The coronavirus disease 2019 (COVID-19) pandemic has shown negative effects on tuberculosis (TB) control. Disruptions to the access to TB services have been reported. In fact, the World Health Organization data show that the pandemic has had a substantial effect on TB trends, with an overall decrease in the number of new TB cases, and an increase in the number of deaths between 2019 and 2020.1
TB and COVID-19 coinfection may be associated with more severe clinical conditions than either disease on its own, leading to greater morbimortality during the acute phase.2–4 Additionally, post-TB lung disease (PTLD) and post-COVID-19 disorders account for substantial consequences on the health of survivors and often require rehabilitation.5,6 Pulmonary impairment after TB is identified in more than 50% of patients, and post-COVID-19 sequelae may affect up to 80% of COVID-19 survivors.5,7 However, the sequelae of TB and COVID-19 co-infected individuals are largely unknown, and there are no studies so far that have evaluated long-term lung function in these patients.
We conducted a prospective cohort study at Hospital de Clínicas de Porto Alegre, Brazil in collaboration with Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) Maugeri, Tradate, Italy. The study was approved by the Ethics Committee of Hospital de Clínicas de Porto Alegre (number 200188). All participants gave their written consent to participation. The study objectives were to assess pulmonary functions tests (PFT, including 6-minute walk test- 6MWT) and quality of life (QoL) in patients with COVID-19 and TB, one year after COVID-19, and to evaluate factors associated with mortality.
Patients ≥18 years of age hospitalized with a concomitant diagnosis of COVID-19 and TB (active or sequelae) were evaluated one year after discharge. Patients underwent PFT: spirometry, plethysmography, diffusing capacity of the lung for carbon monoxide (DLCO), and 6MWT. To assess QoL, the EuroQol-5D scale (EQ-5D) was used. In addition, patients were asked about persistent post-COVID-19 symptoms. Categorical comparisons were performed by chi-square test using Yates's correction if indicated, or Fisher's exact test. Continuous variables were compared using the t-test or Wilcoxon test. A two-sided p value <0.05 was considered significant.
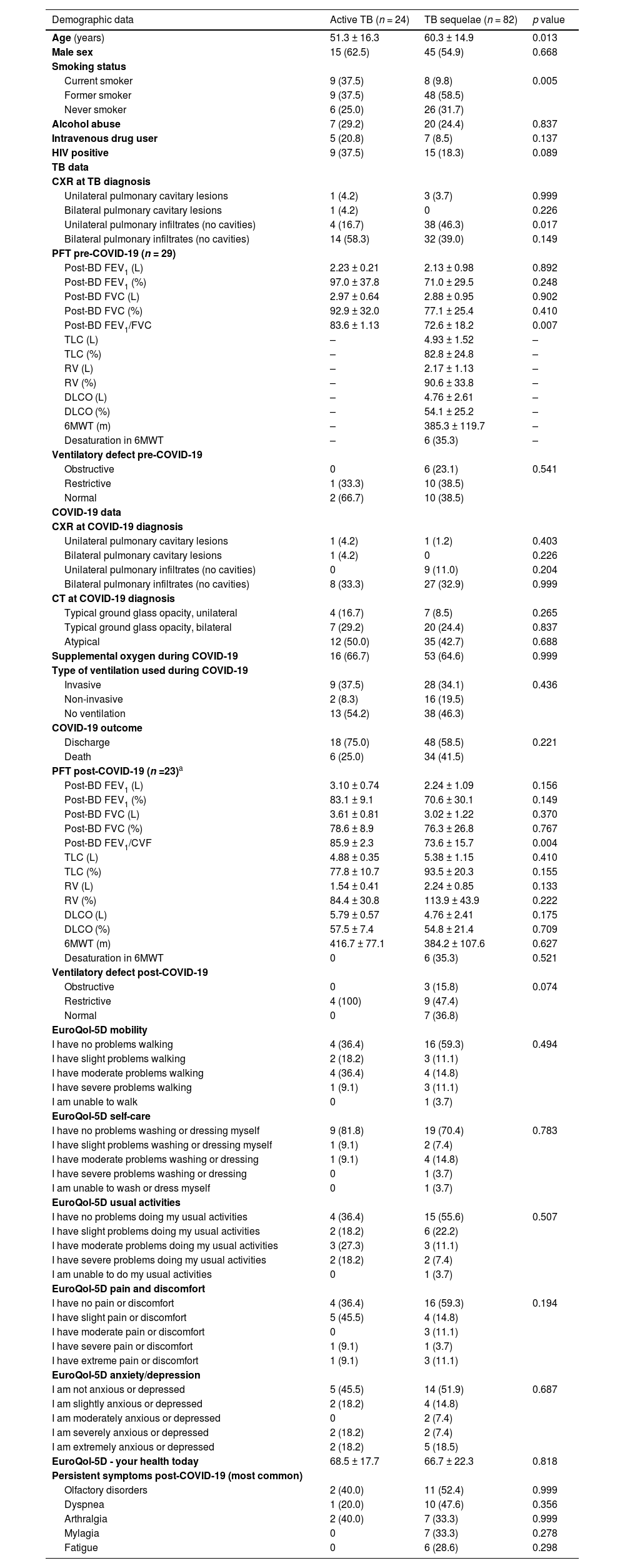
We included 106 patients with COVID-19 and active TB (n = 24) or TB sequelae (n = 82), from March 2020 to December 2022. Forty (37.7%) patients died from COVID-19 during the study period. Of the 66 patients who survived COVID-19, 23 underwent PFT (and 6MWT), and were assessed for QoL and persistence of symptoms. Table 1 shows the cohort characteristics. The most common post-COVID-19 ventilatory impairment was restrictive. A large percentage of patients had impaired QoL in the usual activities, anxiety/depression, mobility and pain/discomfort dimensions. All patients reported at least one persistent post-COVID-19 symptom. Active TB patients were younger and had a higher prevalence of current smoking.
General characteristics of patients.
| Demographic data | Active TB (n = 24) | TB sequelae (n = 82) | p value |
|---|---|---|---|
| Age (years) | 51.3 ± 16.3 | 60.3 ± 14.9 | 0.013 |
| Male sex | 15 (62.5) | 45 (54.9) | 0.668 |
| Smoking status | |||
| Current smoker | 9 (37.5) | 8 (9.8) | 0.005 |
| Former smoker | 9 (37.5) | 48 (58.5) | |
| Never smoker | 6 (25.0) | 26 (31.7) | |
| Alcohol abuse | 7 (29.2) | 20 (24.4) | 0.837 |
| Intravenous drug user | 5 (20.8) | 7 (8.5) | 0.137 |
| HIV positive | 9 (37.5) | 15 (18.3) | 0.089 |
| TB data | |||
| CXR at TB diagnosis | |||
| Unilateral pulmonary cavitary lesions | 1 (4.2) | 3 (3.7) | 0.999 |
| Bilateral pulmonary cavitary lesions | 1 (4.2) | 0 | 0.226 |
| Unilateral pulmonary infiltrates (no cavities) | 4 (16.7) | 38 (46.3) | 0.017 |
| Bilateral pulmonary infiltrates (no cavities) | 14 (58.3) | 32 (39.0) | 0.149 |
| PFT pre-COVID-19 (n = 29) | |||
| Post-BD FEV1 (L) | 2.23 ± 0.21 | 2.13 ± 0.98 | 0.892 |
| Post-BD FEV1 (%) | 97.0 ± 37.8 | 71.0 ± 29.5 | 0.248 |
| Post-BD FVC (L) | 2.97 ± 0.64 | 2.88 ± 0.95 | 0.902 |
| Post-BD FVC (%) | 92.9 ± 32.0 | 77.1 ± 25.4 | 0.410 |
| Post-BD FEV1/FVC | 83.6 ± 1.13 | 72.6 ± 18.2 | 0.007 |
| TLC (L) | – | 4.93 ± 1.52 | – |
| TLC (%) | – | 82.8 ± 24.8 | – |
| RV (L) | – | 2.17 ± 1.13 | – |
| RV (%) | – | 90.6 ± 33.8 | – |
| DLCO (L) | – | 4.76 ± 2.61 | – |
| DLCO (%) | – | 54.1 ± 25.2 | – |
| 6MWT (m) | – | 385.3 ± 119.7 | – |
| Desaturation in 6MWT | – | 6 (35.3) | – |
| Ventilatory defect pre-COVID-19 | |||
| Obstructive | 0 | 6 (23.1) | 0.541 |
| Restrictive | 1 (33.3) | 10 (38.5) | |
| Normal | 2 (66.7) | 10 (38.5) | |
| COVID-19 data | |||
| CXR at COVID-19 diagnosis | |||
| Unilateral pulmonary cavitary lesions | 1 (4.2) | 1 (1.2) | 0.403 |
| Bilateral pulmonary cavitary lesions | 1 (4.2) | 0 | 0.226 |
| Unilateral pulmonary infiltrates (no cavities) | 0 | 9 (11.0) | 0.204 |
| Bilateral pulmonary infiltrates (no cavities) | 8 (33.3) | 27 (32.9) | 0.999 |
| CT at COVID-19 diagnosis | |||
| Typical ground glass opacity, unilateral | 4 (16.7) | 7 (8.5) | 0.265 |
| Typical ground glass opacity, bilateral | 7 (29.2) | 20 (24.4) | 0.837 |
| Atypical | 12 (50.0) | 35 (42.7) | 0.688 |
| Supplemental oxygen during COVID-19 | 16 (66.7) | 53 (64.6) | 0.999 |
| Type of ventilation used during COVID-19 | |||
| Invasive | 9 (37.5) | 28 (34.1) | 0.436 |
| Non-invasive | 2 (8.3) | 16 (19.5) | |
| No ventilation | 13 (54.2) | 38 (46.3) | |
| COVID-19 outcome | |||
| Discharge | 18 (75.0) | 48 (58.5) | 0.221 |
| Death | 6 (25.0) | 34 (41.5) | |
| PFT post-COVID-19 (n =23)a | |||
| Post-BD FEV1 (L) | 3.10 ± 0.74 | 2.24 ± 1.09 | 0.156 |
| Post-BD FEV1 (%) | 83.1 ± 9.1 | 70.6 ± 30.1 | 0.149 |
| Post-BD FVC (L) | 3.61 ± 0.81 | 3.02 ± 1.22 | 0.370 |
| Post-BD FVC (%) | 78.6 ± 8.9 | 76.3 ± 26.8 | 0.767 |
| Post-BD FEV1/CVF | 85.9 ± 2.3 | 73.6 ± 15.7 | 0.004 |
| TLC (L) | 4.88 ± 0.35 | 5.38 ± 1.15 | 0.410 |
| TLC (%) | 77.8 ± 10.7 | 93.5 ± 20.3 | 0.155 |
| RV (L) | 1.54 ± 0.41 | 2.24 ± 0.85 | 0.133 |
| RV (%) | 84.4 ± 30.8 | 113.9 ± 43.9 | 0.222 |
| DLCO (L) | 5.79 ± 0.57 | 4.76 ± 2.41 | 0.175 |
| DLCO (%) | 57.5 ± 7.4 | 54.8 ± 21.4 | 0.709 |
| 6MWT (m) | 416.7 ± 77.1 | 384.2 ± 107.6 | 0.627 |
| Desaturation in 6MWT | 0 | 6 (35.3) | 0.521 |
| Ventilatory defect post-COVID-19 | |||
| Obstructive | 0 | 3 (15.8) | 0.074 |
| Restrictive | 4 (100) | 9 (47.4) | |
| Normal | 0 | 7 (36.8) | |
| EuroQol-5D mobility | |||
| I have no problems walking | 4 (36.4) | 16 (59.3) | 0.494 |
| I have slight problems walking | 2 (18.2) | 3 (11.1) | |
| I have moderate problems walking | 4 (36.4) | 4 (14.8) | |
| I have severe problems walking | 1 (9.1) | 3 (11.1) | |
| I am unable to walk | 0 | 1 (3.7) | |
| EuroQol-5D self-care | |||
| I have no problems washing or dressing myself | 9 (81.8) | 19 (70.4) | 0.783 |
| I have slight problems washing or dressing myself | 1 (9.1) | 2 (7.4) | |
| I have moderate problems washing or dressing | 1 (9.1) | 4 (14.8) | |
| I have severe problems washing or dressing | 0 | 1 (3.7) | |
| I am unable to wash or dress myself | 0 | 1 (3.7) | |
| EuroQol-5D usual activities | |||
| I have no problems doing my usual activities | 4 (36.4) | 15 (55.6) | 0.507 |
| I have slight problems doing my usual activities | 2 (18.2) | 6 (22.2) | |
| I have moderate problems doing my usual activities | 3 (27.3) | 3 (11.1) | |
| I have severe problems doing my usual activities | 2 (18.2) | 2 (7.4) | |
| I am unable to do my usual activities | 0 | 1 (3.7) | |
| EuroQol-5D pain and discomfort | |||
| I have no pain or discomfort | 4 (36.4) | 16 (59.3) | 0.194 |
| I have slight pain or discomfort | 5 (45.5) | 4 (14.8) | |
| I have moderate pain or discomfort | 0 | 3 (11.1) | |
| I have severe pain or discomfort | 1 (9.1) | 1 (3.7) | |
| I have extreme pain or discomfort | 1 (9.1) | 3 (11.1) | |
| EuroQol-5D anxiety/depression | |||
| I am not anxious or depressed | 5 (45.5) | 14 (51.9) | 0.687 |
| I am slightly anxious or depressed | 2 (18.2) | 4 (14.8) | |
| I am moderately anxious or depressed | 0 | 2 (7.4) | |
| I am severely anxious or depressed | 2 (18.2) | 2 (7.4) | |
| I am extremely anxious or depressed | 2 (18.2) | 5 (18.5) | |
| EuroQol-5D - your health today | 68.5 ± 17.7 | 66.7 ± 22.3 | 0.818 |
| Persistent symptoms post-COVID-19 (most common) | |||
| Olfactory disorders | 2 (40.0) | 11 (52.4) | 0.999 |
| Dyspnea | 1 (20.0) | 10 (47.6) | 0.356 |
| Arthralgia | 2 (40.0) | 7 (33.3) | 0.999 |
| Mylagia | 0 | 7 (33.3) | 0.278 |
| Fatigue | 0 | 6 (28.6) | 0.298 |
Ten patients had PFT pre- and post-COVID-19. There was a reduction in all lung function parameters, but not statistically significant (p > 0.05 for all comparisons; data not shown). The 6MWT final test was in average 39.4 m lower than the initial test (although not significant, patients lost about 10% of the performance).
Table 2 shows the factors associated with mortality. TB sequelae patients who were older, needed supplemental oxygen and invasive ventilation, and those who had lower total lung capacity (TLC) (%) and DLCO (%) had higher mortality. Active TB patients who needed invasive ventilation had higher mortality.
Factors associated with mortality in TB-COVID-19 patients.
| Demographic data | Active TB | p value | TB Sequelae | p value | ||
|---|---|---|---|---|---|---|
| Survivors(n = 18) | Non-survivorsa(n = 6) | Survivors(n = 48) | Non-survivorsa(n = 34) | |||
| Age (years) | 49.6 ± 13.9 | 56.3 ± 22.9 | 0.393 | 55.1 ± 15.4 | 67.5 ± 10.9 | <0.0001 |
| Male sex | 11 (61.1) | 4 (66.7) | 0.999 | 24 (50.0) | 21 (61.8) | 0.407 |
| Smoking status | ||||||
| Current smoker | 8 (44.4) | 1 (16.7) | 0.230 | 4 (8.3) | 4 (11.8) | 0.189 |
| Former smoker | 5 (27.8) | 4 (66.7) | 25 (52.1) | 23 (67.6) | ||
| Never smoker | 5 (27.8) | 1 (16.7) | 19 (39.6) | 7 (20.6) | ||
| Alcohol abuse | 5 (27.8) | 2 (33.3) | 0.999 | 12 (25.0) | 8 (23.5) | 0.999 |
| Intravenous drug user | 3 (16.7) | 2 (33.3) | 0.568 | 4 (8.3) | 3 (8.8) | 0.999 |
| HIV positive | 7 (38.9) | 2 (33.3) | 0.999 | 7 (14.6) | 8 (23.5) | 0.458 |
| TB data | ||||||
| PFT pre-COVID-19 | ||||||
| Post-BD FEV1 (L) | 2.23 ± 0.21 | – | – | 2.29 ± 1.09 | 1.91 ± 0.84 | 0.358 |
| Post-BD FEV1 (%) | 97.0 ± 37.8 | – | – | 75.2 ± 30.8 | 65.7 ± 28.4 | 0.436 |
| Post-BD FVC (L) | 2.97 ± 0.64 | – | – | 3.04 ± 0.96 | 2.69 ± 0.94 | 0.373 |
| Post-BD FVC (%) | 92.9 ± 32.0 | – | – | 80.9 ± 26.4 | 72.2 ± 24.4 | 0.398 |
| Post-BD FEV1/FVC | 83.6 ± 1.1 | – | – | 75.3 ± 19.6 | 69.2 ± 16.4 | 0.418 |
| TLC (L) | – | – | – | 5.57 ± 1.49 | 4.39 ± 1.43 | 0.179 |
| TLC (%) | – | – | – | 99.1 ± 25.1 | 68.9 ± 14.6 | 0.020 |
| RV (L) | – | – | – | 2.55 ± 1.42 | 1.84 ± 0.76 | 0.279 |
| RV (%) | – | – | – | 94.4 ± 35.0 | 86.9 ± 35.5 | 0.721 |
| DLCO (L) | – | – | – | 5.50 ± 3.08 | 4.12 ± 2.12 | 0.325 |
| DLCO (%) | – | – | – | 68.4 ± 21.5 | 41.7 ± 22.2 | 0.035 |
| 6MWT (m) | – | – | – | 394.1 ± 131.4 | 377.4 ± 115.8 | 0.786 |
| Desaturation in 6MWT | – | – | – | |||
| Ventilatory defect post-TB | ||||||
| Obstructive | – | – | – | 4 (28.6) | 2 (16.7) | 0.148 |
| Restrictive | – | – | 3 (21.4) | 7 (58.3) | ||
| Normal | 2 (66.7) | – | 7 (50.0) | 3 (25.0) | ||
| COVID-19 data | ||||||
| CXR at COVID-19 diagnosis | ||||||
| Unilateral pulmonary cavitary lesions | 0 | 1 (16.7) | 0.250 | 1 (2.1) | 0 | 0.999 |
| Bilateral pulmonary cavitary lesions | 0 | 1 (16.7) | 0.250 | – | – | – |
| Unilateral pulmonary infiltrates (no cavities) | – | – | – | 5 (10.4) | 4 (11.8) | 0.999 |
| Bilateral pulmonary infiltrates (no cavities) | 4 (22.2) | 4 (66.7) | 0.129 | 17 (35.4) | 10 (29.4) | 0.740 |
| CT at COVID-19 diagnosis | ||||||
| Typical ground glass opacity, unilateral | 4 (22.2) | 0 | 0.539 | 3 (6.3) | 4 (11.8) | 0.441 |
| Typical ground glass opacity, bilateral | 4 (22.2) | 3 (50.0) | 0.307 | 12 (25.0) | 8 (23.5) | 0.999 |
| Atypical | 10 (55.6) | 2 (33.3) | 0.640 | 18 (37.5) | 17 (50.0) | 0.368 |
| Supplemental oxygen during COVID-19 | 10 (55.6) | 6 (100) | 0.066 | 22 (45.8) | 31 (91.2) | <0.0001 |
| Type of ventilation used during COVID-19 | ||||||
| Invasive | 4 (22.2) | 5 (83.3) | 0.003 | 8 (16.7) | 20 (58.8) | <0.0001 |
| Non-invasive | 1 (5.6) | 1 (16.7) | 6 (12.5) | 10 (29.4) | ||
| No ventilation | 13 (72.2) | 0 | 34 (70.8) | 4 (11.8) | ||
Median time do death: Active TB group (13 days [5–27.8 days]) and TB sequelae group (15.5 days [6.8–29.3 days], p = 0.691.
In this prospective cohort study, we demonstrated that, one year after COVID-19, patients with TB and COVID-19 had abnormal PFT, reduced 6MWT performances, impaired QoL, and persistent symptoms. Furthermore, the mortality of these patients was high (almost 40%).
In the largest cohort of patients with TB and COVID-19,2 mortality was 11%, and the factors associated with death were older age, male gender and invasive ventilation. In a previous study,3 the case fatality rate was 12.3% and deaths were mostly in patients >60 years, with at least one comorbidity. Older age and invasive ventilation were also risk factors for mortality in the present study. However, we identified a higher mortality, probably because we included only hospitalized patients.
Patients with TB sequelae and COVID-19 who died had lower TLC (%) and DLCO (%) pre-COVID-19, emphasizing the mortality related to PTLD. In fact, PTLD patients have twice the risk of spirometry abnormalities than the general population, and patients surviving COVID-19 may have persistent abnormalities in PFT, such as restrictive ventilatory defects and diffusion impairment.5 In the present study, a large percentage of patients had restrictive ventilatory pattern, although part of this may be due to sequelae from TB. Although not significant, the loss in 6MWT performances in the final test (about 10%) was relevant.
This study has some limitations. We did not evaluate COVID-19 radiological sequelae, nor pre-COVID-19 QoL. The relatively small sample size of patients with pre- and post-COVID-19 PFT (several patients had severe clinical conditions contraindicating PFT) may have prevented us from finding statistically significant differences.
In conclusion, this study describes the combination of PTLD and post-COVID-19 sequelae, evaluated through PFT (including 6MWT) and QoL. Further studies should evaluate comprehensive strategies to assessment/follow-up and determine the need for pulmonary rehabilitation to improve lung health of patients with these two diseases overlapping.