Endoscopic techniques can be considered reasonably safe since they are widely used and the rate of complications is extremely low. Still complications do occur and in order to avoid them, the evaluation of the patient before and after any intervention is of the utmost importance. In this article, issues concerning the preparation of the patient and informed consent, the general assessment – medical history, current medications, physical examination, laboratory tests, radiological evaluation and analysis of the indication and planning will be addressed. The post intervention evaluation will also be discussed, in order to detect and treat complications and decide on the final guidance for the patient after discharge.
There are very few up-to-date studies or publications dealing with these areas, the evidence level remains low and most recommendations are based on common sense and expert opinion.
As técnicas endoscópicas podem ser consideradas razoavelmente seguras dado que são amplamente utilizadas e o índice de complicações é extremamente reduzido. Ainda assim, ocorrem complicações e, para as evitar, a avaliação do paciente antes e depois de qualquer intervenção, é da maior importância. Neste artigo, serão abordadas as questões relacionadas com a preparação do paciente e o consentimento esclarecido, a avaliação geral – historial médico, medicação actual, exame físico, testes de laboratório, avaliação radiológica e análise da indicação e planeamento. A avaliação após a intervenção também será discutida, para detectar e tratar complicações e determinar a orientação final para o paciente, após a alta.
Existem muito poucos estudos ou publicações actualizados que abordem estas áreas, o nível de evidência permanece baixo e a maioria das recomendações baseiam-se no bom senso e na opinião de peritos.
Endoscopic techniques, flexible, rigid bronchoscopy and thoracoscopy are central tools in the evaluation and treatment of respiratory disorders and their use has been steadily growing.The first rigid bronchoscopy was performed in 1897 when Gustav Killian removed a piece of pork bone from the bronchus of a 63-year-old farmer, thus avoiding a tracheotomy.1,2 IKEDA3 in the late 60s pioneered fiberoptic bronchoscopy as a tool to enter subsegmental bronchi and obtain specimens for early diagnosis of lung cancer. During the last 30 years the flexible bronchoscope has become the diagnostic instrument of choice for visualization of the bronchial tree as it is less invasive, does not require general anaesthesia and provides much better visualization of the smaller peripheral airways. The introduction of laser technology into the tracheobronchial tree and the advent of airway stents in the early 1990s caused a resurgence of rigid bronchoscopy in the management of both benign and malignant central airway obstruction.4–6
Thoracoscopy began in 1908 with Jacobeus,7 and was extensively used in the treatment of tuberculosis, for pneumothorax induction and lyses of adhesions. When effective treatment for TB was discovered, interest in this technique disappeared. With technical improvements during the 90s, thoracoscopy regained popularity for dealing with undiagnosed pleural effusion.
These techniques can be considered safe since they are widely used and the rate of complications is extremely low.8–10 A recent retrospective analysis of 23.682 patients undergoing bronchoscopy over a period of 11 years showed a mortality rate of 0.013% with a complication rate of 0.739%.9 Mortality from medical thoracoscopy ranges between 0.09 and 0.24%.11 Despite these small numbers, complications do occur and in order to avoid them, the evaluation of the patient before and after any intervention, is of utmost importance. Considering that this issue is of major concern, it is surprising that there are very few up to date studies dealing with these areas, the evidence level remains low and most recommendations (European Respiratory Society, American Thoracic Society and national societies) are based on common sense and the very small number of evidence based publications.
The aim of this article is to address pre- and post evaluation workup of patients undergoing endoscopic techniques in order to determine the fitness of the patient and the ideal planning and strategy in order to obtain the maximum benefit with the lowest risk.
The issues discussed are the preparation of the patient and informed consent, the general assessment – medical history, current medications, physical examination, laboratory tests, radiological evaluation and analysis of the indication and planning. The post intervention evaluation will also be discussed, in order to detect and treat complications and decide on the guidance to be given to the patient after discharge.
Pre-operative assessmentPreparation and informed consentThe importance of relevant and comprehensible patient information before diagnostic and therapeutic procedures is increasingly recognized, and improves the patient's tolerance of the procedure.12–14 There are several ways of helping patients, for example, careful explanation and relaxing music, have been found to calm patients and reduce anxiety.15,16 Patients and their relatives may have questions about the procedure and later management and sufficient time should be made available for this. The clinician should be able to explain the procedure, its purpose, the associated risks and possible adverse outcomes and the patient should be able to give consent entirely voluntarily.
It is the responsibility of the doctor who performs the examination to ensure that a valid consent form has been signed. An intervention performed without consent may lead to legal proceedings.17
General assessment – history and physical examinationIt is essential to have detailed information about the patient's current and past medical history for formulating diagnostic hypothesis and planning the examination. Relevant information should be obtained about smoking history, occupational exposure, and comorbidities such as asthma, COPD, cardiovascular status (myocardial infarction, arrhythmias, unstable angina, congestive heart failure), bleeding disorders (thrombocytopenia, immunossupression, uremia, impared liver function), allergies and medications (antiagregating agents, anticoagulant therapy).
Before any procedure, it is useful to know the basal physical characteristics of the patient. Monitoring of vital signs (heart rate, respiratory rate, blood pressure and O2 saturation) is mandatory (Fig. 1). Visual assessment of the patient is required to detect signs of respiratory distress, superior vena cava syndrome, stridor, hoarseness, anatomic abnormalities of the face and neck (for example wounds, burns and fractures), and spine deformities that could preclude the performance of the examination. Lung auscultation to rule out asymmetries of breath sounds (atelectasis, pneumothorax), abnormal breath sounds (wheezing, crackles) enables the physician to understand whether they had existed previously or are a consequence of the procedure. Performance status evaluation is also needed to prevent the unnecessary performance of invasive techniques in terminally ill patients who may be best treated with comfort measures.
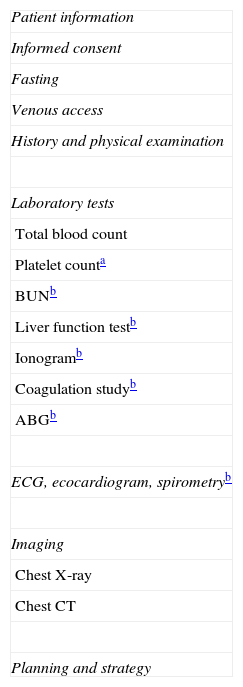
Laboratory tests and imagingTotal blood count and platelet count, to eliminate anaemia and thrombocytopenia, blood chemistry to detect electrolytic imbalances, impaired renal and liver function that may impact on blood clotting and drug metabolism (namely anaesthetics and sedatives often used during procedures) are considered routine workup. In specific situations, like elderly patients, or patients with a past history of heart disease, electrocardiogram (EEG) and echocardiogram might also be necessary. In patients with COPD and respiratory insufficiency, arterial blood gas (ABG) analyses and lung function tests might be helpful.
Imaging studies such as chest X-ray, chest CT and chest ultrasound should be carefully analyzed prior to any intervention, since they can provide valuable information for the planning of the technique.
Evaluation of the indication and planningIt is mandatory that for every invasive technique the clinician be aware of the indications, contraindications and possible complications. After following the steps addressed above regarding patient fitness for the procedure, it is crucial to go through the indication, bearing in mind that diagnostic procedures of any kind should only be performed on patients for whom a diagnosis is going to alter management and where the benefit outweighs the risks.
In addition, careful planning helps in the choice of the right diagnostic techniques – biopsy, brushings, transbronchial needle aspiration biopsy (TBNA), bronchoalveolar lavage (BAL) and transbronchial lung biopsy (TBLB) – in order to get the most out of the procedure.
In relation to therapeutic techniques, it is important to consider patient performance status and life expectancy and only perform therapies that will impact on quality of life. Also the choice of the right therapy – laser, mechanical debulking, eletrocautery, criotherapy, photodynamic therapy, stents – is crucial to ensure a successful outcome (Table 1).
Pre-procedure evaluation.
Although bronchoscopy is a safe technique with low rates of morbidity and mortality,8,9 care should be taken in certain situations.
RespiratoryPatients with severe COPD (FEV1<40% or less than 1L) should have an ABG measurement before bronchoscopy, sedation should be avoided and supplementary O2 should be given with caution.18 In the presence of a highly hypoxemic patient, bronchoscopy can be performed with noninvasive pressure ventilation via a face mask, which solves this specific problem.19 If it is not possible to ensure adequate oxygenation, bronchoscopy should not take place. Arterial oxygen tension (PaO2)>60mmHg at rest or a saturation >90%, with O2 supplements would be considered acceptable safety thresholds.20–22
Asthmatic patients are more prone to develop bronchospasm and so a bronchodilator should be given prior to bronchoscopy.8
CardiovascularIf there is a history of recent myocardial infarction, fibreoptic bronchoscopy must be postponed for at least 6 weeks,8 if possible. Unstable angina and poorly controlled congestive heart failure should also lead to postponement of an elective procedure.
Anticoagulation and antiplatelet agentsIn order to prevent bleeding complications, anticoagulant therapy should be suspended 3 days earlier or be reverted with vitamin K.8 If it is absolutely necessary to maintain hipocoagulation, heparin should be started and the INR<1.5. Regarding antiplatelet agents, a study23 concluded that clopidogrel increases risk of bleeding and should be interrupted 5 days before bronchoscopy with transbronchial biopsies. Aspirin, on the other hand, is considered to be safe.24 If transbronchial lung biopsies (TBLB) are to be performed it is essential to check platelet count, protrombine time and tromboplastin time. There is no evidence in relation to “safe” levels of coagulation parameters or platelet counts, but a platelet count of 50,000mL−1 and a prothrombin and partial thromboplastin time within 1–2s of the control value is generally regarded as safe.25
AgeElderly patients are prone to comorbidity and a decreased metabolism of some drugs, namely topic anaesthetics and midazolam. However, several studies have shown that they tolerate the procedure well and age per se is not a contraindication.26,27
Bronchoscopy in the ICUPatients in the ICU are high risk patients and benefits must outweigh the risks. Pre-oxygenation must be ensured by increasing the inspired fraction of O2 (FIO2) to 100% and the exam should be performed with a swivel connector with a perforated diaphragm, through which the bronchoscope is inserted, allowing simultaneous ventilation.28 Endotracheal tube size and external diameter of the bronchoscope have to be checked prior to the exam to avoid damage to the scope of vision and impaired ventilation.
Head trauma patients should be monitored for intracranial pressure and have complete anaesthesia with neuromuscular blockage during bronchoscopy.8
Prophylaxis of endocarditisAntibiotic prophylaxis before bronchoscopy is not recommended, unless the procedure involves incision of the respiratory mucosa.29
Pre medicationAtropine to dry the airways is no longer recommended because several studies have shown that there is no benefit compared to placebo and it has side effects like tachycardia.30 Although the routine use of sedation is not a prerequisite before bronchoscopy it should be offered whenever there is no contraindication31,32
FastingPatients undergoing bronchoscopy should have no food by mouth for 4h before procedure or clear fluids by mouth 2h before,33 patients should be allowed to take their regular medication, except for any that have to be suspended.
An intravenous access should always be provided.
Rigid bronchoscopy (RB)Rigid bronchoscopy is performed under general anaesthesia and so the first thing to do is to evaluate the state of health of the patient. Ventilatory function, cardiac status, hematologic, renal and liver function all must be assessed.
Anatomical features must be taken into consideration. Patients who cannot tolerate hyperextension of the neck or rotation of the neck due to a fused or unstable cervical spine should not be considered for bronchoscopy. Patients with unstable midline facial fractures or deformities of the mouth are not suitable to undergo rigid bronchoscopy.
Rigid bronchoscopy is the preferred option for other endobronchial therapies4,34,35 such as laser, eletrocautery, criotherapy and stent placement. As well as understanding the indications, contraindications and possible complications of RB,10 it is also essential to know about these techniques so as to be able to select the most appropriate for each particular case. Patients undergoing these therapies generally have poor performance status and relevant comorbidities, so it is crucial to analyze the risk/benefit. For a patient undergoing laser therapy it is important to know whether the symptoms are caused by the obstruction, if the lung has been collapsed for more than 4–6 weeks, if there is involvement of the pulmonary artery, if there is functional lung distal to the obstruction.
If a stent is to be placed, the following must be taken into account: type of obstruction (intrinsic/extrinsic), localization (central airways), and patency distal to the obstruction. In order to answer these questions, there should be a careful radiological and endoscopic evaluation prior to any intervention.
ThoracoscopyMedical thoracoscopy is generally performed under local anaesthesia and conscious sedation and is considered a safe procedure.11 Besides knowing the indications, contraindications and complications, a detailed medical history, drug history, physical examination and imaging, chest X-ray and chest CT, are crucial to any preoperative evaluation. Although an ultrasound prior to the procedure is not mandatory, it increases safety and should be used whenever possible.36
Patient general health status is assessed by a total blood count, blood chemistry and coagulation study. Depending on age (>65 years) and the presence of certain comorborbidities, ECG, ABG analyses and spirometry (severe COPD patients) may be added to the screening.
Dyspnea in a patient with a pleural effusion is not a concern since it will improve with effusion drainage, during thoracoscopy.
The procedure involves intravenous sedation/analgesia and so a reasonable level of oxygenation should be assured (>90% with supplemental oxygen during the procedure).36 Visual inspection of the point of entry is important in deciding where to insert the thoracoscope, avoiding skin infection or other abnormalities like sequelae of previous radiotherapy.
Patients must be able to tolerate lateral decubitus during the whole of the procedure.
Like other invasive techniques performed through surgically scrubbed skin, thoracoscopy is not likely to produce significant bacteriemia and so profilactic antibiotics are not recommended.29 When there is pleural space infection it is advisable to give profilactic antibiotics in patients at risk of endocarditis.29
If pleurodesis is a possibility, it is important to analyze the patient performance status, namely life expectancy (superior to 3 months) and to rule out a trapped lung.
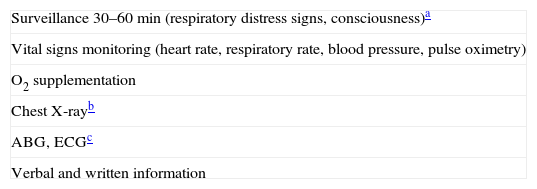
Post intervention evaluationAll patients should be observed for at least 30–60min after bronchoscopy or for 2h after rigid bronchoscopy or intervention. Observation can take place in the operating room or in a recovery room.
The monitoring of ventilation features, such as SaO2, the respiratory rate and pattern (visible signs of bronchial obstruction and respiratory distress), ABG when required and hemodynamic features, such as blood pressure, heart rate and ECG, is of paramount importance.
Post-operative care should focus on the most common complications, such as acute airway obstruction, bleeding, mucus retention, pneumothorax, respiratory failure and cardiac dysfunction. Hypoxic events subsequent to bronchoscopic procedures can occur in as many as 80% of the patients; oxygen supplementation after the procedure successfully reduces such hypoxic episodes, particularly in subjects with impaired lung function.37
Discharge from the recovery room can be performed when the patient is conscious, when all aspects of the ventilatory and airway reflexes have been restored, and when the patient is able to take deep breaths and to cough effectively without signs of obstruction.
Where patients have been sedated they must be advised after discharge not to drive or operate machinery or sign legal documents in the following 24h.8
Patients should be discharged in the presence of a relative capable of reporting complications and written information about the procedure and its complications should be provided (Table 2).
If the patient was submitted to transbronchial biopsy, a chest X-ray should be performed 1h later to rule out pneumothorax. Verbal and written information about the procedure should be provided with instructions to go to the emergency department in case of dyspnea or chest pain. Fever after BAL is a possible complication and patients should also be warned about this.
If a stent has been placed, the patient should be given a card identifying the type, the size and location of the stent and a contact phone number. A follow up visit should be scheduled; this is generally between 4 and 6 weeks but this may vary between centres. A study addressing this issue concluded that routine follow up bronchoscopies were not justified.38 Nebulizations and mucolitycs may be recommended but there are no controlled studies.
Post thoracoscopyAs medical thoracoscopy is performed with conscious sedation, monitoring of vital signs is essential until patient is fully recovered and is no longer at risk of cardiac and respiratory depression. Chest tube functioning should be checked for bleeding and air leaks. A chest X-ray should be performed to monitor lung reexpansion. Proper analgesia should be supplied especially if a talc pleurodesis has been performed. Two hours later, the chest tube should be connected to active suctioning to promote lung reexpansion. Removal of the chest tube should be considered when production of pleural fluid is less than 100–200ml/day and the lung is fully expanded.11 In mesothelioma it is common practice to perform radiotherapy within 2 weeks at the trocar site of entry to avoid seeding, but there are studies that do not agree with this.39
ConclusionA thorough evaluation performed prior to any intervention, including medical history, drug history, physical examination, blood tests and imaging, is critical to avoid unnecessary risks and to achieve a successful outcome. Diagnostic procedures must always impact on patient management and therapeutic interventions must take into account patient performance status and life expectancy. Post operatively it is important to be aware of the possible complications and provide adequate surveillance and monitoring to guarantee patient safety and make appropriate decisions for the future. It does not matter how many technological innovations and skills there are in the field of endoscopic techniques, this process of decision making before and after any intervention will remain the key point.
Conflicts of interestThe authors have no conflicts of interest to declare.