Video-assisted thoracoscopic surgery (VATS) is an approach to resection of bronchogenic cysts (BC) which is effective and viable. There may be complications as a result of pericystic adhesions to neighboring structures during dissection. This report describes an unusual case of an operative complication, the rupture of the main left bronchus. The initial VATS approach was converted into a right thoracotomy to remove the cyst and suture the bronchus once adequate exposure was obtained. Bronchus reconstruction failed and a few hours later, it was necessary to perform a left thoracotomy. A left pneumonectomy was required after the attempt to reconstruct the anastomosis was ruled out. The conclusion is that great care should be taken when using VATS approach for BC with adhesions.
A cirurgia torácica vídeo-assistida (VATS) é uma abordagem eficaz e viável na ressecção de cistos broncogénicos (BC). As complicações durante a dissecção podem dever-se a aderências pericisticas a estruturas vizinhas. Este artigo descreve um caso pouco comum de uma complicação operatória que consiste na rutura do brônquio principal esquerdo. A abordagem inicial VATS foi convertida a uma toracotomia direita para remover o cisto e proceder a sutura do brônquio uma vez obtida a exposição adequada. A reconstrução bronquial fracassou e algumas horas mais tarde foi necessário realizar a toracotomia esquerda. A pneumonectomia esquerda foi inevitável após a tentativa de reconstruir a anastomose ter sido descartada. Em conclusão, a abordagem VATS para o BC com adesões deve ser realizada/planificada com extremo cuidado.
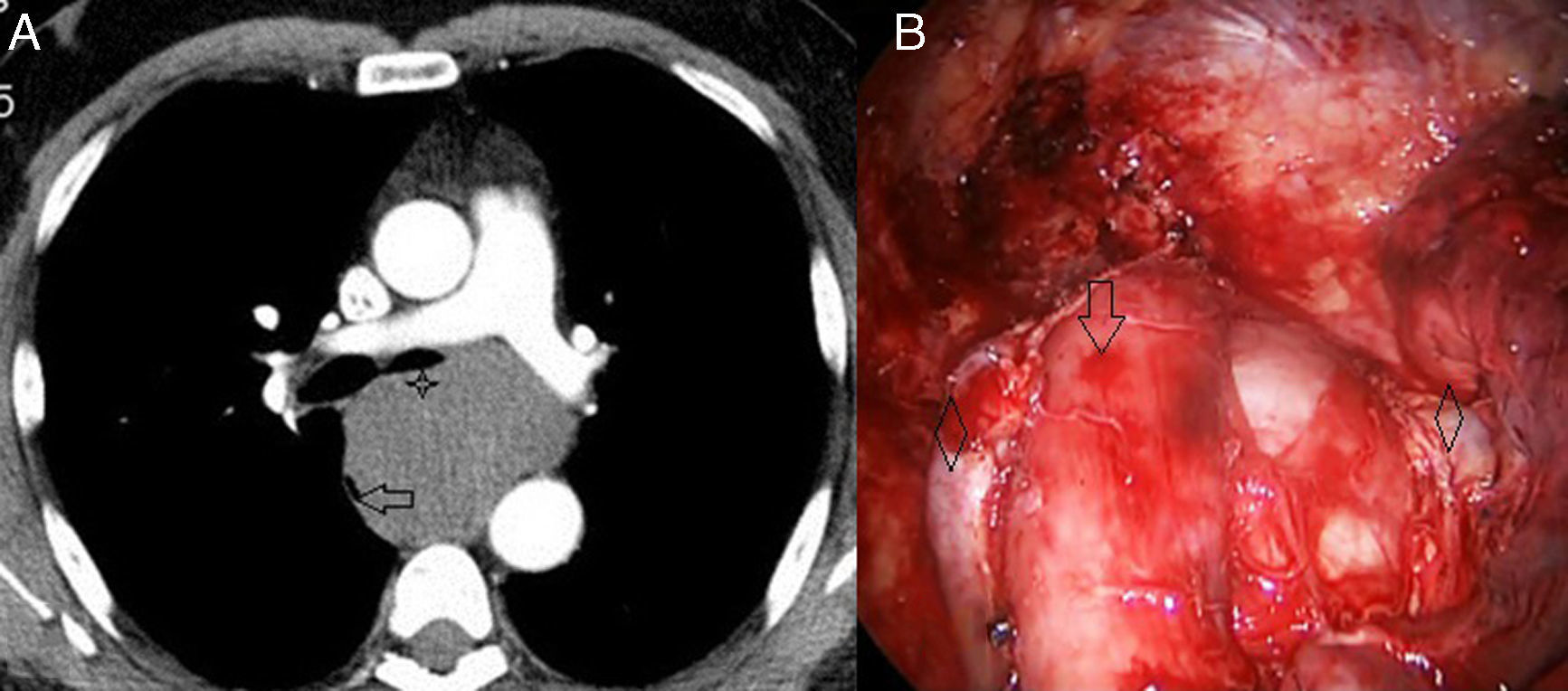
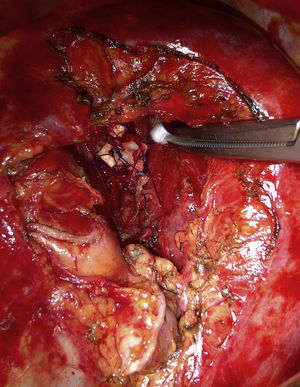
A 42-year-old man with no significant medical history was admitted to our institution, having been referred by his pulmonologist. He presented progressive dyspnea and chest discomfort over the previous three months. Routine chest X-ray showed an enlarged mediastinum. A computed tomography (CT) scan showed a well-circumscribed cyst, of 7cm×5cm×10cm, in the middle and posterior mediastinum, causing the displacement of neighboring structures (Fig. 1A). We performed a magnetic resonance imaging (MRI) which showed a smooth-contoured cystic subcarinal mass with displacement of trachea and main bronchi and reduced caliber of the left main bronchus. Preoperative bronchoscopy excluded any communication between the cyst and the tracheobronchial tree. The patient was considered eligible for surgical treatment by a minimally invasive technique in the right hemithorax. He was intubated with a left-sided double-lumen endotracheal tube (37ch) to obtain one-lung ventilation. We used two port incisions, one in the seventh intercostal space along the posterior axillary line for the camera, and another of 4 cm on the fifth intercostal space along the anterior axillary line. The lung was trapped with pleural adhesions which had to be released in order to expose the lesion. The cystic mass was firmly attached to the adjacent lung parenchyma and chest wall. Once the cystic lesion was exposed, the mediastinal pleura were opened. The azygos vein was sectioned and the esophagus, which had been anteriorly displaced, was separated from the cyst (Fig. 1B). Dissection at the subcarinal level resulted in a sudden, massive air leak. Difficulty in ventilating the patient necessitated conversion to a right thoracotomy. Once the cyst was aspirated and removed, we observed a rupture in the left main bronchus, the wall of which was very thin and had suffered loss of tissue. The rupture extended almost the whole distance from to the carina. We repaired the rupture and the patient was extubated. A fibrobronchoscopy was performed which showed that bronchus reconstruction had been unsuccessful. There was a torsion in the suture with severe stenosis. A few hours later the patient presented hypoxemia and a chest X-ray showed left lung atelectasis. We decided to re-operate through a left thoracotomy to reconstruct the suture. The aortic arch was mobilized and the ductus arteriosus was sectioned to expose the left side of the carina. Despite all our efforts, a safe anastomosis could not be assured so we decided on a left pneumonectomy. The bronchial stump was reinforced with Teflon pledgets (Fig. 2) and the patient recovered uneventfully and was discharged on postoperative day 7.
(A) Computed tomography showing a large bronchogenic cyst located in the subcarinal region narrowing left main bronchus (asterisk) and displacing esophagus (arrow). (B) Intraoperative thoracoscopy image in which we can observe the correlation with the CT image. Anterior displacement of the esophagus is (arrow) and the azygos vein is sectioned (rhombus).
Bronchogenic cysts which are rare in the general population are among the most common cystic lesions of the pediatric mediastinum and lung. The term bronchogenic is applied to all cysts originating from or with physical connection to the bronchial tree. Pathologically, BC are lined by respiratory ciliated columnar or cuboidal epithelium containing mucus glands. The accumulation of mucus results in the gradual enlargement of non-communicating BC.1 Although some BC are asymptomatic and diagnosed as incidental findings on radiographs, most are associated with clinical symptoms such as coughing, dyspnea, chest pain, and sputum.2
Surgery is usually the treatment of choice for BC.3 There is a general consensus on the need for surgery in symptomatic patients, but there is still controversy as to what is the best course in asymptomatic cases.2,4 In recent years, routine surgical procedures have evolved from thoracotomy to a thoracoscopic approach, with excellent results. This would seem to confirm that the appropriate treatment is resection of mediastinal cysts using thoracoscopic procedures.5–7
However, even though in some patients cysts may remain silent forever, once symptoms do arise, it has to be understood that surgery, although advocated, is definitely not an easy option due to the complicating anatomic factors.2 Reports of intraoperative complications during removal of a BC show that these can include bleeding and bronchial rupture.8–10 In our case, the patient presented chest pain and dyspnea and the cyst was associated with severe adhesions to adjacent organs like the esophagus, carina and lung parenchyma. The sharp dissection required led to bronchial damage. This bronchial damage was thought to be related to inflammation due to infection, which generated strong adhesions between the bronchial and cystic wall. The cyst content had not been evacuated prior to removal. Aspiration of mucoidal liquid could have facilitated the exposure and the visualization of the cyst wall at the level of the bronchus rupture. At this stage, a portion of the cyst wall should have been left with ablation of the mucosal lining by electrocautery as reported by Read et al.11
In summary, this report represents an account of a serious complication during the removal of a BC. We would like to emphasize the importance of paying particular attention when resecting mediastinal BC, especially when they are symptomatic and present adhesions.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Peña E, Blanco M, Otero T. Rutura do brônquio principal esquerdo durante a cirurgia torácica video-assistida de um quisto broncogénico. Rev Port Pneumol 2013. http://dx.doi.org/.