Hospitalizations due to community-acquired pneumonia (CAP) in mainland Portugal from 2000 to 2009 accounted for 3.7% of all hospital admissions in population with 18 or more years of age. There is no direct-cost data regarding these admissions.
MethodsIn this observational descriptive study all adult hospitalizations associated with CAP diagnosis were retrospectively analyzed for the period between 2000 and 2009. Patients under 18 years old, those with pneumonia as secondary diagnosis, patients with tuberculous or obstructive pneumonia, and immunocompromised patients were excluded from the study. The direct cost of hospitalization was calculated according to the diagnosis-related groups (DRG), established for the respective year of hospitalization.
ResultsThere were 294,026 hospital admissions with an average annual direct cost of 80 million Euros, which almost doubled between 2000 and 2009. The average direct hospitalization costs per admission, including wards and Intensive Care Units (ICU), amounted to €2,707, with an increasing trend. The average hospitalization cost was €2,515 for admissions resulting in live discharge, and €3,457 for the deceased.
ConclusionThe average direct cost of adult hospitalizations associated with CAP amounted to €2,707 in mainland Portugal from 2000 to 2009, showing an increase of 37.5% in hospitalization cost of living and deceased patients. The economic impact of CAP-related hospital admissions justifies the need for better implementation of preventive measures.
Community-acquired pneumonia (CAP) is a major public health problem, and a significant cause of mortality and morbidity.1,2 The incidence of CAP in adults varies between countries, and is estimated to reach up to 12 cases per 1000 individuals per year.1 In mainland Portugal, the annual incidence of hospital admissions for CAP was 3.61 per 1000 adult inhabitants from 2000 to 2009, and 13.4 per 1000 inhabitants in the population over 65 years of age.3
Treatment of patients with CAP at any level of medical care is associated with significant direct and indirect costs, which are further pronounced at the hospital level. Hospitalization costs for CAP are estimated to represent the largest part of the annual direct costs, which are between 8.4 and 10 billion Dollars in the United States (US),4 and 10.1 billion Euros in Europe.5 In the US, approximately 40% of CAP episodes require hospitalization with an average 5.6 days of hospital stay, incurring a direct cost of US$18,000 per episode.2
Few studies are available on the economic impact of pneumonia. Some European studies show a considerable difference between the cost of patients treated in an outpatient setting and a hospital setting. In a study published in 2004 in Spain between 1993 and 1995 with 292 patients, the average direct cost of outpatient treatment per patient was €196 versus an average direct cost of €1,553 in hospitalized patients.6 In Italy, a study with 120 patients between 1999 and 2000, the average cost of medical care per patient, including a follow-up period of 6 months, amounted to €1,586.7 These two studies did not include patients admitted to the ICU. In Germany, a multicenter study performed in the first semester of 2003 with 580 patients and 13.8% of patient admitted to ICU, the average direct cost of hospitalization was US$1,333 with a maximum value of US$9,488 and the major determinants of cost were length of hospital stay and ICU admission.8
In Portugal, there are no studies on the economic impact of hospital admissions of adults with CAP. The existence of a centralized database in the Portuguese Health System Central Administration (Administração Central do Sistema de Saúde – ACSS) containing clinical and administrative information on hospital admissions within the Portuguese National Health Service (Serviço Nacional de Saúde – SNS) allow a better characterization of the economic impact of CAP, and in particular, the direct cost of hospital admissions.
The aim of this study was to characterize the direct cost of hospital admissions for CAP in mainland Portugal, including the average direct cost per day, per hospitalization, and by outcome (living or deceased). Based on the average cost per day, an estimate was made on the time required to reach 1 million Euros of expenditure.
Materials and methodsThe ACSS, an entity under the Portuguese Ministry of Health, contains the administrative and clinical data of all hospital admissions within the Portuguese National Health Service, which covers almost the entire population resident in mainland Portugal, i.e., approximately 10 million inhabitants. Clinical information, including diagnoses and procedures, is coded by a medical team specifically trained in coding using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM).9
In this observational descriptive study, a retrospective analysis of the ACSS data was carried out, covering a period of 10 years between 2000 and 2009. Inclusion criteria were hospital admissions of adults with a main diagnosis of pneumonia (ICD-9-CM 480-486 and 487.0). Those excluded were patients under 18 years old, hospitalizations with pneumonia as secondary diagnosis, tuberculous pneumonia and obstructive pneumonia (e.g., associated with pulmonary neoplasia), patients with HIV infection (ICD-9: 042-044 and/or DRG 488, 489 or 490), patients immunocompromised due to antineoplastic or immunosuppressive therapy (E933.1), and transplant patients (V42). Data from ward and ICU admissions were treated jointly since the database did not allow for separate analysis. Patient data was kept anonymous throughout the study.
According to the official Portuguese ordinance regarding diagnosis-related groups (DRG), the direct cost of hospitalization was calculated in accordance with the amount established for the respective year of hospitalization.10 The total direct cost of hospital admissions between 2000 and 2009 was analyzed to calculate the average cost by year, by day and according the discharge outcome (living or deceased) using a Microsoft Excel® spreadsheet (Microsoft Corp., Redmond, WA, USA).
ResultsIn mainland Portugal, 7,849,266 hospital admissions were recorded between 2000 and 2009 among individuals aged 18 years or more. Of these, 294,027 (3.7%) were diagnosed as CAP according to the inclusion criteria of the study. 164,655 (56%) patients admitted were male and 129,372 (44%) were female. The median age was 77 years, corresponding to a mean (SD) of 73.1 (16.0) years, with a steady increase (5%) of the mean age over the 10 years (Table 1). The annual average incidence of hospitalization was 3.61 per 1000 adult population, and an increase in incidence from 1.02 to 13.40 per 1000 inhabitants was observed in the age range of <65 and ≥65 years. Overall, there was an increase of 64.7% in the number of hospital admissions.
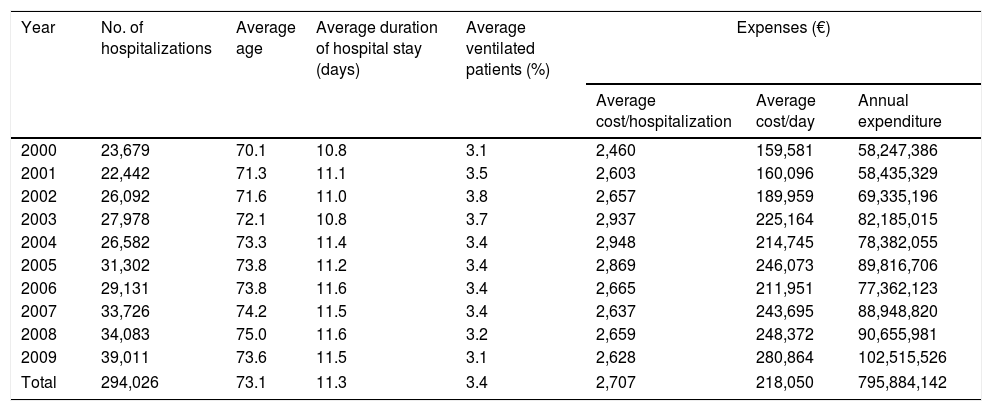
Direct costs of hospitalization for CAP between 2000 and 2009 in mainland Portugal, by hospital admission, daily and annual expenses (source ACSS).
| Year | No. of hospitalizations | Average age | Average duration of hospital stay (days) | Average ventilated patients (%) | Expenses (€) | ||
|---|---|---|---|---|---|---|---|
| Average cost/hospitalization | Average cost/day | Annual expenditure | |||||
| 2000 | 23,679 | 70.1 | 10.8 | 3.1 | 2,460 | 159,581 | 58,247,386 |
| 2001 | 22,442 | 71.3 | 11.1 | 3.5 | 2,603 | 160,096 | 58,435,329 |
| 2002 | 26,092 | 71.6 | 11.0 | 3.8 | 2,657 | 189,959 | 69,335,196 |
| 2003 | 27,978 | 72.1 | 10.8 | 3.7 | 2,937 | 225,164 | 82,185,015 |
| 2004 | 26,582 | 73.3 | 11.4 | 3.4 | 2,948 | 214,745 | 78,382,055 |
| 2005 | 31,302 | 73.8 | 11.2 | 3.4 | 2,869 | 246,073 | 89,816,706 |
| 2006 | 29,131 | 73.8 | 11.6 | 3.4 | 2,665 | 211,951 | 77,362,123 |
| 2007 | 33,726 | 74.2 | 11.5 | 3.4 | 2,637 | 243,695 | 88,948,820 |
| 2008 | 34,083 | 75.0 | 11.6 | 3.2 | 2,659 | 248,372 | 90,655,981 |
| 2009 | 39,011 | 73.6 | 11.5 | 3.1 | 2,628 | 280,864 | 102,515,526 |
| Total | 294,026 | 73.1 | 11.3 | 3.4 | 2,707 | 218,050 | 795,884,142 |
The average duration of hospital stay was 11.3 days, and the percentage of mechanically ventilated patients was 3.4%. These figures remained constant throughout the period analyzed (Table 1).
Global direct cost amounted to approximately €800 million, corresponding to an annual average of €80 million, and a daily average of €218,050 (Table 1). Each hospitalization had an average direct cost of €2,707. Over the 10 years analyzed, the average cost of hospitalization increased by 6.8%, from €2,460 in 2000 to €2,628 in 2009. The annual expenditure almost doubled due to the increase in the number of hospitalizations, from €58,247,386 to €102,515,526 respectively, which corresponds to an increase of 76.0%.
The intra-hospital mortality rate was 20.4% (59,925 patients) with deaths in all age groups. Analyzed by discharge outcome, the average hospitalization cost resulting in live discharge was €2,515, and for the deceased it amounted to €3,457, marking a difference of 37.5%.
Considering the inpatient treatment of CAP and using an estimated average daily cost of 218,050 Euros, it took only 4.6 days to reach 1 million Euros of expenditure.
DiscussionA total of 294,027 hospital admissions for CAP were assessed, which corresponded to 3.7% of total hospitalizations. The total direct cost of hospitalization for CAP amounted to approximately 800 million Euros, corresponding to an annual average of 80 million Euros, a daily average of €218,050, and an average direct cost of €2,707 per hospitalization, regardless of the inpatient setting (ward or ICU).
Over the studied period, there was an increase of 64.7% in the number of hospital admissions, and of 5.0% in the mean age of hospitalized patients. Meanwhile, no significant increase was observed in the duration of hospital stay and the percentage of patients that underwent invasive mechanical ventilation, which could be an indirect indicator of severity. This increase in the number of hospitalizations may explain the 76.0% raise in direct annual cost over the same period from €58,247,386 in 2000 to €102,515,526 in 2009. Given that the rate of hospital admissions for CAP in patients aged ≥65 is five times higher than that of patients <65 years of age, this rising trend in costs over the years is considered to be equally correlated with age. However, other factors must be taken into account, namely the different annual distribution of admissions GDH's and the increase cost of GDH's over the time period analyzed.
In the data analyzed, the average daily cost of hospitalization with live discharge was €2,515, and the cost for the deceased was €3,457, showing an increase of 37.5%. In the literature review, we did not find any data on direct cost according to the outcome of hospitalization, which precludes a comparison with our figures. It is assumed that the cost for deceased patients is higher due to a greater consumption of resources, and most likely, the need for admission to the ICU. The period analyzed (2000–2009), the number of patient (294,026), the inclusion of ICU patients, and the different methodology in our study may have contributed to an average direct cost higher than the reported amounts of €1,553 in Spain,6 €1,586 in Italy7 and US$1,333 in Germany.8
The data examined allows us to quantify the direct costs of hospitalization for CAP in mainland Portugal (10 million inhabitants), which add up to one million Euros every 4 days and 14h (4.6 days).
It should be noted this study covers a period during which adult conjugated pneumococcal vaccine was not yet available and the national influenza vaccination coverage rate ranged from 14.2 to 17.5%.11 The present study showed preventive measures are another factor to take into account. These should include intervention in lifestyle risk factors as well as influenza and pneumococcal vaccination.12
This study has several limitations. This is a descriptive retrospective administrative data-based study with coded clinical information that only allows direct hospitalization costs to be determined. As such, it is not possible to assess the severity of the pneumonia cases, nor to identify the inpatient setting, that is, admission to a ward or the ICU. The good hospital coverage in Portugal, ease of access, and fear of dying at home may justify the inclusion of patients with end-of-life pneumonia. This population will understandably increase average length of stay as well as cost, particularity in the older age groups. Similarly, some cases of nosocomial pneumonia have been included. Despite these limitations, the methodology used is valid, and has been applied in multiple studies carried out in various countries.3,13–16
In conclusion, the high economic impact of hospital admissions for CAP, coupled with an aging population and an increase in co-morbidities, decisively highlights the importance of better implementation of preventive measures.
FundingNone declared.
Conflicts of interestAll the authors have nothing to disclose.
The authors also thank the Portuguese Health System Central Administration under the Ministry of Health (ACSS/MS) for allowing access to the data.