In the United States, cases of severe acute respiratory distress syndrome (ARDS), pneumonitis, lipoid pneumonia, and organizing pneumonia secondary to vaping have been rising since June 2019.1 This syndrome is termed as e-cigarettes or vaping product use-associated lung injury (EVALI) by centers of disease control (CDC).1 We report the case of a young female who was diagnosed with EVALI and required mechanical ventilation with extracorporeal membrane oxygenation (ECMO).
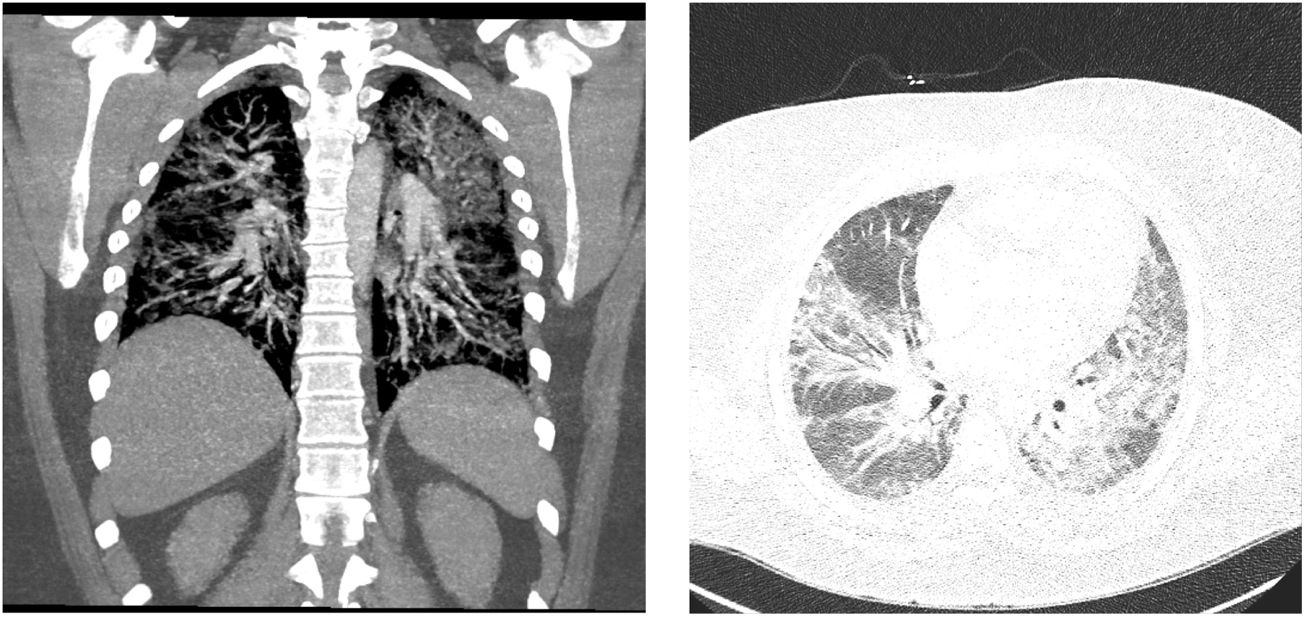
A 26-year old female with a history of asthma, depression, and substance abuse presented to the emergency department (ED) with two weeks of dyspnea on exertion and whitish productive cough. She had a history of smoking cigarettes and vaping tetrahydrocannabinol. The patient reported receiving a new tetrahydrocannabinol cartridge from a different supplier 2.5 weeks ago. Her oxygen saturation was 84% on room air with respiratory rate (RR) in the 30s and she had crackles in the lungs bilaterally. Initial labs were significant for leukocytosis (WBC: 16.7k/mm3) and EKG was normal. Chest X-ray showed bilateral opacities, and CTA chest revealed bilateral ground-glass opacities and no pulmonary embolism (Fig. 1). Echocardiography showed normal ejection fraction. Broad-spectrum antibiotics and furosemide were started. ABG on 12L of oxygen showed pH: 7.40, PCO2: 39, bicarbonate: 23.8, and PO2: 93 with a persistent RR of 30–35. She was intubated for respiratory failure. Bronchoscopy was performed, and bronchoalveolar lavage was sent for analysis and culture. High dose methylprednisolone was started after no bacterial growth was seen on initial sputum culture. While on mechanical ventilation, she continued to be hypoxic showing features of severe ARDS (PaO2/FiO2=68), following which she was placed in prone position. After 20min of pronation, she was on a ventilator setting of tidal volume: 6mL/kg, FIO2: 100%, PEEP: 15cm H2O, and driving pressure of 15cm H2O. ABG showed pH: 7.33, PCO2: 46, bicarbonate: 26, PO2: 69. After 4h of pronation, the patient was placed in a supine position. Given the severity of respiratory distress, a veno-venous ECMO (31 French ProtekDuo, flow: 4.4L/m, sweep: 2) was cannulated through the right internal jugular vein with the plan to adjust settings based on frequent ABGs. She was then placed on an ultraprotective ventilator setting (tidal volume: 250mL, PEEP: 10cm H2O, RR: 10 with FIO2: 40%).
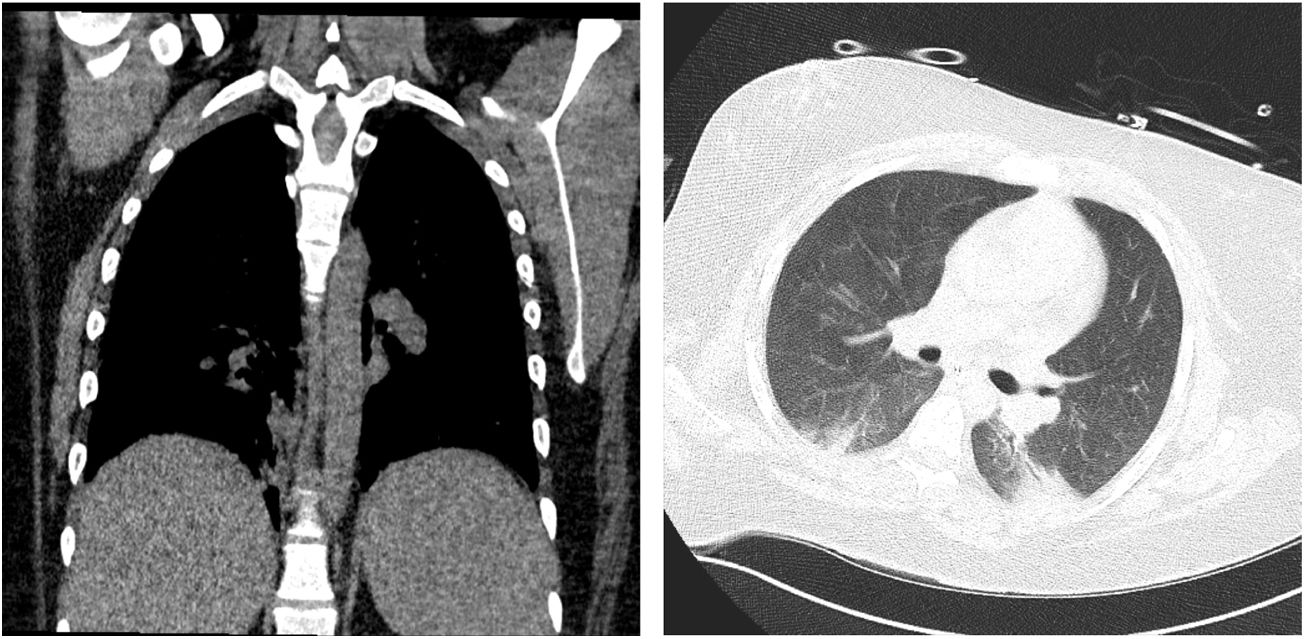
Results from cultures remained negative. Further tests were negative for fungus, influenza, atypical organisms, HIV, and other rheumatological diseases. After 3 days of methylprednisolone 500mg IV, she was switched to prednisone 60mg IV twice a day. After she showed clinical and radiological signs of improvement (Fig. 2), ECMO was weaned off on the 8th day. She was extubated on the 10th day. Subsequently, she got out of the ICU on the 15th day and was discharged on the 20th day of her hospital stay.
The management of EVALI comprises of respiratory supportive care, antibiotics, and corticosteroids. The initiation of antibiotics on presentation is important as pneumonia is a common cause of respiratory failure. Once no evidence of infection has been identified, the de-escalation of antibiotics should be considered. Corticosteroids have known to show excellent clinical results. However, caution must be applied while starting corticosteroid if there is a strong suspicion of infection. At times, if the presentation is less severe, corticosteroid could be held until infectious causes are ruled out. Although up to 35% of patients may require intubation and mechanical ventilation, the overall prognosis is usually good, and improvement is seen within weeks of starting corticosteroids.2
Three criteria define EVALI: pulmonary infiltrates in imaging, use of electronic cigarettes within the previous 90 days, and the absence of other possible infectious, cardiac, neoplastic, or rheumatological causes.2 Our patient met all three. Escalation of care with intubation and mechanical ventilation was performed because of severe ARDS. Due to the worsening hypoxia, early ECMO was initiated with a protective ventilation strategy to facilitate faster recovery of the lung injury. In a case series by Maddock et al., one out of six patients required ECMO for seven days.3 In a case report, Baxter et al. report that early initiation of ECMO for a young male helped improve the condition within 72h.4 In another case series by Choe et al., one out of four patients required ECMO for 14 days for refractory hypoxia.5
This case highlights the complicated course and the devastating effects of EVALI. In addition to expanding the scant literature, to the best of the authors’ knowledge, this is also the first case where ECMO was performed for EVALI on a female patient. Early initiation of ECMO with lung-protective ventilation strategies could be considered as a potential management strategy for selected individuals suffering from severe ARDS due to EVALI, and this case serves as a data point for such situations.
Conflicts of interestThe authors have no conflicts of interest to declare.