In the Netherlands we have an unique organisation of only 4 centres being responsible for all patients who need Home Mechanical ventilation(HMV). Nationwide criteria for referral and initiation of HMV are stated in our national guideline and recently a unique national learning management system (LMS) for all caregivers and professionals was developed. A nationwide multi-centric research program is running and every centre is participating. In this paper we provide information about the evolution of HMV in the Netherlands during the last 30 years, including details about the number of patients, different diagnose groups, residence and the type of ventilators.
Home mechanical ventilation (HMV) was first initiated in Europe in the sixties during the polio epidemic to offer the possibility of maintaining chronic ventilatory support outside the hospital. While patients with a neuromuscular disease were the first to be considered, many others with different diagnoses followed afterwards. Over the following years, it was observed by the Dutch government that the care of these patients was poorly organized; therefore, they chose to centralize HMV in 1992 and divided the Netherlands into four regions each with their own HMV center.1 In addition, it was mandated that all centers had to be associated with a University hospital (Fig. 1). As we believe that this is a very well-functioning approach, we will describe the individual elements necessary to build such a unique system with focus on the following topics: 1) organization of HMV, 2) training of caregivers and health-care professionals, 3) research, and 4) associated financial aspects. Furthermore, we will present detailed data obtained over the last 30 years from our national HMV registry, including number of patients, underlying diseases, use of invasive versus non-invasive intervention, and, most importantly, the residence of the patients.
Organization of HMV in the NetherlandsEach HMV center organizes patient care in their specific region with a team consisting of pulmonologists, specialized nurses and technicians. After the indication for HMV is determined by the pulmonologist, the specialized nurse will take over and start HMV. Currently, this still takes place in an inpatient setting but it is our goal to start HMV at home more often, as it has been shown to be safe, effective and cost-effecient.2–4 During this process, the patient, family and caregivers are instructed and trained on site. Our team is also responsible for the follow-up with HMV patients, which means that the same group of nurses will visit the patient at home at least once every year and the patient will visit the outpatient clinic for scheduled intermittent evaluations. Technical aspects of the intervention, including analysis of the ventilator files, measurements of transcutaneous carbon dioxide and oxygen saturation, and (on indication) polygraphy, are addressed at home by the nurses, who are authorized to change settings accordingly. Patients can always contact their HMV center in case of problems as the nurses are on call 24/7. The Homecare provider is only involved in periodic and ad hoc maintenance of the ventilators. All the above is incorporated into the Dutch guidelines for Home Mechanical Ventilation (2012), which were collectively developed by all HMV centers to improve the communication in the care chain. Implementation of these guidelines led to a further increasing awareness in the care chain and standardized the roles of those involved. Safety criteria were standardized not only for the hospital, but also for private homes and other care facilities. Furthermore, it set a number of standards regarding expertise, minimum number of new patients treated per year, and number of specialized nurses required per patient for regular follow-up. As we try to create a safe environment for our HMV patients, the guidelines also include, for example, a protocol applicable in case of power failure; thus, how evacuation should be efficiently executed, which is particularly important for more dependent patients.
As our common standard guidelines are not suited for children, a special Dutch edition for children was developed.5 Finally, to ensure proper communication between all parties in the field, which is crucially important for the success of a care system, the Dutch association of patients and professionals involved in chronic ventilatory support was established more than 30 years ago. It serves as a national mediator and information provider for patients, voluntary and professional caregivers, health insurance companies, and policy makers.
Education and training of caregivers and health-care professionalsIn 2019, a unique national training program for caregivers of chronically ventilated patients was launched.6 Protocols among the 4 HMV centers were unified and a blended learning experience was developed for both voluntary and professional caregivers. Whereas e-learning is used to provide the necessary knowledge, practical training will be given at our skills center and in specific patient-related situations. After completion of the training, an assessment consisting of a theoretical exam and a practical test will follow. The practical exam will contain all restricted and high-risk procedures, testing the acquired knowledge of the necessary equipment, and assess how caregivers handle acute situations. The professional caregivers will be awarded with credits for their specific accreditation register. One of the main advantages of this training approach is that all voluntary and professional caregivers working in the field of HMV are trained in the same way across the entire country. To date, we have almost reached 10.000 registered individuals who have followed this learning program.
ResearchIn line with the aforementioned forms of collaboration regarding training, efforts are being directed toward optimally benefitting from research endeavors on a national level. For example, a recent study involving patients with neuromuscular diseases, showed similar results for HMV initiation at home and in the hospital in addition to substantial savings when initiating the process at home.4 These study will impact our national guidelines regarding the place of initiation of HMV in specific patient groups. Further collaborative studies in COPD (NCT03053973), myotonic dystrophy (NL7972) patients and ALS patients (NCT05033951) are currently ongoing.
TelemonitoringWhile we got more experience in telemonitoring during initiation and supervising patients at home, this was solely in a study environment and we find now that implementing it in daily care is more difficult. The challenges we have to deal with are privacy and security issues on the one hand and getting reliable signals of both ventilators and transcutaneous monitors. Nevertheless also on this important topic the 4 HMV centers have the same goal and it is foreseen to have a uniform pathway by 2022.
Financial aspectsThe Dutch Healthcare authority dictates that HMV treatment will only be reimbursed if one of the 4 centers is involved. This means that all Dutch patients qualifying for HMV have to be referred to one of these centers. In 2017, a task force entrusted to look for alignment of disposables within the 4 different centers was assigned. The first national tender for the purchase of disposables needed for the care of HMV patients was completed, which will lead to a cost reduction. Plans are currently being conceptualized for joint procurement and maintenance of ventilators.
National registry on HMVAll patients treated over the last 30 years in any of the 4 Dutch HMV centers were included in the national registry for HMV.
Data collectionThe data are collected in every center on the 1st of January every year and sent to the registry.
These data contain information regarding gender, sex, age, diagnosis leading to HMV, types of ventilation, and type of residence.
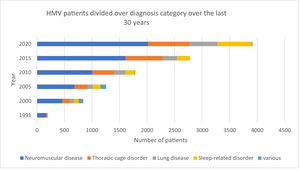
Diagnostic categoriesPatients are divided into 5 main categories: neuromuscular disease, thoracic cage disorder, lung disease, sleep-related breathing disorder, and various (not belonging to the other 4 groups). The sleep-related breathing disorder group represents those patients who need ventilatory support (i.e., pressure support) if CPAP is not effective.
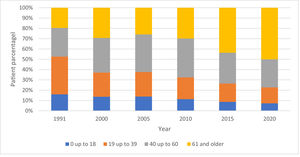
Age distributionPatients are divided in 4 age categories: 0-18, 19-40, 41-60 and >61 years of age.
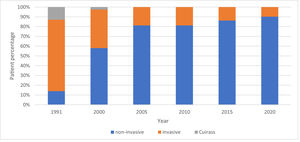
Types of HMVHMV is divided into 3 types: non-invasive ventilation (NIV), invasive ventilation (IV) and negative pressure ventilation by Cuirass (a shell around thorax and abdomen).
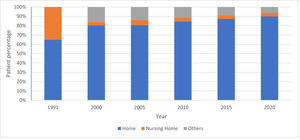
Types of residenceWe define 3 main types of residence: ‘home’, a private accommodation in which the patient or partner has full control, while care can be provided by themselves or by caregivers; ‘nursing home’, defined as institutions where patients live permanently because they need professional care facilities; ‘other’, comprising places of residence other than a nursing home where care is organized under certain individual conditions.
Fig. 2 shows the steady and marked growth of the number of patients and indicates that patients with neuromuscular disorders have consistently represented the largest group. As for all other groups, the number of HMV patients with thoracic disorders or lung disease steadily increased but remained similar relative to the total patient number. Interestingly, a modest increase in the relative number of HMV patients with sleep-related disorders appeared to be evident over the past 5 years.
When evaluating the dynamics of age distribution, we see a shift from younger patients who are in the age groups 0-18 and 19-39 years to more senior patients (>61 years of age) as being the predominant group relying on HMV. Even the middle aged group (40-60) was dominant in the first 20 years, but lost share in the last decade in favor of the senior group (Fig. 3).
While 30 years ago, patients almost exclusively were ventilated invasively, nowadays, the majority of patients undergo a non-invasive approach (Fig. 4).
Fig. 5 shows that the vast majority of HMV patients’ lives at home and that the number of patients in nursing homes decreased from roughly 37% in 1991 to 4% in 2020.
DiscussionThis paper outlines the unique organization of HMV in the Netherlands: an example of how knowledge and experience in the area of HMV can be efficiently centralized. The national registry provides a valuable source of information of trends in HMV in the Netherlands over the last 30 years. Carefully consulting this registry has led to a national guideline that defines what it entails to function as an effective HMV center. This contributed to a uniform set up and improved management of HMV as well as an updated reimbursement policy.
Building on the strong cooperation among centers, a national education program fostering uniformity in high-risk procedures in the entire country was developed. In addition, a national research program with focus on both COPD and neuromuscular diseases has been launched. Currently, we are working on updating our guidelines to further improve our unique organization, with the end-goal of optimizing the care of HMV patients. We strongly agree with a recent editorial by Schwarz and Windisch in which they embraced our organization and suggested that the Dutch system might serve as a blueprint for other countries.7
The number of HMV patients in the Netherlands has considerably increased over the past 30 years (Fig. 2). In 2001/2002, at the time of the Eurovent study, the relative HMV use on a population-level was 5.6/100.000 in the Netherlands, while the average use amounted to 6.6/100.000 in Europe (with the exclusion of patients with OSA8). In 2020, 22 out of 100,000 people rely on HMV in our country; this number excludes patients with standard CPAP. While there is no recent update available of the Eurovent study, a much higher prevalence was recently reported in the Geneva district area (37.9/100.000) and the Italian region Lombardy (63 / 100.000).910 Although it is evident that the Dutch prevalence of HMV users increased considerably over the last decade, it is still lower compared to other western countries. One of the reasons is that, due to our system, we are very restrictive in prescribing HMV. The Dutch uniform and strict guidelines used by all 4 centers ensure that only patients meeting certain criteria can start HMV. As mentioned before, patients that need HMV must be referred to one of the 4 centers; otherwise, HMV is not possible in the Netherlands. Not all patients might be motivated to travel to one of these centers leading to a lower number of patients on HMV. Another reason potentially underlying the relatively low prevalence in the Netherlands is that, in contrast to Italy and other south European countries, COPD was previously not considered an indication for HMV as we were not convinced of the (beneficial) effects of HMV treatment in COPD patients. This was highlighted and confirmed in a study by Crimi et al. (2016) showing that the Netherlands had the lowest percentage of COPD patients on HMV.11 However, this perspective changed after publications by Kohnlein and Murphy demonstrating that chronic NIV is beneficial in COPD patients with chronic hypercapnic respiratory failure.1213 Nowadays, COPD patients with chronic hypercapnia do qualify for NIV in the Netherlands, preferably in combination with pulmonary rehabilitation.
Despite the policy change of prescribing NIV to specific COPD patients, this is still the smallest group of HMV patients in the Netherlands, in contrast to the situation in Switzerland, where COPD patients constitute the predominant HMV group.9
Remarkably, patients > 60 years of age have become the largest group of HMV users in the Netherlands over the past decade (Fig. 3). A similar but even more extreme trend was observed in a Swiss study where the median age of HMV patients was 71 years and only 25% of the patient population was under the age of 59.9 The exact reason for this is unclear; however, more knowledge and a better understanding of the possible benefits of HMV in this group might drive the increased demand among more senior patients.
As indicated by several studies, chronic ventilatory support shifted from invasive towards non-invasive ventilation over the last years. At present, we only apply invasive ventilation in ∼10% of all our HMV patients in the Netherlands, which is similar to the 10.4% invasive ventilated patients reported in a 2018 Hungarian study.14 The reason for this shift is the availability of more sophisticated ventilators with a wide range of masks and the possibility of adding mouthpiece ventilation. This means that in almost all patients an effective set up of non-invasive ventilation is possible. However, probably the most important contributing factor is the increased use of assist coughing techniques like air stacking and mechanical in- and exsufflation.15 Sputum can be mobilized more effectively and there is no need to change to invasive ventilation. Finally, we are proud that 90% of the patients is still living at home probably partly due to the fact that ventilatory support is provided non-invasively. The care associated with NIV is less complex and less intense for caregivers than with invasive ventilation. Moreover, the use of ventilators in general has been simplified enormously. Another reason for the success of HMV is the blended learning program; ongoing evaluation indicates this initiative (in combinations with the nationwide protocols) is a supportive tool in daily practice for implementing home care.
In conclusion, this paper presents the unique organization of HMV in the Netherlands. The centralization of HMV care demonstrated to be effective in providing a uniform treatment to all patients with chronic respiratory failure based on a nationwide training system. Undoubtedly, continued collaborative research by the 4 HMV centers will further improve our standard of care.