Despite aggressive treatment, sarcoidosis may be debilitating and progressive. The role of tumor necrosis factor (TNF) ap in the genesis of granulomas is ambiguous. It has proved to be critical in the formation and maintenance of granulomatous inflammation and its antagonist, Infl iximab, has therefore been used with success in the treatment of patients with sarcoidosis. There are, however, reports of onset of sarcoidosis in patients treated for other conditions and where there had been no outbursts before submission to this therapy. We used Infl iximab in the treatment of patients with sarcoidosis who either had not responded to corticosteroids and other conventional drugs or had developed unacceptable side effects to these drugs. The initial dose was 5 mg/kg body weight and subsequent doses were given at weeks 2, 4 and then every other 8 weeks for a total period of one year. We treated ten patients with biopsy proven sarcoidosis, five men and five women, with a mean age of 47.1 years ranging from 28 to 63 years of age. Three patients had severe neurological symptoms, two had hepatic cirrhosis, one had granulomatous inflammation of the lachrymal gland and had already undergone repeated surgery, one had extensive pulmonary involvement (stage III), one had disfiguring lupus pernio and two presented disabling cutaneous nodules. Eight patients had more than one organ with evidence of disease. All patients were submitted to at least seven infusions of Infliximab. In four patients the dosage of corticosteroids or other immunosuppressive drugs was suspended, in three the dosage was reduced and in one, corticosteroids were added to the Infl iximab therapy. In five of the patients there was an important improvement. One of the patients with neurological symptoms displayed a complete recovery, while another had significant improvement of vision deficit enabling her to read again. Two patients withdrew from therapy, one due to lack of improvement of neurological symptoms and the other due to the onset of organizing pneumonia spawned by Infl iximab. Two patients developed anti-histone antibodies during treatment.Infl iximab seems effective in treating patients who are either resistant or develop side effects to a standard regimen of corticosteroids and immunosuppressive agents. These patients, treated with Infl iximab, should be under tight surveillance in order to quickly identify possible secondary effects.
Apesar de tratamento agressivo e atempado, a Sarcoidose pode ser, por vezes, uma doença progressiva e bastante debilitante. O papel do factor de necrose tumoral (TNF)-ap na génese dos granulomas é ambíguo. Por um lado a sua presença é necessária para a formação e manutenção da inflamação granulomatosa, sendo, portanto, o seu antagonista utilizado com sucesso no tratamento de doentes com sarcoidose; por outro lado e para outras situações, há referência do aparecimento dessa patologia em doentes submetidos a Infl iximab. O Infl iximab foi por nós utilizado no tratamento de doentes com sarcoidose que não apresentavam resposta à corticoterapia ou a outras terapêuticas convencionais ou que desenvolviam efeitos secundários inaceitáveis a essa terapêutica. A dose inicial foi de 5 mg/Kg de peso e as doses subsequentes foram administradas na 2.ª semana, na 6.ª semana e depois, durante o período de um ano de 8 em 8 semanas. Dez doentes com diagnóstico de sarcoidose por biopsia, iniciaram terapêutica com este fármaco. Destes cinco eram homens e cinco mulheres, com uma idade média de 47,1 anos, variando a idade entre 28 e 63 anos. Três doentes apresentavam sintomas graves do sistema nervoso central, dois, cirrose hepática, uma inflamação granulomatosa da glândula lacrimal já submetida a múltiplas cirurgias, uma com envolvimento pulmonar extenso (estádio III), uma, com lúpus pérnio desfigurante e dois, com nódulos cutâneos desfigurantes. Oito doentes apresentavam mais do que um local de doença. Todos os doentes completaram pelo menos sete ciclos de tratamento. Em quatro doentes a dose de corticóides ou de outra terapêutica imunosupressora foi suspensa, em três foi reduzida, e apenas em uma doente foi necessário juntar corticóides à terapêutica com Infl iximab. Cinco doentes apresentaram uma melhoria significativa. Um dos doentes com sintomas neurológicos apresentou resolução total, enquanto que a segunda melhorou substancialmente o seu deficit visual permitindo que voltasse a ler. Dois doentes suspenderam terapêutica, uma por falta de melhoria dos sintomas, neurológicos e outra por aparecimento de pneumonia organizativa durante o tratamento com Infl iximab. Três doentes desenvolveram anticorpos anti-histonas durante o tratamento. O Infl iximab parece ser eficaz no tratamento de doentes com sarcoidose refractária ou que desenvolvem efeitos secundários ao regime terapêutico habitual de corticóides ou outros agentes imunosupressivos. No entanto é necessário manter uma vigilância apertada destes doentes para identificar rapidamente efeitos secundários que possam surgir.
Sarcoidosis is a multisystem granulomatous disorder of unknown origin, characterized by the widespread presence of noncaseating granulomas. Despite aggressive treatment, sarcoidosis may be debilitating and progressive. Although there is no cure for sarcoidosis, corticosteroids are universally used for suppressing the progressive and harmful granulomatous inflammation associated with the disease. Unfortunately, many patients develop intolerable side effects and, in such situations, a number of alternative drugs, including immunosuppressive agents, non-cytotoxic anti-inflammatory agents and others have been used despite the fact that these drugs are not consistently effective and many have serious side effects.1
Recent studies point to the antagonist of tumour necrosis factor (TNF) α as an alternative in some patients with sarcoidosis. The role of TNF α in the genesis of granulomas is ambiguous. It has proved to be critical in the formation and maintenance of granulomatous inflammation and therefore, its blockage is used with success in the treatment of patients with sarcoidosis. Infliximab, a tumour necrosis factor antagonist, blocks the effect of tumour necrosis factor and exerts a beneficial effect by controlling sarcoidosis. However, there are reports of onset of sarcoidosis in patients who have been submitted to this therapy for other conditions.
We present the results of ten sarcoidsis patients with multisystemic involvement or resistant to corticotherapy who were followed in our clinic and treated with infliximab.
Materials and methodsBetween 2006 and 2009, ten patients with sarcoidosis who were followed-up at our outpatient Pulmonology clinic in Hospital de Santa Maria received infliximab. These patients had clinical as well as histological evidence of sarcoidosis and they were either resistant to treatment with corticosteroids and/or alternative drugs or had developed unacceptable side effects to these drugs; diabetes, depressive syndrome, psychotic behaviour, arterial hypertension (HTA) and osteoporosis.
All patients had a negative tuberculin test and were submitted to bronchoscopy to rule out infection by Mycobacterium tuberculosis.
Infliximab was administered in an outpatient infusion clinic. The initial dose was 5mg/kg body weight and a subsequent dose was given at weeks 2, 6 and then at 8-week-intervals until one year of therapy was fulfilled.
In most of the patients, corticosteroids and other immunosupressors were reduced or discontinued.
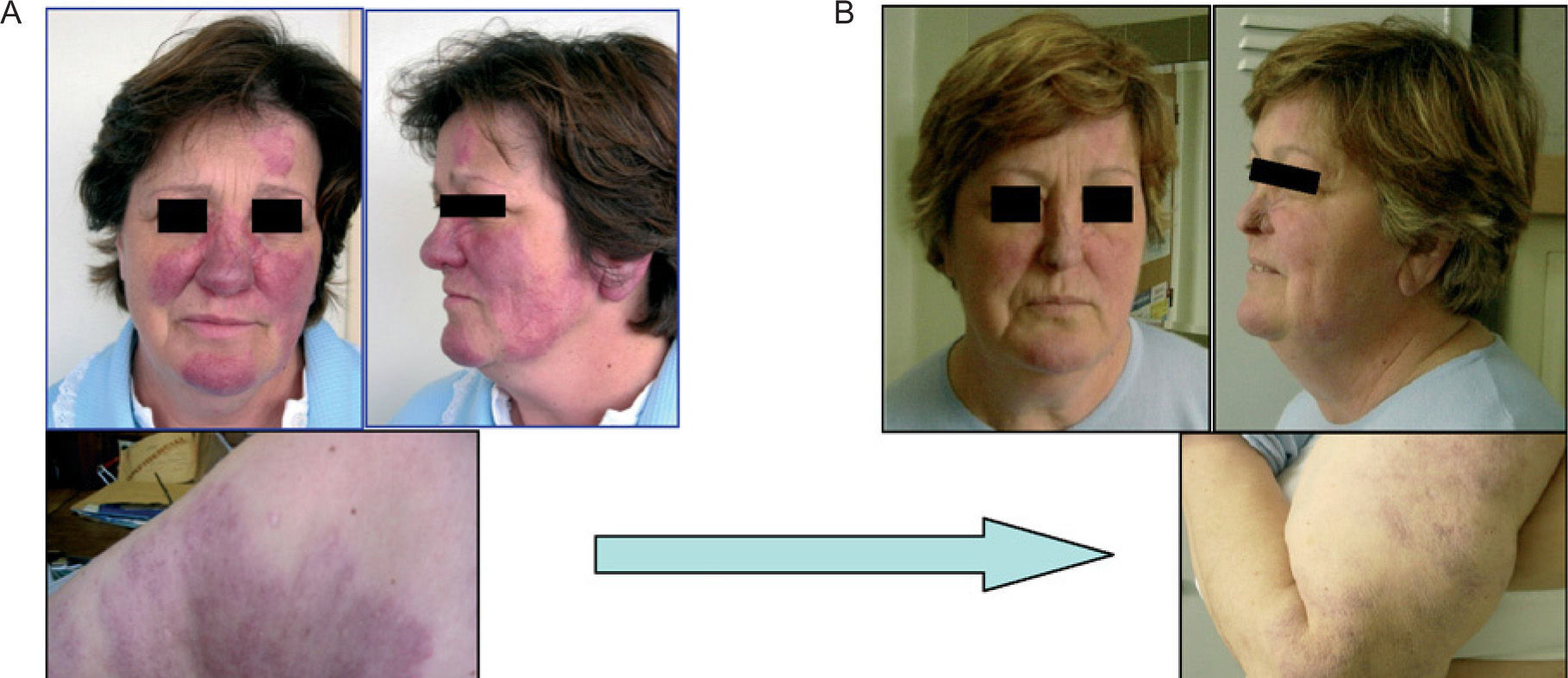
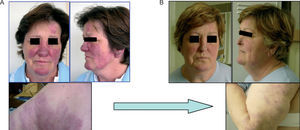
ResultsPatient no. 1At the age of 23 this 54-year-old Caucasian woman had been diagnosed with lupus pernio. Pulmonary involvement (stage III) was identified in 1991 at the age of 39. At this point she had no respiratory symptoms and pulmonary lung function tests showed a reduced diffusion capacity (DLCO-74mmol/min/kPa) so treatment with resochine was started as the skin was involved.
In 1992 there was a worsening of skin disease; lesions were now more evident leading to social exclusion, so steroid therapy was initiated. There was a slight improvement after treatment.
Over the next twelve years, the patient was treated with steroids when there was a functional and respiratory deterioration, with reasonable response and resochine when skin lesions became more prominent.
In 2004 she showed radiological and functional worsening but with no new symptoms, so at this time, due to hypertension, obesity and a depressive syndrome, no treatment was initiated.
In March 2006 she had dyspnoea on exertion, small joint pain and lupus pernio became more exuberant and disfiguring. Thoracic CT scan evidenced enlargement of adenopathies, thickening of bronchovascular bundles and bronchiectasis (stage II). Laboratory tests showed elevated serum angiotensin converting enzyme (SACE) (148 U/L) and arterial blood hypoxemia (PaO2, 67mmHg). Pulmonary function tests showed reduction in diffusing capacity DLCO, 55mmol/min/kPa and DLCO/VA, 50mmol/min/kPa.
She started therapy with azathioprine and prednisolone and although there was some improvement, her hypertension became more difficult to control, there was a worsening of her depressive symptoms and she also had a significant weight gain (87kg to 94kg) and so infliximab was started. This therapy combination led to important hepatic toxicity (ALT-7 × N, AST-4 × N, Gamma GT-50 × N and LDH-2 × N) which led to suspension of azathioprine and with only infliximab and prednisolone there was a normalization of hepatic enzymes.
After five infusions of infliximab the patient had no limitation for medium efforts and her skin lesions had improved significantly (Fig. 1). Thoracic CT scan also showed improvement, at this time there was only evidence of stage I with smaller adenopathies. Arterial blood gas evaluation was normal (PaO2-88mmHg) and diffusing capacity was closer to normal range (DLCO-70mmol/min/kPa and DLCO/VA-68mmol/min/kPa).
The patient completed 12 infusions and, 18 months after last infusion her disease is stable without the need of any therapy.
Patient no. 2In 1992 this 51-year-old caucasian male, former smoker (5 Packs/year) presented with exuberant and disfiguring cutaneous nodules in the eyelids, nose, hands and feet. At this time he had stage I pulmonary involvement (bilateral hilar adenopathies) and hepatic manifestations (hepatomegaly with elevation of hepatic enzymes —AST [2 × N], ALT [3 × N] and Gamma-GT [3 × N]—). Laboratory tests showed elevation of SACE and there was a slight reduction in diffusing capacity (DLCO, 75mmol/min/kPa).
Between 1993 and 2007 he was treated with deflazacort with minimum effective dosage of 30mg and 15mg every other day. During this period he developed subcapsular cataracts, aggressive behaviour with need of hospitalization and hyperuricemia that was very difficult to manage.
From 2007 the patient was followed at our clinic, still with a high dose of steroids (deflazacorte 15/30mg/day), stage I pulmonary involvement and multiple cutaneous nodules in fingers, nose and elbows and also exuberant gout tophi both highly disfiguring and physically disabling. He also had lupus pernio, cutaneous plaques in the dorsum and face and also suffered from diffuse joint pain. Laboratory tests showed elevation of hepatic enzymes, SACE and uric acid (between 10.5 and 11mg/dL) even under treatment with steroids, colchicine, nonsteroidal anti-inflammatory drugs and allopurinol.
Due to the long evolution of disease, the magnitude of cutaneous lesions, their professional and social impact and the dependence of steroids we decided to start therapy with infliximab.
He completed one year of therapy (9 infusions) with no side effects and excellent response; cutaneous plaques and 95 % of cutaneous nodules disappeared leading to significant aesthetic improvement especially in the face, hands and arms. Pulmonary involvement remained stage I but less exuberant and laboratory tests showed normal hepatic (except for Gama GT which was only slightly elevated) and SACE results.
It was not possible to suspend or reduce steroid therapy due to persistent hyperuricemia. During treatment with infliximab the patient had worsening of gout with more episodes of acute arthritis attacks and more intense episodes of joint pain.
Patient no. 3In 1991 this 60 year-old caucasian male, former smoker, referred had painful and disfiguring cutaneous nodules (diameter 5cm) that did not allow him to lie down on his back. He also complained of fatigue and reduced tolerance to medium efforts. There was also pulmonary involvement stage II. Laboratory tests showed elevation of SACE and lymphocytosis (28 %) in bronchoalveolar lavage. Pulmonary function tests had reduced FEV1/FVC (74 %). Diagnosis of sarcoidosis was confirmed with mediastinal lymph node biopsy.
He was submitted to steroid and hydroxichloroquine therapy with no improvement and, because these lesions were very disabling infliximab therapy was proposed.
The patient completed 11 infusions, with total resolution of pulmonary involvement and a 50 % reduction in the number of cutaneous nodules and with no more pain caused by these. No side effects were registered and it was possible to suspend therapy with steroids and hidroxichloroquine. Pulmonary function tests became normal and he stopped complaining of fatigue.
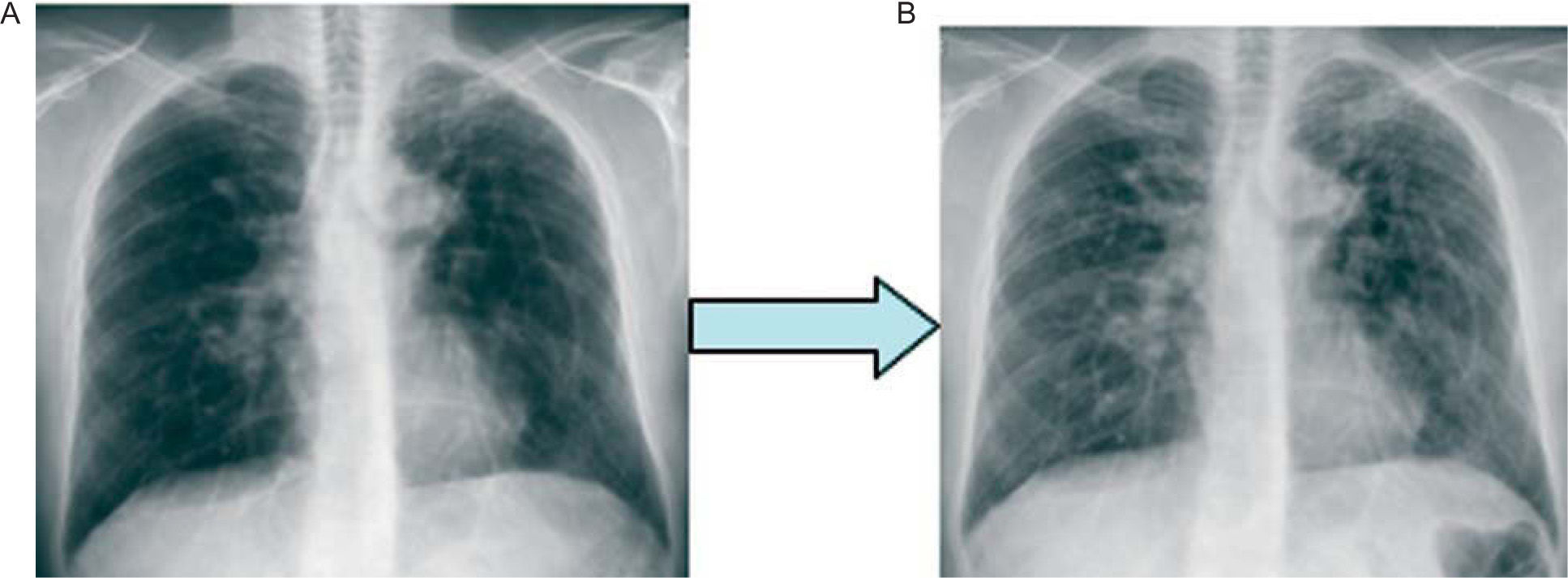
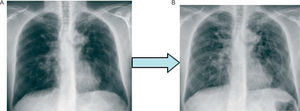
Patient no. 4In 1982 this 47 year-old Caucasian male was diagnosed with splenomegaly. He was 18 years old when he underwent abdominal exploratory laparoscopic surgery that was inconclusive (abdominal adenopathies); at the age of 21 he was submitted to spenectomy. The first changes in chest x-ray film (Stage II) came at the age of 26 leading to a pleuroscopy with consequent diagnosis of sarcoidosis. At this time there was also hepatic (hepatomegaly and elevation of hepatic enzymes), cutaneous (cutaneous plaques), lymph node and etmoido-maxilar involvement. The patient had symptoms of shortness of breath, fatigue and dry cough.
He had many periods of treatment with steroids with worsening after suspension of therapy and intolerance to other medications: azathioprine, metothrexate and hidroxichloroquine. Before treatment with infliximab the patient was dependent on deflazacorte (7.5mg/day) and under this therapy there had been evolution of pulmonary involvement to fibrosis (stage IV) (Fig. 2A and B).
He started infliximab due to the great extent and instability of disease and dependence on steroids.
The patient completed eight infusions of infliximab throughout one year and although there was subjective improvement, we were not able to quantify it. There was a gradual reduction in steroid therapy until 3mg/day which he still maintains. He developed high auto-antibodies (ANA) and Anti-histone titers without having any new symptoms.
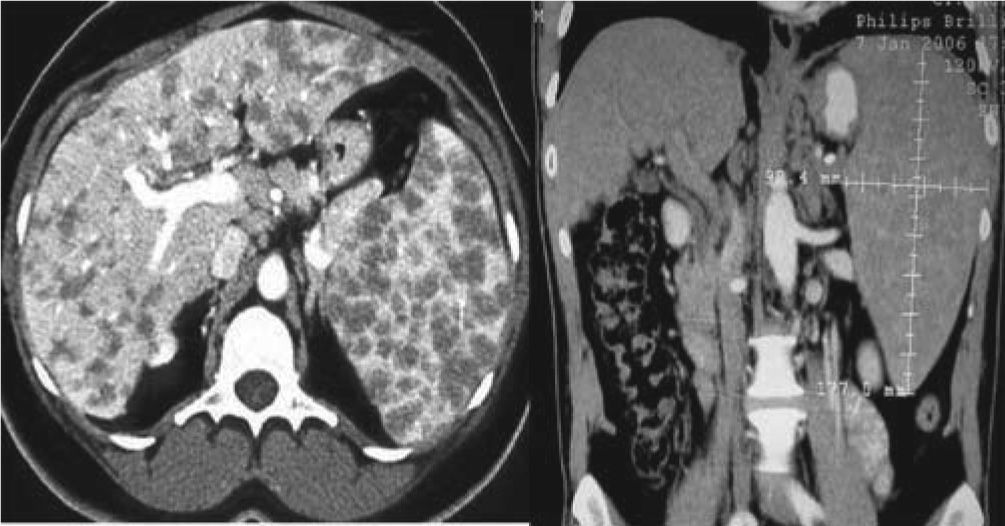
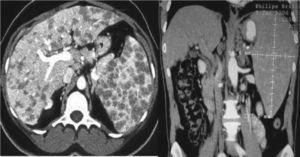
Patient no. 5In the year 2000 this 63 year-old caucasian male was referred to our clinic due to persistent elevation of liver enzymes. The hepatic biopsy revealed non-caseating granulomas. Although he did not have any symptoms there was hepatosplenomegaly and evidence of haematological (leucopenia, linfopenia and neutropenia) and stage III pulmonary involvement (Thoracic CT scan with micro nodular pattern in peri-hilar area with thickening of interlobular septa in the right inferior lobe). The bronchial biopsy performed at this time confirmed the diagnosis revealing non-caseating granuloma.
He was submitted to therapy with azathioprine which was suspended due to worsening of leucopenia and trombocitopenia with no significant improvement of hepatic enzymes. There was, however, some recovery of the pulmonary involvement.
The patient started treatment with infliximab due to rapidly progressive hepatic cirrhosis with no alternative treatment; he did not present criteria for liver transplant.
He completed eight infusions and during this time liver enzymes fluctuated but rarely in the normal range and leucopenia and trombicitopenia were persistent. He developed high ANA. Anti-histone and anti DS DNA titers without developing any new symptoms. Thoracic CT scan showed total resolution of lung parenchymal involvement but revealed the presence of pulmonary hypertension, moderate splenomegaly and esophageal varices (Fig. 3).
Patient no. 6In 2001 this 29 year old caucasian male was diagnosed with sarcoidosis after investigation of complaints of astenia and weight loss, the bronchial biopsy performed showed non-caseating granulomas. At this time he had Stage II pulmonary (hilar and mediastinal adenopathies and micronodulation in the pulmonary lower lobes) and myocardial (very suggestive myocardial scintigraphy) involvement and so low dose steroid therapy was initiated.
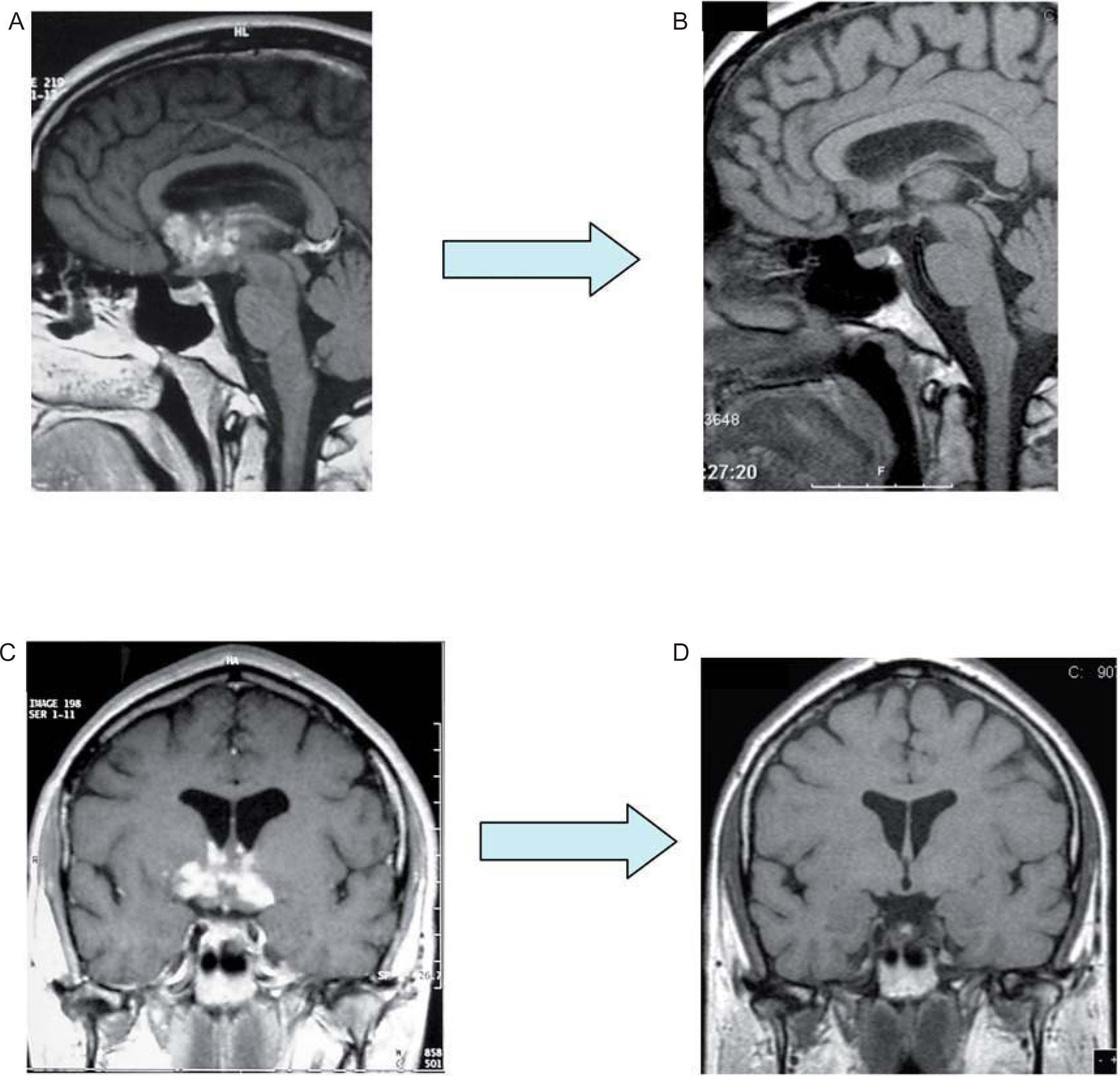
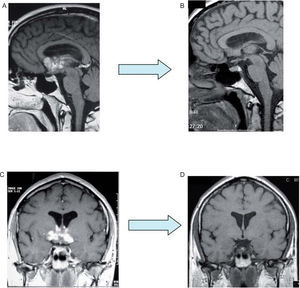
He was asymptomatic until 2006 when he developed facial palsy, dysarthria, diplopia and ataxia suggesting a neurological involvement of sarcoidosis, brain magnetic resonance imaging (MRI) showed infiltration of hypothalamus and peri-chiasmatic region with granuloma and its extension predominantly to right basal ganglia and corpus callosum sub-regions. He was submitted to high dose steroids without possibility of adjustment due to recurrent exacerbations of the disease which led to multiple hospitalizations. Here he was submitted to high dosage of steroids in pulses and in August of 2007 azathioprine (150mg/day) was associated to the 60mg of daily prednisolone.
He was sent to our clinic in February 2008 and considering the resistance to instituted therapy, we decided to suspend azathioprine and start infliximab.
After three infusions and the possibility of reduction of prednisolone to 50mg/day he was hospitalized due to meticilin-sensible Staphylococcus aureus spondylodiscitis and was successfully treated with flucloxacilin for 42 days. After this, prednisolone was reduced to 20mg/day.
After six infusions the patient suffered from a decrease of strength in lower limbs leading to frequent falls, apparently with no related of loss of consciousness. The immediate study showed severe hypernatremia (169.7mmol/L), and after a thorough investigation, diabetes insipidus was excluded and the diagnosis of misalignment of the central osmorreceptor secondary to sarcoidosis was accepted. Successful treatment has consisted of daily ingestion of large quantities of water. A repeated brain MRI showed total resolution of the central nervous lesions (Fig. 4B-D).
He then developed symptoms of postural hypotension and was submitted to cardiac MRI that suggested myocardial involvement by sarcoidosis.
At present, after eleven infusions of infliximab he continues to have frequent symptoms of postural hipotension but has significantly improved mobilization, and has no dysarthria. He still continues with steroid therapy (prednisolone 15mg/day) as well as Infliximab.
Patient no. 7In 2008 this 36 year old caucasian female was diagnosed with sarcoidosis.
She had had a history of epilepsy from the age of 13, stabilized with carbemazepine, and headaches for many years. In March 2008 she referred to intense headaches with a significant loss of vision (more severe in the right eye); a brain CT scan done at this time revealed a lesion in the optic chiasm. Confirmation came with MRI showing an important bi-lobuled lesion that gained contrast suggesting a tumour. She was submitted to steroid therapy with metilprednisolone but because there was no improvement and every time there was a reduction of dosage the symptoms worsened, the patient had a craniotomy with biopsy of the lesión. The result was non-caseating granulomas and cultures for fungi and tuberculosis were negative. Chest X-ray film showed pulmonary involvement stage I, bronchial and transbronchial pulmonary biopsies were negative for granuloma but bronchoalveolar lavage came up with CD4/CD8 lymphocytes of 4.3.
At this point she was sent to our clinic for follow-up, under prednisolone 40mg/day. She then suffered deterioration of the symptoms with loss of vision in the left eye, pain with eye movements and severe headaches. Brain CT scan revealed a new lesion in the left optic nerve. She was submitted to high dose endovenous steroid therapy (metilprednisolone), raised oral prednisolone to 80mg/day and associated methotrexate 15mg/week with significant improvement after one week of treatment.
After two months she began progressively reducing the dosage of prednisolone but by when she got to 60mg/day, there was a worsening of the symptoms, especially in the left eye. Brain MRI scan showed progression of the right lesion and a new lesion in the pituitary stalk which extended through infundibulum until right hypothalamus.
Faced with such a severe clinical and radiological deterioration under such extensive immunosuppression, a significant weight gain (she now weighed 111kg) and the onset of hypertension and diabetes we decided to start infliximab.
After three infusions of infliximab the patient was able to read without any difficulty and the MRI brain scan was normal. Prednisolone was reduced to 25mg/day and methotrexate to 12.5mg/week.
After five infusions the patient developped figurate erithema of the lower limbs suggestive of toxidermia so she was hospitalized and submitted to skin biopsy that showed only an unspecific perivascular lymphocytic infiltrate. At this time Chest X-Ray film and thoracic CT scan showed no changes and ANA titers were negative. During this hospitalization she had Herpes zoster infection in left supraciliary region that was resolved with acyclovir treatment.
She has now completed 6 infusions of infliximab, she is asymptomatic with normal visual acuidity and we have been able to reduce imunosuppression down to prednisolone 15mg/day and methotrexate 10mg/week with consequent weight loss.
Patient no. 8In 1993 this 49 year old caucasian female was diagnosed with sarcoidosis after the excision of a cutaneous nodule in her upper lip. Biopsy revealed non-caseating granulomas. Laboratory tests showed normal range SACE and serum calcium. Two years later she referred an episode of multiple nodules scattered in the lower limbs that disappeared without any treatment, they were not biopsied.
During the following two years the patient referred self-contained episodes characterized by periods of dyplopia and reduced strength in upper and lower limbs (more evident on the left side). Brain MRI scan showed areas of demyelination of the white matter suggestive of multiple sclerosis. She presented a normal electromyography and at this time there was no evidence of sarcoidosis (pulmonary CT scan was normal).
She began immunosuppressive treatment with β-1A interferon but nonetheless she still referred at least twice a year episodes of ataxia, pending foot and paresthesis of upper and lower limbs. These outbreaks were treated with endovenous steroid therapy with resolution within a maximum period of one month.
After the age of 45 the disease stabilized until 2007 when there is onset of new cutaneous lesions (multiple cutaneous nodules scattered in all the body) associated with persistent complaints of pending foot. Skin biopsy revealed multiple non-caseating granulomas and lung CT scan was suggestive of stage I pulmonary disease. Laboratory tests showed normal range SACE and serum calcium and pulmonary lung function tests were normal. Bronchial biopsy showed no granuloma but bronchoalveolar lavage came up with CD4/CD8 lymphocytes of 6.6.
We accepted diagnosis of sarcoidosis with pulmonary stage I, cutaneous and neurological involvement so interferon was suspended and prednisolone was started at a daily dosage of 30mg.
Although there was almost total resolution of lung involvement, she still had neurological symptoms (imbalance and pending foot) and there had been an onset of a severe depressive syndrome secondary to steroid therapy, so we decided to start infliximab. Steroid therapy was gradually reduced until suspended after six infusions. There was significant improvement in the number of symptoms and the pain caused by cutaneous nodules but no significant gain in the neurological symptoms so we decided to suspend infliximab and restart prednisolone in a daily dosage of 10mg and methotrexate 12.5mg/week.
Ten months after suspending infliximab the neurological symptoms have stabilized and it was possible to reduce prednisolone to 5mg/day. She developed high ANA titers without the onset of new symptoms.
Patient no. 9In 1997 this 47 year old caucasian female was diagnosed with sarcoidosis after investigation of persistent leucopenia. At this time she had stage II lung involvement and disfiguring chronic obstruction of both lachrymal glands which lead to permanent suppuration and the need for multiple surgeries.
She was treated with steroid therapy for a year and initially improved but there was recurrent remission after altering medication so we found that the minimum effective dosage was prednisolone 10mg/day and methotrexate 5mg/week. This was enough to ameliorate pulmonary impact (stage I) and to slightly reduce lachrymal gland symptoms.
We started infliximab with the hope of controlling lachrymal suppuration and after four infusions we were successful in suspending steroid and methrotexate therapy. At this time the patient presented new cutaneous vesicular periorbital lesions which were biopsied and were negative for granuloma or for toxidermic lesions.
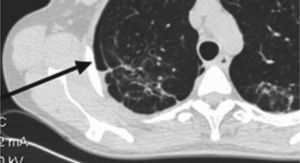
After five infusions she developed new respiratory symptoms, cough and fatigue. Lung CT scan was suggestive of organizing pneumonia so we decided to suspend infliximab. In three weeks time there was spontaneous resolution of this pulmonary lesion and remission of stage II lung involvement and so steroid and methotrexate therapy were re-started (prednisolone 10mg/day and methotrexate 5mg/week).
A few months after the suspension of infliximab the patient had a transient ischemic attack. Brain MRI with gadolinium contrast excluded neurological sarcoidosis and was suggestive of vascular lesion. Anti antiphospholipid titers were found to be positive. She is now treated with oral anticoagulation.
At present, 18 months after the last infusion of infliximab and under a small dosage of therapy (prednisolone 5mg/day and methotrexate 5mg/week), the patient has no symptoms, there is no lachrymal gland suppuration and a complete resolution of lung sarcoidosis (stage 0)
Patient no. 10In 2005 this 41 year old Caucasian female was diagnosed with sarcoidosis following complaints of fatigue, dyspnoea on exertion, myalgia, joint pain and weight loss. She had stage III pulmonary sarcoidosis (extensive micronodular pattern and thickening of bronchovascular bundles) pulmonary lung function tests showed restriction (TLC-75 %) and reduction in diffusion of CO (DLCO-SB-79mmol/min/kPa).
She was treated with steroid therapy with total resolution of micronodular pattern but due to a rapid evolution to stage IV and the onset constitutional symptoms together with disabling joint pain, we decided to start infliximab.
After five infusions of infliximab there was an important improvement in fatigue and joint pain, normalization of diffusion of CO but there was a remission of the micronodular pattern, very evident in the thoracic CT scan. At this time we thought of suspending infliximab but instead we decided to associate prednisolone in a daily dosage of 10mg.
The patient completed 9 infusions of infliximab and now, under prednisolone 5mg/day, she has no micronodulation in the thoracic CT scan but does present some fibrotic changes.
Four months after suspension of infliximab the patient still had joint pain but it is much less severe and there was onset of small pneumothorax in the right side, too small to be drained that is under tight surveillance (Fig. 5).
DiscussionThere are two aspects of the granulomatous response of sarcoidosis: the initial event, leading to granuloma formation, and the evolution of the response as either resolution or chronic disease. In patients with an acute form of the disease, a high proportion of CD4-positive lymphocytes have been identified in bronchoalveolar lavage fluid. These T cells are activated and are associated with macrophage activation, interferon production, and formation of the granuloma and this has been cited as an example of the Th-1 response. In many sarcoidosis patients, the granulomatous response is resolved during the following 2–5 years and is related to an influx of CD-8 positive lymphocytes. The cytokines associated with chronic disease include IL-8, IL-12, and tumour necrosis factor-alpha (TNFα).2
TNFα is a 17.5-kd protein that plays a significant role in antigen-stimulated, cell mediated immune responses and in the development of noncaseating granulomas in a variety of diseases. TNFα has an important role in the pathogenesis of a number of chronic inflammatory diseases. In sarcoidosis, alveolar macrophage-derived TNFα participates in the induction and maintenance of granulomas.3,4 High levels of TNFα and high levels of TNFα seem to correlate with the progression of the disease.
Infliximab is an anti-TNFα monoclonal antibody that adheres to soluble transmembrane TNFα with high affinity and forms a stable complex that blocks the union of this cytokine with its receptor. This blockage leads to the neutralization of TNFα inhibiting its action after its release by pulmonary macrophages and other cells and prevents the formation of granuloma which is an essential step in the pathogenesis of Sarcoidosis. TNFα blocking therapy with infliximab or etanercept is effective in many diseases including rheumatoid arthritis, Crohn's disease, ankylosing spondylitis, and psoriatic arthritis.5–7
In sarcoidosis, there are no guidelines regarding the indications, dose, and duration of therapy, and assessing response of the disease to infliximab. There are however a few studies 1,8–11 providing evidence that this medication is effective in the treatment of some patients with sarcoidosis.
Our study seeks to describe the clinical evolution of a group of sarcodosis patients treated with infliximab. This medication was chosen because patients presented one or more of the following:
- A.
Patients dependent on steroid therapy.
- B.
Patients who did not tolerate the severity of side effects of instituted therapy.
- C.
Patients with no alternative therapies available.
Infliximab was well tolerated by our group of patients. Only two did not complete a complete year of treatment; one, due to lack of response and the second due to onset of organizing pneumonia. There were no cases of lymphomas or other malignant diseases in the patients studied. None of our patients exhibited allergic or anaphylactic reactions.
With the exception of the patient who developed organizing pneumonia with subsequent spontaneous resolution, there were no significant side effects associated with this therapy. As was described by other authors, 12,13 three of our patients developed high ANA and Anti-histone titers without developing any new symptoms. In the patient that developed a transient ischemic attack, the doubt remains whether this was due to antiphospholipid titers and if these appeared secondary to Infliximab therapy.
The clinical presentation of Sarcoidosis can often mimic tuberculosis. This disease was excluded when all patients were submitted to bronchoscopy with negative cultures for Mycobacterium tuberculosis. During the time of treatment with Infiximab, most of our patients did not develop serious pulmonary or extrapulmonary infections, although there was a greater risk of infections due to opportunistic agents.14,15 Not even the two patients with stage IV disease had fungic or other infections.
We do have to mention one patient with supra-ciliary vesicular cutaneous lesions suggestive of herpes zoster and another that was hospitalized due to meticilin-sensible Staphylococcus aureus spondylodiscitis. Both situations were solved with antibiotic therapy.
Infliximab was effective in treating sarcoidosis with cutaneous, neurological, lachrymal gland involvement and also pulmonary in some cases. Patients with hepatic and splenic involvement showed no response to this therapy.
There was a significant improvement in five patients with cutaneous lesions, in some cases with total resolution. Cutaneous involvement has been referred to in the current literature2,9,17,20 as having a significant response to this treatment.
Two out of the three cases of neurosarcoidosis had a fantastic recovery and are at present almost asymptomatic without the need of large doses of immunosupressors. Currently, there is insufficient data to support infliximab as first-line therapy for neurosarcoidosis, but it does hold promise as a potential second-line therapy. It definitely is an option in resistant cases.
In the case of the patient with involvement of the lachrymal gland, this is a less frequent location of sarcoidosis with rare form of presentation. We chose to use Infliximab due to the impact of the symptoms on the patient and the lack of response to other therapies. The result was positive and the patient is now asymptomatic requiring only a low dose of prednisolone and methotrexate.
As far as pulmonary sarcoidosis is concerned, results are variable. All patients had pulmonary involvement ranging from stage I to Stage IV. In four patients there was total resolution and in another four, significant improvement. One of the patients had worsening of the disease under infliximab with the need to associate predisolone. In the last patient there was no change of the pulmonary manifestations.
It was possible to reduce or suspend immunosuppressive therapy in nine of the ten patients which suggests that once the aggressive inflammation is brought under control, this can be maintained with lower dosages of medication.
ConclusionInfliximab seems effective in treating patients who are either resistant or develop side effects to a standard regimen of corticosteroids and immunosuppressive agents.
Infliximab appears to be particularly effective in treating neurological and cutaneous sarcoidosis and it also allows reduction of associated therapies.
There is insufficient data at this time o allow the recommendation of infliximab therapy for first line therapy in cases of Sarcoidosis but it is definitely an option in difficult cases. The optimal dosage, length of treatment and long term toxicity should be evaluated in prospective trials.
However these patients should be followed-up very closely in order to quickly identify possible adverse reactions and the effects of long term therapy are still little known. Reactivation of pulmonary sarcoidosis remains an issue.
- Home
- All contents
- About the journal
- Metrics
- Open access