Convex-probe endobronchial ultrasound-transbronchial needle aspiration (EBUS-TBNA) and esophageal ultrasound with ultrasound bronchoscope (EUS-B) are nowadays the interventional pulmonology cornerstone of non-small-cell lung cancer mediastinal and hilar staging; these techniques also allow the diagnosis of mediastinal and hilar involvement related to extrapulmonary primary neoplasms, infections and inflammatory diseases.
Mediastinal and hilar lymph node stations beyond major mediastinal blood vessels, without direct contact with the tracheobronchial tree, are not routinely accessed through EBUS-TBNA or EUS-B, especially due to procedural safety concerns.1 However, since 2007, there have been several case reports and series presenting endoscopic transvascular needle aspiration (TVNA) as a feasible and safe technique.2–4
To the best of our knowledge, we are reporting the first Portuguese case of a technically successful hilar lymph node sampling through EBUS-TVNA, resulting in a definitive cytological diagnosis.
A 76-year-old man, former smoker (45 pack-years), retired from metallurgical industry, with a previous medical history of arterial hypertension, atrial fibrillation under anticoagulant therapy and dyslipidemia, experienced onset of neck pain, hoarseness and progressive exertional dyspnea. The patient presented an Eastern Cooperative Oncology Group Performance Status (ECOG PS) grade equal to 1. Constitutional symptoms, anorexia or dysphagia were absent. Neck and chest CT scan revealed a 2 cm-sized nodular lesion in the right lateral wall of the hypopharynx and unsuspicious mediastinal and hilar lymph nodes. A pharyngeal biopsy was diagnostic for invasive squamous cell carcinoma of the hypopharynx (T2N2aM0, stage IV-A). Chemotherapy and radiation therapy led to favorable clinical and imaging responses.
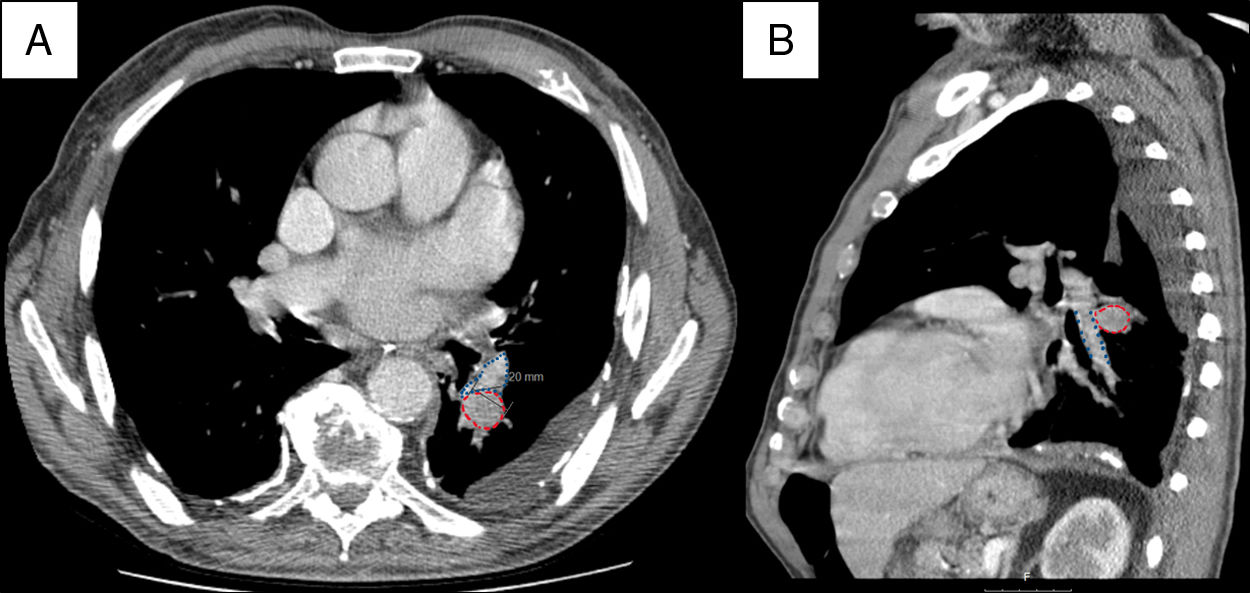
Fourteen months after the initial diagnosis, a follow-up chest CT scan identified ‘de novo’ small left pleural effusion and a 2 cm-sized left hilar lymph node suspicious for metastasis (Fig. 1). There was a multidisciplinary consensus decision to perform diagnostic bronchoscopy and EBUS-TBNA.
Contrast-enhanced chest CT scan images (A: axial image; B:sagittal image) showing the anatomical relationships between the interlobar branch of the left pulmonary artery (outlined by blue dots), the 11 L lymph node station (outlined by red dashed lines) and the left lower lobe bronchus. Note that, in this patient, the 11 L lymph node station does not have direct contact with the bronchial wall.
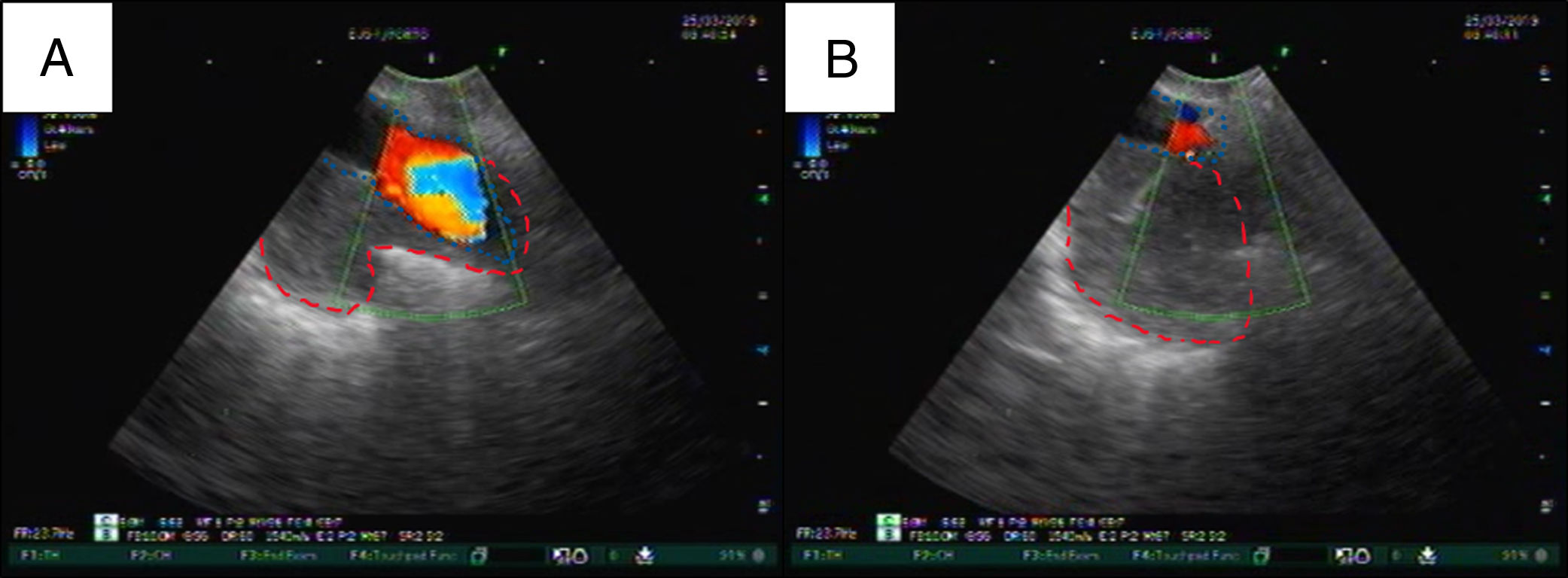
In our center, we perform EBUS under general anesthesia. Anticoagulant therapy has been properly preemptively discontinued. Fiberoptic bronchoscopy performed before EBUS was normal. A systematic inspection of mediastinal and hilar lymph node stations was performed through EBUS according to the European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS).5 The left interlobar (11 L) lymph node station was the only one warranting sampling due to suspicious imaging criteria; however, color Doppler ultrasound showed the need for TVNA to reach the lymph node station (Fig. 2). We used a 22-gauge EBUS needle to perform a transvascular puncture of the 11 L lymph node station. A good quality sample was obtained after one pass; thus, no further needle passes were done. Rapid on-site cytological evaluation (ROSE) was not performed due to the unavailability of this technique in our institution. No postprocedural complications occurred, allowing the patient to be discharged home after a short period of clinical surveillance.
EBUS-TBNA color Doppler ultrasound images of the transvascular puncture of the 11 L lymph node station: the left pulmonary artery branch is outlined by blue dots and the 11 L lymph node station is roughly outlined by red dashed lines. A: the lymph node does not have any direct contact with the bronchial wall due to the interposition of the left pulmonary artery branch. B: the EBUS needle traversed the vessel and successfully reached the lymph node.
Cytological analysis of the sampled lymph node station was diagnostic for mediastinal metastasis of squamous cell carcinoma. No immunohistochemical or mutational analysis was performed because at the time, in our institution, these techniques were available only for histological specimens. Second-line therapy with immunotherapy was started and the patient remains under treatment and follow-up.
Currently, EBUS-TVNA is not included in mediastinal or hilar assessment as it should not be performed routinely until prospective data becomes available. Additionally, it should be only executed by experienced bronchoscopists in carefully selected patients and procedural settings.
Declarations of interestNone
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.