Nocardiosis is a rare bacterial infection caused by Nocardia spp. Lung is one of the most affected organs, but it may involve other tissues, such as central nervous system and skin.1 It is usually associated with immunosuppression but it might occur in immunocompetent patients.2
Radiological appearance is widely variable. It might present as pulmonary nodules, consolidations, cavitated masses or pleural effusions,3,4 which is why it can be confused with other infectious pathologies or malignancy.
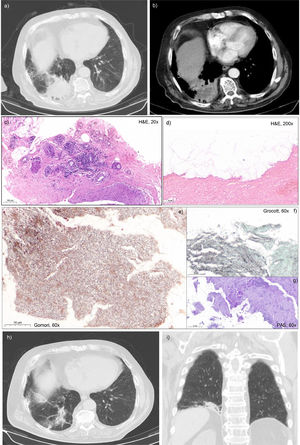
We report the case of a 73-years-old man, former smoker (45 packs/year), with known history of hypertension, cerebrovascular disease and anxiety. He was referred to our department due to persistent cough and hemoptoic sputum for 6 months, without any others symptoms, and treatment failure after 2 empiric antibiotic courses with persistent heterogeneous mass on radiology imaging. Physical examination revealed decreased breath sounds in the lower third of the right hemithorax and chest-X-ray showed the reported heterogeneous hypotransparency in the right base. Blood analysis was unremarkable apart from an elevated c-reactive protein (82.7 mg/L). Chest CT scan (Fig. 1 (a) and (b)) confirmed an irregular lung mass in the right lower lobe, measuring 6.04 × 5.21 × 3.82 cm, heterogeneous, with spiculated borders and small cavitations inside, along with some mediastinal adenopathies, characteristics suggestive of malignant lesions. Given the known risk factor of smoking, the lasting clinical condition without treatment response and the suspected characteristics of the lung mass on CT imaging, a lung cancer diagnosis was hypothesized and transthoracic biopsy was performed. Histology analysis on routine haematoxylin-eosin (H&E) stain revealed a chronic inflammatory infiltrate, with no cytological atypia observed, and with higher amplification evidence of numerous thin, filamentous, tree-like branching rods (Fig. 1 (c) and (d)). The use of modified Gomori's and Grocott-Gomori's methenamine silver stains allowed identification of these colonies of branching hyphae-like appearance microorganisms, periodic acid-schiff negative, compatible with infection by Nocardia spp (Fig. 1 (e), (f) and (g)).
(a) and (b) Chest CT scan showing a heterogeneous lung mass, with irregular and spiculated borders and small cavitations inside, measuring 6.04 × 5.21 × 3.82 cm and located in the right lower lobe; (c) Trans-thoracic biopsy core at 20x routine haematoxylin-eosin stain (H&E) showing moderated perivascular chronic inflammatory infiltrate of the fibrous parenchyma, almost devoided of epithelial component and without evidence of malignant neoplasia; (d) High power field (H&E, 200x) showing the bacterial colony where the tree-like branching filamentous rods of Nocardia spp. are evident; (e) Modified Gomori's method for reticulum stain (60x) also highlights the fungi-like morphology of Nocardia spp. (f) Grocott-Gomori's methenamine silver stain (60x) reveals in black the branching hyphae appearance of the bacteria. (g) The periodic acid-Shiff (PAS) stain 60x was negative for fungi content. (h) and (i) Chest CT scan revaluation after 6 months of treatment shows structural changes at the level of the right lung base where an area of irregular densification with disorganization of the surrounding tissue was still identified.
The sputum study was not successful for microbiological identification. The patient refused other invasive procedures, namely bronchoscopy.
He was admitted for empirical intravenous treatment with Trimethoprim/Sulfamethoxazole (TMP/SMX) 15 mg/kg per day.5 Four weeks later, given good clinical response and radiological improvement, he was discharged with maintenance oral TMP/SMX to meet at least six months of treatment. CT scan reassessment 6 months after shown near-complete resolution of the mass and fundamental sequelae alterations at the level of the right lung base (Fig. 1 (h) and (i)). At the time this report was written, the patient was asymptomatic and there was no radiological evidence of relapse.
In summary, we presented a rare case of pulmonary nocardiosis in an immunocompetent patient, without relevant medical conditions impairing his immune system, and who was first evaluated due to neoplastic suspicion.
Since the symptoms are nonspecific the diagnosis of Nocardia pneumonia is challenging.1–4 In this case, as microbiological identification was not possible, the diagnosis relied on histologic examination and was supported by remarkable clinical and radiological improvement after proper antibiotherapy. When sensitivity testing is not possible, a first course of intravenous therapy with TMP/SMX for at least 2–3 weeks, followed by oral therapy is recommended.5 Depending on the clinical evolution, the total duration of treatment can last up to 12 months in severe cases.5,6 Keeping a close follow up is crucial.
The prognosis depends on the extent of the disease and comorbidities, but an early diagnosis and timely treatment are associated with a decrease in mortality and a lower risk of relapse.1,5,6
Although there are some reported cases in immunosuppressed patients, the information about clinical features and outcome of pulmonary nocardiosis in immunocompetent patients is still sparse.