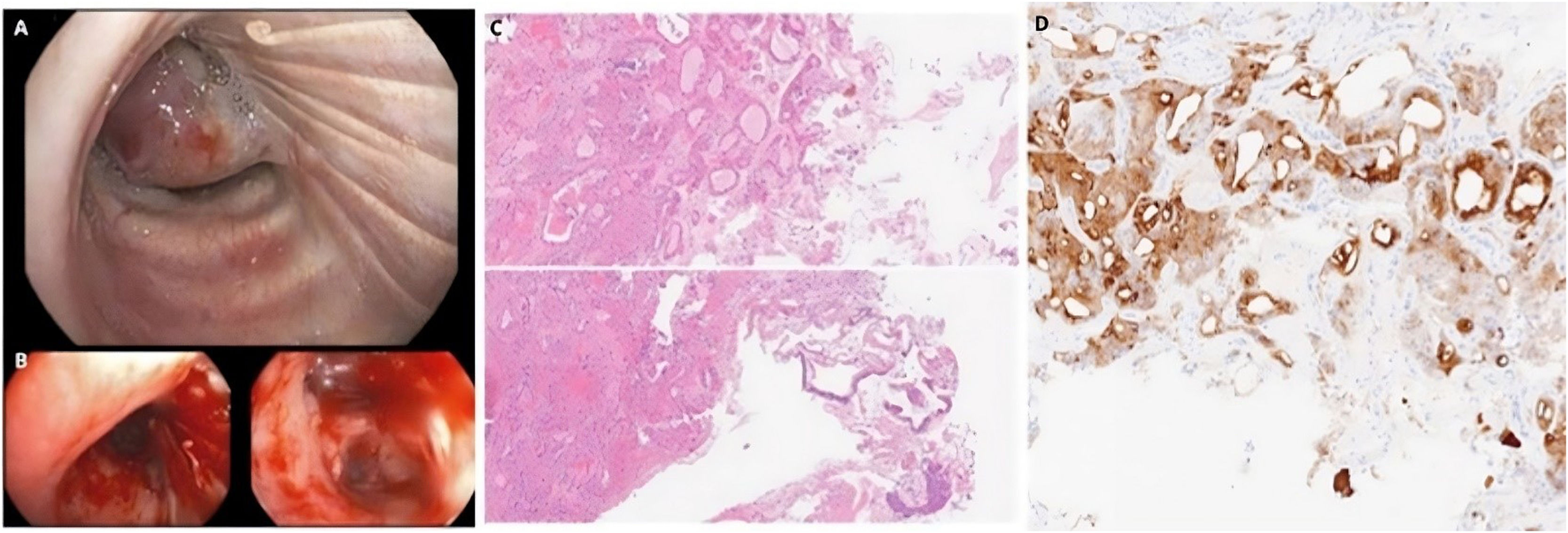
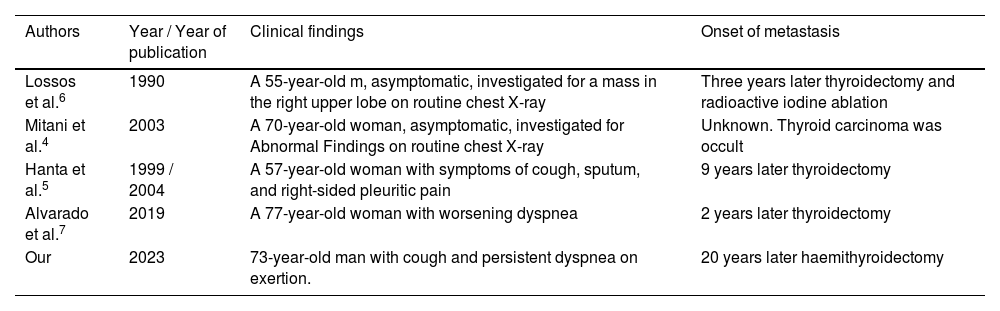
Endobronchial metastasis from extrapulmonary tumors is a rare clinical condition, most often due to systemic spread of breast, kidney, or colorectal cancers.1 Thyroid cancer can lead to bone, lung, liver, or brain metastasis but, like other malignancies, rarely involves the tracheo-bronchial tree.1 Oncocytic thyroid carcinoma (OTC) is a follicular thyroid neoplasm that accounts for 4% of thyroid cancers. It may be extremely aggressive and often tends to spread locoregionally and give rise systemic metastasis.2 Known as Hürthle cell carcinoma, the new WHO 2022 classification of thyroid cancers proposed the current name of oncocytic carcinoma because of its peculiar histological features.3 Oncocytic cells, which can be found in other organs, are in fact cells with different characteristics from the original ones, characterized by eosinophilic cytoplasm due to the presence of numerous mitochondria. These changes may occur with aging, inflammation or generally high levels of oxidative stress as part of a process of metaplasia.3 Essential features of malignancy are vascular and/or capsular invasion.3 Here, we describe the case of a 73-year-old patient, former smoker of 10 cigarettes per day for 15 years (equal to 7.5 pack-year), with endobronchial occlusion of the right upper lobe bronchus (RULB), with a past history of OTC undergone hemithyroidectomy twenty years before. He sought our attention 2 years ago due to the onset of cough in association with persistent dyspnea on exertion for several months. No additional comorbidities were present. Physical examination demonstrated mild reduction of breath sounds in the upper third of right hemithorax. Chest X-ray had raised suspicion of dysventilatory areas of the superior lobe. In consideration of the clinical presentation and medical history, a contrast-enhanced chest computed tomography (CT) was performed, which showed multiple nodules suggestive of metastasis with a particular focus on a solid material, characterized by contrastographic enhancement, located in the RULB and the segmental and subsegmental branches of the anterior bronchus (B3, B3a and B3b). Additionally, some pericentimetric paratracheal and aortopulmonary window lymph nodes were reported. A flexible bronchoscopy was therefore scheduled with diagnostic and therapeutic purposes, to take biopsy samples and obtain recanalization. The procedure revealed a vegetant mass determining stenosis estimated to be 90% of the RULB extended to the right main bronchus (Fig. 1a). The patient then underwent laser-therapy, biopsies and unblocking with jumbo forceps, during the same diagnostic procedure conducted through flexible bronchoscopy (Fig. 1b, after treatment). All these interventions were performed while the patient was breathing spontaneously under moderate analgosedation. Finally, low-power laser therapy was performed on the distal portion of the metastasis that remained macroscopically visible at the level of the RULB. Laser treatment aimed at controlling symptoms and tumor growth. After just one laser session, the patient referred improved exertional dyspnea. Histopathological examination performed on the biopsy material was positive for oncocytic neoplasm (or Hürthle cell neoplasm) with thyroid-derived immunophenotypic characters (Fig. 1c), therefore consistent with metastatic oncocytic carcinoma. In this case, positivity was reported for the following immunohistochemical stains: cytokeratin-19 (CK-19), thyroid transcription factor-1 (TTF-1) and Thyroglobulin (Fig. 1d). The subsequent treatment was guided by the oncologist, who prescribed tyrosine kinase inhibitor therapy (Lenvatinib) on the basis of the appearance of distant bulky metastases and referred the patient to surgery to perform a radical thyroidectomy. The patient also underwent bronchoscopy follow-up, which showed no new endobronchial lesions to date. Based on this rare event, a literature review was conducted to assess the incidence and time of onset of endobronchial metastases from this type of tumor. To the best of our knowledge, this is the first published case of such late-onset of even rare bronchial tree metastasis from OTC. Only four cases of endobronchial metastasis from oncocytic thyroid cell tumor were identified4–7 (Table 1). In all these cases, including ours, it is plausible to suspect a mechanism for the development of endobronchial metastases as a result of lymphatic spread. Involvement of lymph nodes (especially the hilar lymph nodes) was indeed noted in our patient and in some of the cases reported in the literature.
A. Endobronchial mass determining stenosis > 90%; B. Endoscopic image after laser-therapy; C. H&E, 400x Histologic sections on biopsy specimen shows follicular and solid growth of eosinophilic tumor cells, with large and granular cytoplasm, consistent with oncocytic neoplasm (immunostaining not shown); D. 400x Immunohistochemical staining for Thyroglobulin showing expression in follicular structure of tumor cells.
Case report on endobronchial metastases from oncocytic thyroid carcinoma.
| Authors | Year / Year of publication | Clinical findings | Onset of metastasis |
|---|---|---|---|
| Lossos et al.6 | 1990 | A 55-year-old m, asymptomatic, investigated for a mass in the right upper lobe on routine chest X-ray | Three years later thyroidectomy and radioactive iodine ablation |
| Mitani et al.4 | 2003 | A 70-year-old woman, asymptomatic, investigated for Abnormal Findings on routine chest X-ray | Unknown. Thyroid carcinoma was occult |
| Hanta et al.5 | 1999 / 2004 | A 57-year-old woman with symptoms of cough, sputum, and right-sided pleuritic pain | 9 years later thyroidectomy |
| Alvarado et al.7 | 2019 | A 77-year-old woman with worsening dyspnea | 2 years later thyroidectomy |
| Our | 2023 | 73-year-old man with cough and persistent dyspnea on exertion. | 20 years later haemithyroidectomy |
We believe that our case is peculiar, based both on the very rare occurrence and therefore on the considerable latency period between the diagnosis of the primary neoplasm and the subsequent appearance of the metastases. In fact, it is estimated that 25% of cases of OTC may develop metastatic disease, with a median time of 50 months.2 In our report, the time from hemithyroidectomy to the first CT finding of metastatic endobronchial lesion was 20 years. Thus, it represents a late onset of disease recurrence that exceeds the average reported in the literature. In conclusion, we believe that endobronchial occult metastasis should always be suspected and investigated in symptomatic patients with long past history of extra-thoracic primitive neoplasm. This is also the case with OTC, albeit this is a rare occurrence.
ConsentWritten informed consent was obtained from the patient.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
N/A.