During the last two decades, systems for supplying heated and humidified oxygen at high flow via nasal cannula have been developed as an alternative to standard oxygen supply systems. High-flow oxygen through nasal cannula (HFNC) devices consists of an air and oxygen mixer, connected via an active heated humidifier to a nasal cannula, allowing supply of a FIO2 of 21–100% (regardless of flow speed) with flows of up 60L/min.1
We conducted a prospective observational study at the Intermediate Care Unit (IMC) in a tertiary hospital from March 2014 to January 2015. We included patients with persistence of acute respiratory failure (defined as oxygen saturation measured by pulse oximetry or arterial blood gas less than 95%) from any etiology, despite oxygen delivered through face mask with an estimated FIO2 greater than 50%. Patients did not require endotracheal intubation – invasive mechanical ventilation or otherwise had a do-not-intubate (DNI) order. Patients with PaCO2 over 50mmHg or pH lower than 7.28 were excluded. HFNC was delivered by the Optiflow® with the MR850 humidifier (Fisher & Paykel, Auckland, New Zealand). The initial FIO2, the flow of oxygen and subsequent adjustments (including progressive withdrawal of HFNC and switching to conventional therapy) were established by the attending physician according to the patient's condition.
Clinical variables (heart rate, respiratory rate) and arterial blood gas prior to the start of HFNC and after 2h of use were recorded. The perceived sensation of dyspnea was assessed using the Borg CR10 scale (from 0 – no dyspnea – to 10 – maximum dyspnea) and the comfort of the device was evaluated using a visual analog scale (from 1 – very uncomfortable to 10 – very comfortable); both variables were collected prior to HFNC use and immediately following removal of the device. The sample had a non-normal distribution, so non-parametric tests were used for statistical analysis. Paired t test and the Wilcoxon signed rank-test were utilized for statistical comparisons.
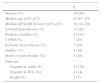
Baseline characteristics of the sample are detailed in Table 1. The main etiology of respiratory failure was heart failure (11), respiratory infection (11), asthma (3) and miscellaneous (3). HFNC was initiated at a mean FIO2 of 0.77 (range 0.5–1.0) and a flow rate of 52.4L/min (range 40–60L/min). Two subjects (7.1%) died in the IMC, one due to gastrointestinal bleeding and another due to metastatic lung cancer; 4 subjects (14.2%) required admission to the intensive care unit, 3 of them requiring mechanical intubation; 22 subjects (78.5%) were discharged from the IMC and transferred to hospital ward with conventional oxygen therapy. The mean length of stay in the IMC was 46.1h. HFNC was used continuously in all cases, with a median duration of HFNC of 24h (range 3–240h). Analysis of clinical and laboratory parameters prior and after HFNC are detailed in Table 2.
Baseline characteristics of the sample (n=28).
| n | |
|---|---|
| Women (%) | 14 (50) |
| Median age (p25–p75) | 82 (67–87) |
| Median APACHE II score (p25–p75) | 16 (14–18) |
| Arterial hypertension (%) | 12 (42) |
| Diabetes mellitus (%) | 12 (42) |
| COPD (%) | 7 (25) |
| Ischemic heart disease (%) | 7 (25) |
| Smoker (%) | 5 (18) |
| Home oxygen therapy (%) | 5 (18) |
| Outcome | |
| Transfer to ward (%) | 22 (79) |
| Transfer to ICU (%) | 4 (14) |
| Death (%) | 2 (7) |
APACHE: acute physiology and chronic health evaluation; COPD: chronic obstructive pulmonary disease; ICU: intensive care unit.
Compared clinical and laboratory parameters prior and after HFNC.
| Parameter | Prior to HFNC | After HFNC | p |
|---|---|---|---|
| Heart rate (bpm) | 90.5 | 84 | 0.01 |
| Respiratory rate (bpm) | 30 | 22 | <0.001 |
| PaCO2(mmHg) | 41.5 | 40 | 0.78 |
| PaCO2 in COPD | 47 | 46 | 0.31 |
| O2saturation (%) | 86.5 | 98 | 0.001 |
| pH | 7.43 | 7.44 | 0.47 |
| Dyspnea | 8 | 3 | <0.001 |
| Comfort | 3.5 | 8 | 0.001 |
HFNC: high flow oxygen therapy through nasal cannula; PaCO2: partial pressure of carbon dioxide; COPD: chronic obstructive pulmonary disease.
In adults, the use of HFNC has been studied in multiple situations. In patients with acute respiratory failure, a study showed a significant decrease in respiratory rate, improvement of dyspnea according to the Borg scale and increase in PaO2.2 The same group obtained similar results in patients with acute respiratory failure despite conventional oxygen therapy in an intensive care service.3 A clinical trial comparing HFNC, conventional oxygen therapy and noninvasive mechanical ventilation demonstrated a reduction in mortality at 30 days in patients treated with HFNC against other modalities, but no differences were found in terms of the need for progression to invasive ventilation.4 Being an IMC unit, where a significant proportion of patients have DNI order, the baseline characteristics of our sample substantially differ with studies mentioned above, mainly in the fact that our population is older and they present with greater severity at admission. In most of our patients, the etiology of respiratory failure were heart failure and respiratory infection, conditions that are reversible with adequate treatment, which allowed progressive withdrawal of HFNC and switching to conventional oxygen therapy in a median of 24h. Our findings support the use of respiratory therapy HFNC as an alternative to NIV in non-severe hypercapnic patients for whom tracheal intubation is not an option.
In the analysis of the subgroup of patients with a prior diagnosis of COPD, no significant changes in pH or PaCO2 levels were found. However, all the patients in our sample had pH>7.28 and PaCO2<50mmHg. Caution should be taken in severe hypercapnic patients with HFNC, since clinical evidence for the use of HFNC in patients with chronic CO2 retention is low and its use in a systematic way in these patients is not recommended; several ongoing studies are trying to assess the use of HFNC in these patients.5
Regarding the improvement in dyspnea, other studies have found similar results in terms of comfort.1,6,7 A clinical trial compared HFNC with Venturi mask, showing greater comfort, fewer desaturations and interface displacements in patients with HFNC.8
In short, HFNC improves oxygenation in patients with acute hypoxemic respiratory failure despite conventional low flow oxygen therapy, without affecting pH or PaCO2, with good results in terms of comfort and reduction of dyspnea.
Authors’ contributions- -
Pablo Demelo-Rodríguez: literature search, data collection, study design, analysis of data, manuscript preparation, review of manuscript.
- -
María Olmedo-Samperio: literature search, data collection, study design, analysis of data, manuscript preparation, review of manuscript.
- -
Daniel Germán Gaitán-Tocora: literature search, data collection, study design, analysis of data, manuscript preparation, review of manuscript.
- -
Juan Carlos Cano-Ballesteros: literature search, study design, analysis of data, manuscript preparation, review of manuscript.
- -
Jorge del Toro Cervera: literature search, study design, analysis of data, manuscript preparation, review of manuscript.
- -
Juan Antonio Andueza-Lillo: literature search, study design, analysis of data, manuscript preparation, review of manuscript.
The authors have no conflicts of interest to declare.