Lung injury associated with drowning is mainly caused by the aspiration of water, which promotes a disruption of the alveolar-capillary endothelium and surfactant integrity, leading to an acute respiratory distress (ARDS)-like syndrome.1 Although drowning is a common cause of death,2 there is still a lack of evidence regarding the management of drowned patients. Current treatment guidelines are retrieved and adapted from other acute hypoxemic respiratory failure (AHRF) conditions. This may be due because drowning is neither a common cause of Emergency Department (ED) access nor Intensive Care Unit (ICU) admission.3 Noninvasive ventilation (NIV) and High Flow Nasal Oxygen (HFNO) therapy4 might be beneficial in these circumstances, potentially reducing the need for intubation in drowning related AHRF.
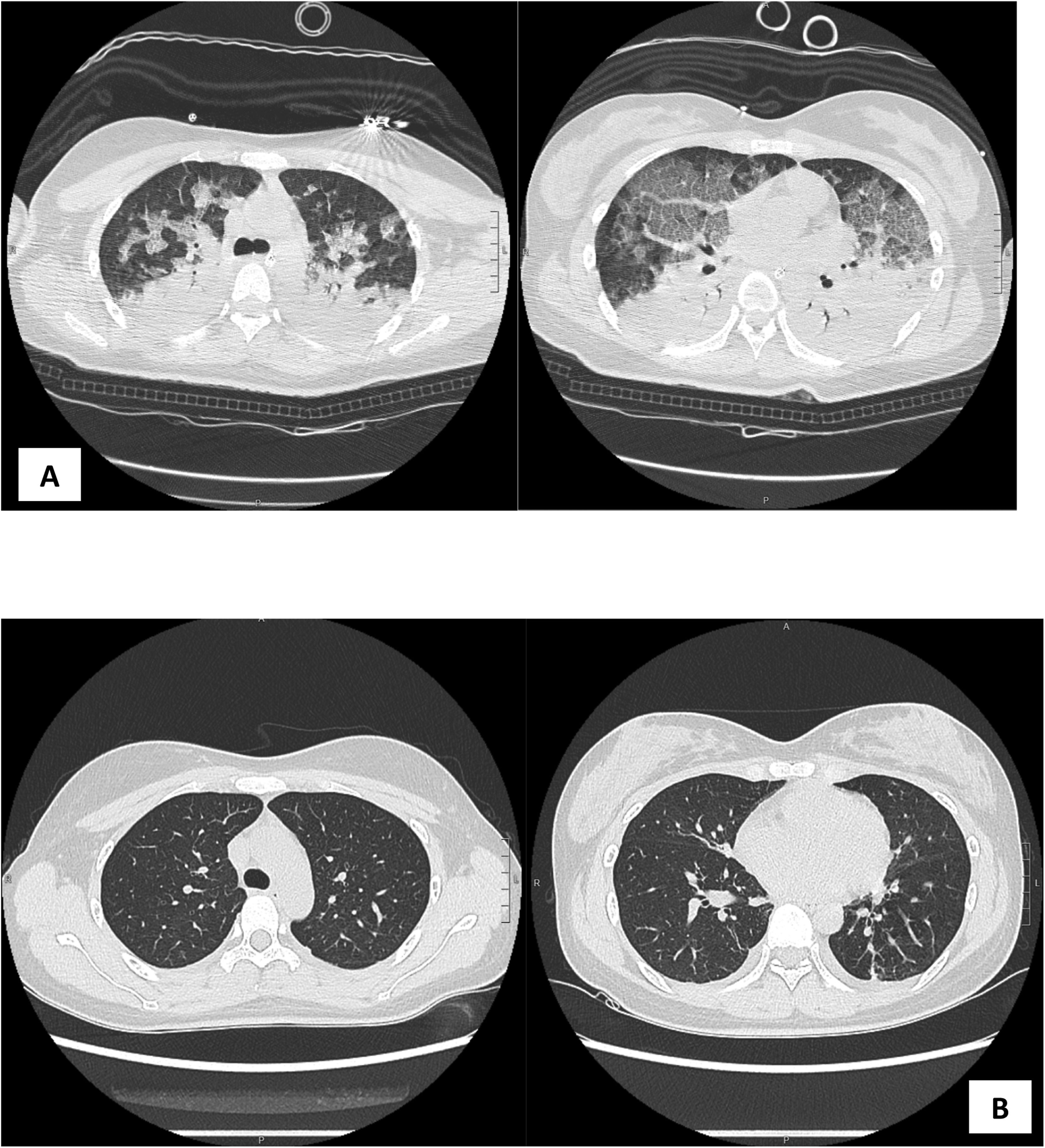
We report a case of a 29-year-old woman admitted to the Emergency Department of “Fondazione Istituto G. Giglio” Hospital of Cefalù, Palermo (Italy) after having experienced a severe AHRF following a near-fatal salt-water drowning. Written informed consent was obtained from the patient before clinical data publication. The patient was found unconscious during a snorkeling session, with her face lying submersed in water. A Grade 5 of the drowning severity classification was assigned to the patient, and basic life support was immediately initiated.5 On arrival, the patient was unconscious (Glasgow Coma Scale- GCS 11, Eye 2-Verbal 4-Motor 5), with a respiratory rate (RR) of 40 breaths/min, a heart rate (HR) of 130 beats/min, and a noninvasive blood pressure (NIBP) of 80/45 mmHg. The patient was mild hypothermic (33 °C), with a BMI of 17.7 kg/m2 (height 168 cm, weight 50 kg).1 Prompt oxygen therapy was administered via a non-rebreathing face-mask with O2 15 L/min achieving a transcutaneous pulse oximetry (SpO2) of 88%. Arterial blood gas analysis revealed a severe acidosis and hypoxemia (pH 7.14; pCO2 35; pO2 39.8; PaO2/FiO2 39.8; lac 10.2 mmol/L; BE −16.7; HCO3− 12.3 mmol/L; SaO2 60%). After an unsuccesfull NIV attempt,6,7 rapid sequence intubation was performed and a protective lung ventilation strategy at FiO2 1 was started, with a slight improvement of gas exchanges and respiratory mechanics (Plateau Pressure – Pplat 21 cmH20; compliance 30 cmH2O). Chest CT-scan revealed a bilateral pleural effusion, with bilateral consolidation areas and ground-glass opacities, mainly affecting the posterior segments of the right lung (Fig. 1A). No abnormalities were detected on the head and abdominal CT-scan. An arterial catheter was positioned in the right arterial artery to measure invasive arterial pressure. Given the hemodynamic impairment non responding to crystalloids infusion, norepinephrine was commenced (mean invasive arterial pressure - MAP target 70 mmHg), and she was then admitted to the Intensive Care Unit (ICU). A fiberoptic bronchoscopy was performed, with no signs of airway injury nor foreign materials (e.g., sand or gravel). Microbiological samples were taken before starting a course of empiric antibiotic therapy3,8 using piperacillin/tazobactam. Serum blood analysis revealed a mild elevation of CRP with normal leucocytes. Restoration of normal body temperature was gradually achieved with heating systems and blankets.
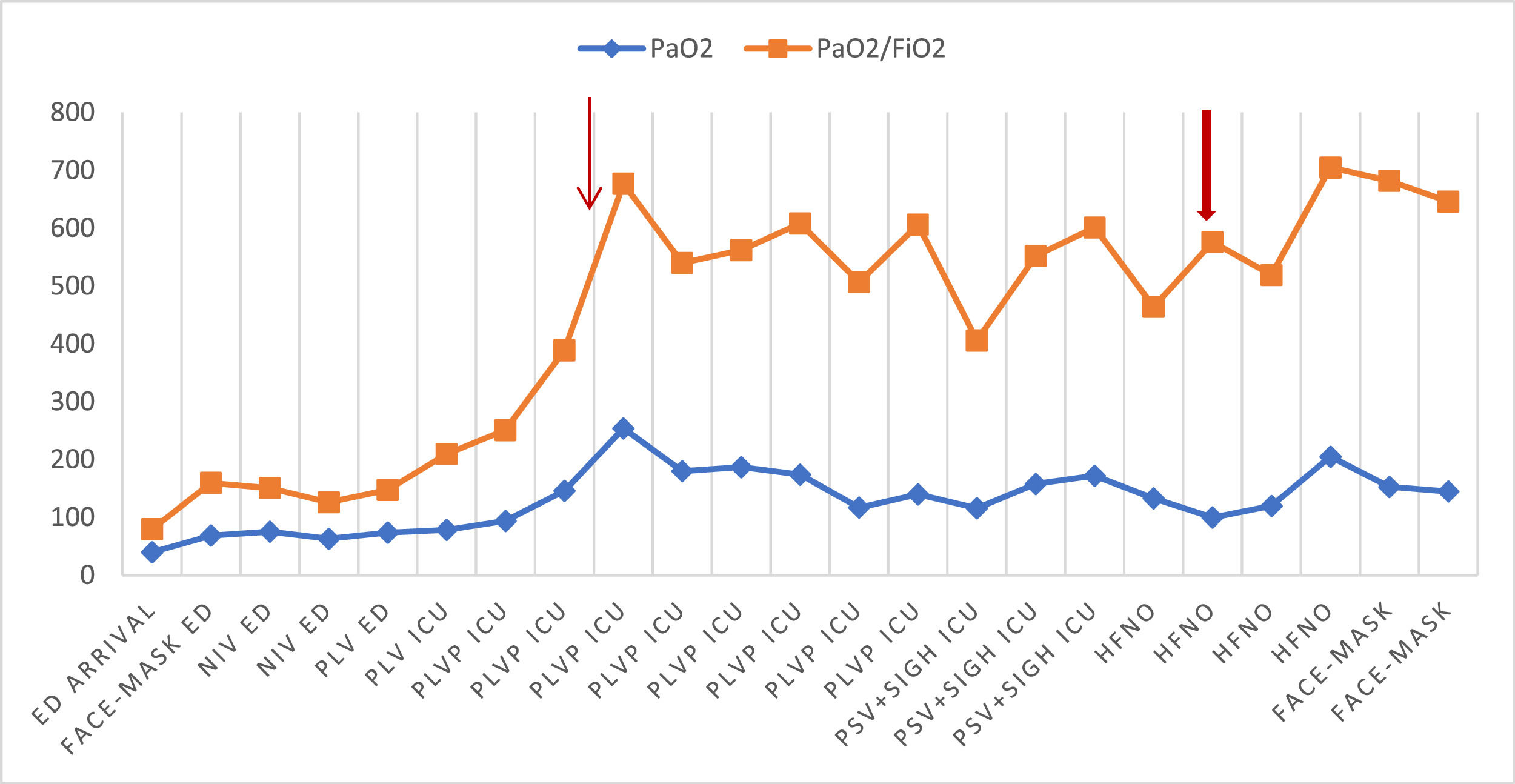
In light of the severe respiratory compromise, prone position was immediately started after 30 min from first assessment and continued for 12 h. Blood gasses revealed gradual improvements, with a complete reduction of hypoxemia at the time of supination (Plateau Pressure – Pplat 19 cmH20; compliance 45 cmH2O). Therefore, she continued a supine pressure support ventilation strategy with a sigh for other 12 h. Changes in blood gas analysis over time are shown in Fig. 2. Echocardiography follow-up was unremarkable, and vasopressors were discontinued due to the hemodynamic stability. At 36 h after admission, lung-ultrasound revealed a reduction of the consolidation pattern, and a chest CT-scan confirmed the significant improvements obtained (Fig. 1B). For this reason, she was early weaned off (PS 14 cmH2O, PEEP 8 cmH2O, FiO2 0.4) from mechanical ventilation, and extubation was planned. After extubation, she commenced HFNO (Airvo 2® Fisher and Paykel; 60 L/min, FiO2 0.3, temperature 37 °C) to prevent the possibility of atelectasis in the dependent lung regions, alternating supine and awake prone position. The aim was to achieve prone position at least for 2 h twice daily8,9 and for most of the night. The HFNO protocol was applied for two days following extubation, with a 12-hour ROX index excluding high risk of intubation (ROX index > 5.99).10 No sedation was needed, as the patient was compliant with the therapeutic plan used.
Time course of blood oxygenation changes according to the ventilation strategy applied.
ED: emergency department; ICU: Intensive Care Unit; NIV: noninvasive ventilation; PLV: protective lung ventilation; PLVP: protective lung ventilation and prone position.
*Arrows indicate gas exchanges improvements (narrow arrow: improvements related to prone position and protective lung ventilation; thick arrow: stabilization of blood oxygenation with the use of awake-prone-HFNO therapy after extubation).
During her stay, she underwent neurological and cardiological examinations, which did not reveal abnormalities that could have explained loss of consciousness and the subsequent drowning. No superinfections were detected, and oxygen therapy was interrupted before home discharge.
To the best of our knowledge, this is the first reported case of drowning where protective lung ventilation, early prone position and extubation followed by awake prone HFNO therapy has been successfully applied.11,12
It could be argued that early ventilatory weaning and extubation may cause the return of pulmonary edema, with the need for reintubation and an anticipation of prolonged hospital stays and further morbidity.5 However, in a retrospective study, the use of HFNO in drowning-related AHRF11 as first line therapy avoided intubation in 78.9% of the patients without complications.
In our case, early weaning from invasive mechanical ventilation coupled with HFNO and awake prone position was beneficial in terms of arterial blood gasses improvement, avoiding reintubation.
High-flow oxygen therapy through nasal cannula delivers heated and humidified oxygen at high flow rates. These generate low levels of positive pressure in the upper airways, and decrease physiological dead space, thus potentially explaining the observed decrease in the patient's respiratory effort. Along with a reduction of respiratory effort and generation of a moderate positive pressure, prone position increases lung aeration from ventral to dorsal regions, thus improving the ventilation-perfusion mismatch.12,13
Noninvasive ventilation as first line therapy was also found to reverse drowning-related hypoxia in a retrospective study 6. The authors concluded that the decision to use NIV has to be mainly based on the preserved or improved neurological patient's status. In our case, the NIV attempt failed despite the patient's neurological condition.
In conclusion, the lack of comparative studies and of multicenter trials still makes the treatment of the lung injured drowned patient a challenge for intensivists. Although the outcome of drowned patients is related to the potential neurological sequalae, AHRF remains the main concern. Ventilation guidelines for drowning patients are mainly adapted from AHRF patients and may not reflect the needs of this particular population. Our result confirms that early pronation, in cases of lack of improvement of oxygenation, might be the correct strategy.14 In addition, HFNO and awake prone position might have a role in avoiding reintubation while maintaining adequate pulmonary gas exchanges.
AuthorshipGM conceived the content, retrieved data and wrote the manuscript. PP revised the manuscript and gave important intellectual contribution. DB, MI and GI revised the manuscript. CG conceived the content, revised the manuscript and gave important intellectual contribution. All authors approved the final version of the work before submission.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical considerationsThe manuscript is in line with the Recommendations for the Conduct, Reporting, Editing and Publication of Scholarly Work in Medical Journals. Informed consent was obtained before data extraction and analysis from clinical records. Written consent is retained by the authors. All personal details of the patient have been removed from the manuscript, including illustrations and tables.
None.