Hemoptysis is a common symptom in clinical practice that should be promptly investigated.1 There are several possible etiologies and, although most of the cases represent self-limited events, severity can be variable and the clinical course unpredictable.1,2 The authors report a case of an unusual cause of hemoptysis.
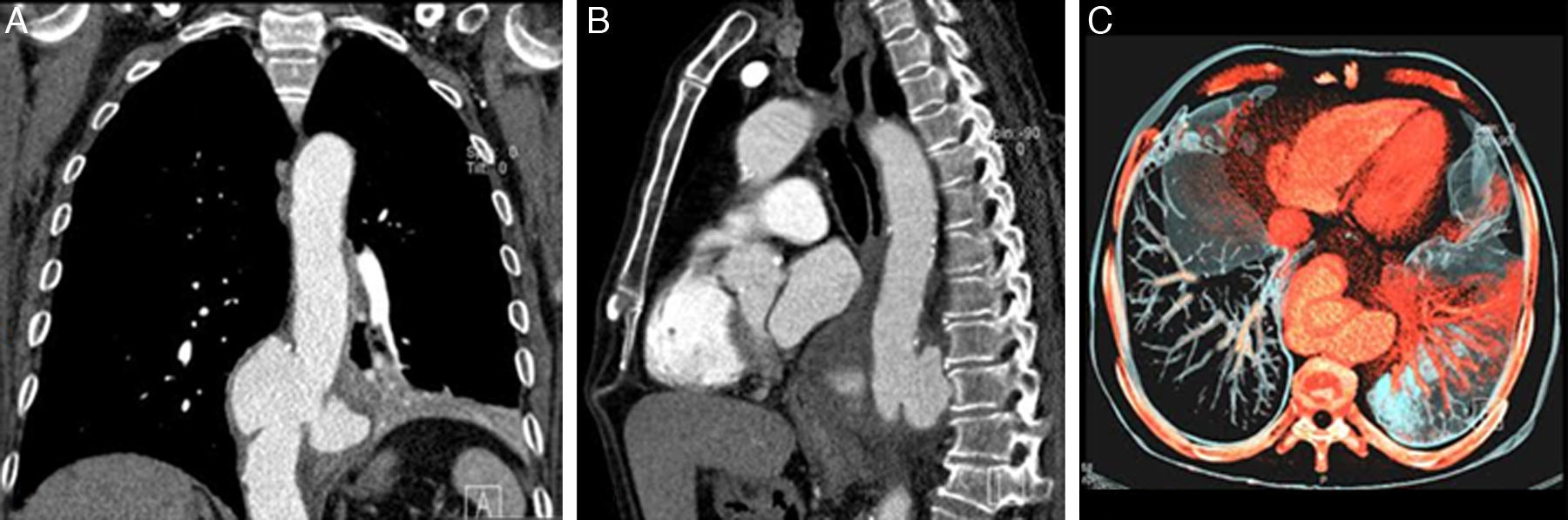
Case report63-year-old male, smoker, without previously known pathologies, except history of non-recent traumatic fracture of the 12th thoracic vertebra. The patient presented to the emergency department with massive hemoptysis and dyspnea and was stabilized through medical non-invasive measures, without needing endoscopic control for bleeding. He reported a first episode of small volume hemoptysis four days before admission and, additionally, complaints of bloody sputum since the previous month, associated with a persistent and diffuse pain in the lower third of the chest and in the upper abdominal quadrants, bilaterally, without relieving or worsening factors. On physical examination at admission, the patient was normotensive, afebrile, with pulse oximetry on room air of 87% and had decreased breath sounds in the lower third of the left hemithorax at chest auscultation. Blood gas analysis revealed type 1 respiratory failure (pO2 50.9mmHg). Analytical study presented mild leucocytosis (12.74×109/L), C-reactive protein of 16mg/L and a decrease of 2.4g/dL in hemoglobin values was documented on the second day of hospitalization. Sputum smear was negative. Chest radiograph showed a slight reticular opacity in the lower third of the left hemithorax. To characterize this finding, a computed tomography (CT) was performed, revealing the presence of a large saccular aneurysm of the transition of the thoracoabdominal aorta with signs of contained rupture and alveolar consolidation in the left lower lobe (Fig. 1). The patient underwent endovascular aneurysm repair with placement of thoracic aortic endograft. Subsequent clinical evolution was favorable, without recurrence of hemoptysis.
Coronal (A), sagittal (B) and axial (C) reconstructions of computed tomography scan of the chest showing a large saccular aneurysm (72×52×54mm of diameter, T×AP×L) of the transition of the thoracoabdominal aorta with signs of contained rupture and alveolar consolidation in the left lower lobe.
Hemoptysis might have several possible etiologies. As clinical course is unpredictable and a massive hemoptysis might be a life-threatening event, etiological investigation is mandatory, with a prompt identification of its causes being essential to initiate an adequate treatment.2 The majority of cases are associated with an infectious or inflammatory process, such as bronchiectasis, tuberculosis or chronic bronchitis, and with lung cancer.2,3 In some cases, past medical history and clinical findings, in association with imagiological aspects, help narrow the differential diagnosis.3 However, sometimes an uncommon cause with a poor radiographic expression might not be included in the diagnostic hypotheses, which would delay the correct diagnosis and the possibility of timely therapeutic intervention, in this way determining an unfavorable evolution.1 A dissecting aortic aneurysm is an uncommon cause of hemoptysis.1,3 In the present case, the clinical manifestation was not the most typical. Usually, a dissecting aortic aneurysm presents acutely, with severe chest pain and with associated hemodynamic instability.4,5 More rarely, it can present with hemoptysis that can be massive and potentially fatal, becoming a surgical emergency.4,5 In this case, the rupture was contained, which might have contributed to its subacute presentation. Imaging had a major role in this context, allowing identification of the cause of hemoptysis, and so a prompt directed therapeutic approach was performed. After endovascular aneurysm repair, the patient had no recurrence of hemoptysis.
Conflicts of interestThe authors have no conflicts of interest to declare.