−0.6 | 0.02 |
| CPAP, n (%) | 7 (23) | 2 (29) | 1.4 | 0.2−7.2 | 0.9 | |||
| NIV, n (%) | 2 (6) | 4 (57) | 19 | 2.6−117 | 0.01 | 4.5 | 1.5−41 | 0.03 |
| Pharmacological treatment | ||||||||
| Systemic steroids, n (%) | 19 (61) | 6 (86) | 3.8 | 0.5−47 | 0.4 | |||
| Hydroxychloroquine, n (%) | 23 (74) | 6 (86) | 2.1 | 0.2−27 | 0.9 | |||
| Azithromycin, n (%) | 22 (62) | 6 (86) | 2.5 | 0.3−31 | 0.6 | |||
| Heparin (Prophylactic dose), n (%) | 18 (58) | 4 (57) | 0.9 | 0.2−4.3 | 0.9 | |||
| Heparin (Treatment dose), n (%) | 10 (32) | 3 (43) | 1.5 | 0.3−6.8 | 0.7 | |||
| Lopinavir/ritonavir, n (%) | 7 (23) | 2 (29) | 1.4 | 0.2−7.2 | 0.9 | |||
| Darunavir/cobicistat, n (%) | 4 (24) | 1 (16) | 1.1 | 0.1−10 | 0.9 | |||
| Tocilizumab, n (%) | 10 (32) | 2 (29) | 0.8 | 0.5 | 0.9 | |||
| CT Radiographic features* | ||||||||
| Lobes involved | ||||||||
| 1 | 0 (0) | 0 (0) | --- | --- | --- | |||
| 2 | 0 (0) | 0 (0) | --- | --- | --- | |||
| 3 | 5 (21) | 1 (17) | 0.8 | 0.1−6.5 | 0.9 | |||
| 4 | 10 (42) | 2 (33) | 0.7 | 0.1−3.8 | 0.9 | |||
| 5 | 9 (38) | 3 (50) | 1.7 | 0.3−8.2 | 0.7 | |||
| Bilateral involvement | 24 (100) | 6 (100) | --- | --- | --- | |||
| Distribution | ||||||||
| Diffuse | 4 (17) | 4 (67) | 10 | 1.5−60 | 0.03 | 8 | 1.3−45 | 0.04 |
| Peripheral | 2 (10) | 1 (17) | 1.8 | 0.1−18 | 0.9 | |||
| Patchy | 18 (75) | 1 (17) | 0.1 | 0.1−0.53 | 0.02 | 0.3 | 0.1−0.6 | 0.02 |
| Pattern | ||||||||
| Mainly interstitial | 6 (25) | 4 (67) | 6 | 0.99−35 | 0.1 | |||
| Mainly consolidative | 18 (75) | 2 (33) | 0.2 | 0.03-1 | 0.1 | |||
| Pulmonary embolism | 11 (46) | 4 (67) | 2.4 | 0.4−14 | 0.7 | |||
| Laboratory tests | ||||||||
| White cells count, n*109/L (IQR) | 7.2 (4.6–24.9) | 5.3 (2.1–20.1) | 0.6 | 0.2−6.5 | 0.3 | |||
| Hemoglobin, g/L (IQR) | 12 (7.3–14.4) | 13.4 (8.3–15.4) | 1.4 | 0.3−10 | 0.6 | |||
| Lymphocytes, 109/L (IQR) | 1.5 (0.1–20.0) | 0.9 (0.1–5.0) | 0.7 | 0.1−12 | 0.8 | |||
| Platelets, 109/L (IQR) | 175 (130–318) | 154 (116–270) | 0.5 | 0.1−7.2 | 0.7 | |||
| C-Reactive Protein, mg/dL (IQR) | 4 (0.1–26) | 6.7 (1.1–36.4) | 2.5 | 0.8−22 | 0.1 | |||
| D-Dimer, µg/L (IQR) | 3.4 (0.28–9) | 4.9 (0.56–12.1) | 2.1 | 0.6−18 | 0.3 | |||
| Albumin, g/L (IQR) | 35 (23–56) | 29 (23–56) | 0.7 | 0.3−9.4 | 0.5 | |||
| LDH, U/L (IQR) | 312 (179–982) | 400 (210–1065) | 1.4 | 0.5−5.4 | 0.6 | |||
| BUN, mg/dl (IQR) | 35 (24–72.0) | 27 (23–60) | 0.6 | 0.1−11 | 0.8 | |||
| Creatinine, mg/dl (IQR) | 0.89 (0.27–2.2) | 1.2 (0.47–4.7) | 1 | 1.3−7.6 | 0.6 |
Data are presented as number and percentage for dichotomous values or median and interquartile range (IQR) for continuous values.
Abbreviations: IQR = inter quartile range; COPD = chronic obstructive pulmonary disease; ILD = interstitial lung disease; RR = respiratory rate; HR = heart rate; MAP = mean arterial pressure, ARDS = acute respiratory distress syndrome; APACHE II = acute physiology and chronic health evaluation II score; SAPS II = simplified acute physiology score; SOFA = subsequent organ failure assessment score, HFNC = high flow nasal cannula; CPAP = continuous positive airways pressure; NIV = non-invasive mechanical ventilation; LDH = lactic dehydrogenase; BUN = blood urea nitrogen.
Interestingly, the daily time course of average PaO2/FIO2 ratio before and after proning was considerably different in PP patients intubated compared with those who were not (see Fig. S4).
DiscussionIn this retrospective, multicenter observational study, we investigated the effects of early awake proning in COVID-19 patients admitted to RICUs for noninvasive respiratory support, compared with standard management (SC).
The main study findings were: (1) PP prevents the need for intubation when compared to SC alone, even after adjustment for baseline confounders, (2) the reduction of ETI is particularly significant in subgroup undergoing HFNC compared with NIV or CPAP, and (3) the duration of positioning as well as the associated radiographic features consistently affect the efficacy of PP.
PP is a validated strategy in the treatment of ARDS patients, being recommended for more than 12 h/day in severe patients.9,33 Several mechanisms might contribute to the benefit of PP including the lung recruitment of previously dependent regions from relief of compressive weight, the distribution of transpulmonary pressure (PTP), the better ventilation–perfusion (V/Q) matching and the amelioration of right ventricular function.10
Given its beneficial effects, some researches hypothesized the use of PP also in patients with hypoxemic acute respiratory failure who are breathing spontaneously.13,14 Although, there is a strong physiological rationale for proning also in non-intubated patients, to date, there is still a paucity of high-quality evidence in this area.
Aside from case series and case reports, results from preliminary prospective studies in non-intubated COVID-19 patients have mostly demonstrated short-term physiological effects in terms of oxygenation improvement or a decrease in respiratory rate and/or dyspnea when awake PP is associated to NRS.16–20 In a prospective study on 56 patients with SARS-CoV2 pneumonia treated with supplemental oxygen or NIV, Coppo et al.21 showed that a trial of at least 3 h of awake PP was effective in improving PaO2/FIO2 ratio. Interestingly the increase in blood oxygenation was maintained after resupination in half of patients. Authors suggested that patients are more likely to respond to PP if procedure is performed early after hospital admission and in subjects with increased inflammatory biomarkers. No effect on clinical outcomes (i.e endotracheal intubation or mortality) was found.21
Given that patient assignment to PP treatment did not depend on the response to a preliminary prone position test, it is arguable that the PP group consisted of both responders and non-responders according to the definition of Coppo et al.21 This might explain why patients whose average PaO2/FIO2 ratio benefited the most from PP had significant difference in the rate of intubation as compared to those who did not show any consistent improvement after proning. Moreover, intubated patients maintained prone position for less time/day compared to PP patients who did not undergo ETI (3 h vs 6 h respectively) whereas comparable values of baseline PCR and D-dimer suggest a similar disease severity and/or progression. It is worth noticing that, although not significant, systemic steroid usage was associated with unfavorable outcome in PP patients. Since evidence on the beneficial effect of steroids in patients with COVID-19 ARF has been emerging,32 our results may sound contradictory. However, our data refer to a period (April–June 2020) when evidence was lacking and the use of steroids was left to physician judgment in terms of molecule, dosage, time to start treatment and duration, thus generating heterogenous schedules. Moreover, the limited number of patients and the unpowered analysis does not allow us to consider these results as significant.
After stratification according to NRS, the synergistic use of awake-PP and HFNC gave greater significant benefit to ETI reduction. These results are in contrast to a previous study22 that demonstrated that the use of awake-PP did not reduce the intubation rate in 199 patients with COVID-19 ARF treated with HFNC and was associated with a delay in intubation. However, the 28-day mortality was not affected. Because homogenous lung aeration with PP30 could result in reduced respiratory effort and lead to a lower incidence of intubation, we can speculate that a higher proportion of potentially recruitable lung takes place in early phases of ARDS compared with later phases. Interestingly, patients with NIV support did not experience significant benefit from PP. Maybe patients undergoing NIV were likely those with higher respiratory distress, thus presumably expressing a more extended and inhomogeneous lung involvement (i.e. advanced stages of ARDS). We can further suppose that NIV may reduce compliance to prone position maintenance over time. Conversely, in patients with lower level of distress who benefited from HFNC, prone position might result in a more homogeneous transpulmonary pressure distribution during spontaneous breathing, thus resulting in a less harmful lung stretch. Nonetheless, this speculation remains to be clarified to future studies.
We also found that patchy pattern on chest CT scan was independently associated with NRS failure. Endothelial injury is emerging as a central hallmark of COVID-19 pathogenesis. It has been demonstrated that the lungs of patients with COVID-19 display distinctive vascular features, consisting of severe endothelial injury associated with intracellular SARS-CoV-2 virus, widespread vascular thrombosis with microangiopathy and occlusion of alveolar capillaries as well as significant new vessel growth (Pulmonary Vascular Endothelitis, Thrombosis, and Angiogenesis in Covid-19). All these findings can contribute to further deterioration in V/Q mismatch and lung tissue damage. Finally, in agreement with previously published studies,16–22 we found that awake proning was safe, and no adverse events occurred in PP group.
This study has some limitations which need to be disclosed. First, the retrospective nature impairs the generalizability of our results. Second, the different standard operating procedures across the two centers can affect patient outcomes, such as mortality, number of days free from NRS or ICU stay. Patients were encouraged to maintain prone positioning for at least 3-h in both centers, however number of daily PP sessions was based on the physician’s judgment and/or the patient’s preference. At the same time, the decision as to whether proceed to ETI was taken by the attending staff, according to shared and well-defined ETI criteria. Notwithstanding, the presence of a control group and the identification of 4 key confounders (age, PaO2/FIO2 ratio, pH value and respiratory rate), used for analysis adjustment, could considerably mitigate these biases.
In conclusion, the description of our cohort provides further evidence that early proning in awake and spontaneously breathing Covid-19 patients is feasible and associated with a reduction of intubation rate, especially in those patients undergoing HFNC.
These intriguing results warrant further randomized controlled trials to answer all the pending questions about the real efficacy of PP in this setting.
Conflicts of interestThe authors have no conflicts of interest to declare.