Lung cancer (LC) is the leading cause of cancer mortality in Portugal and although more frequent in male and older patients (pts), 0.6–13% of LC diagnosis occur in young pts.1 The definition of young patient is not clear, varying between less than 35 years to less than 50 years.1,2 Several studies have been published regarding LC in young pts, suggesting an increased percentage of female1–4 and non-smokers pts,1,5 a longer duration of symptoms,5 a higher frequency of adenocarcinoma1–5 rather than squamous cell carcinoma and a higher frequency of advanced disease at diagnosis.2,4,6 It is still controversial whether younger pts have similar,6 better1–4 or worse5 outcomes than older pts and recent studies have suggested that young pts with non-small cell lung carcinoma (NSCLC) harbor more driver mutations than older pts.7
In order to understand whether or not LC in younger pts is a genetically unique disease with a particular natural history, biology and prognosis, we retrospectively performed a comprehensive and comparative analysis of younger versus older LC pts diagnosed in our institution from January 2014 to April 2020. Patients were included in the young cohort if their age at diagnosis was greater than two standard deviations less than median age at diagnosis,2 which in our study meant pts aged 42 years or younger. Patients´ clinical and pathological features and clinical outcomes were evaluated. Categorical characteristics were compared using the Chi-square test and continuous variables were compared using the Kaplan- Meier method. A p value less than 0.05 was considered significant.
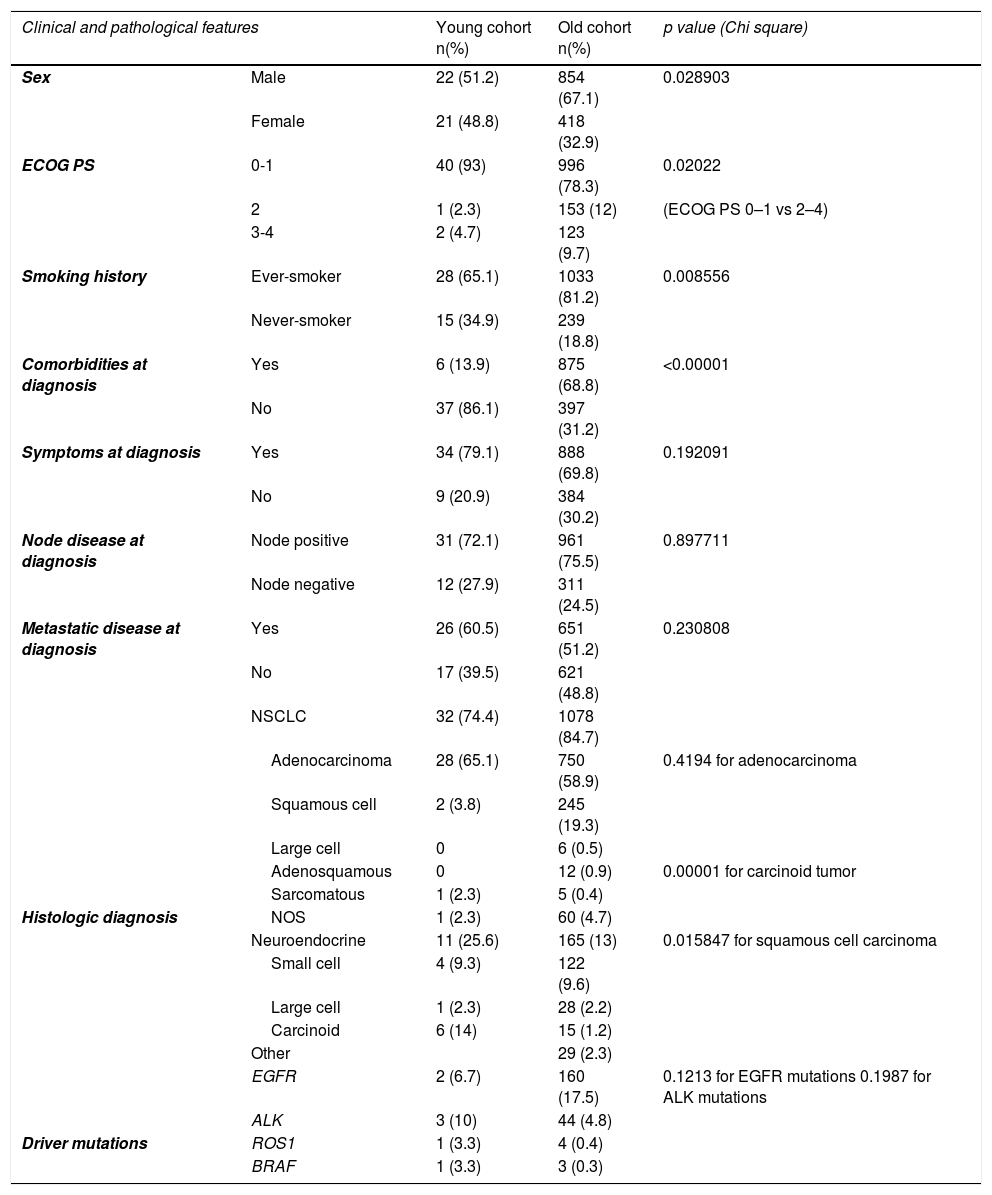
We identified 1315 pts with LC: 43 (3.3%) pts were included in the young cohort (median age at diagnosis was 37.9 years, 29–42) and 1272 (96.7%) pts were included in the old cohort (median age at diagnosis was 65.8 years, 43–95). Younger pts were more likely to be female, have an Eastern Cooperative Oncology Group performance status of 0–1, have fewer comorbidities at diagnosis and to be never-smokers, than older patients. Similar rates of symptomatic disease, node positive disease and metastatic disease were seen in both cohorts (Table 1).
Clinical and pathological features of LC pts in the young versus old cohorts.
Lung cancer in the young versus old cohorts was equally likely to be adenocarcinoma, more likely to be carcinoid tumor and less likely to be squamous cell carcinoma. The frequency of EGFR and ALK variants was similar in both cohorts. Median follow-up time was longer in the young cohort (16.6 months versus 13.4 months, p = 0.123). There were 46.5% versus 53.8% deaths registered in the young and old cohorts, respectively. Median overall survival (OS) was better in the young cohort, but the difference was not significant (9.2 months versus 8.4 months; p = 0.166). No deaths were documented in clinical stages I and II in the young cohort. Median OS was better in younger pts with clinical stages I, II and IV LC and worse in younger pts with clinical stage III LC, but differences were not significant (p = 0.245; p = 0.332; p = 0.088; p = 0.459, respectively).
Our findings are consistent with previous studies suggesting that younger pts with LC are more likely to be female,1–4 fitter,2 healthier1,2 and never-smokers.1–5 Adenocarcinoma was the most common histopathology in both age groups but unlike other reports,1–5 an increased likelihood of adenocarcinoma in younger pts was not found. We also report a lower incidence of driver mutations in comparison to previous studies7 and an increased rate of EGFR and ALK variants in younger pts was not found. Moreover, we reported a non-significant improved outcome in younger pts and median OS in both younger and older pts was inferior in comparison to previous studies. Our study was not, however, restricted to NSCLC as most previous studies were and that may explain the differences found. The small number of younger pts may also explain survival differences. Prospective multicentre studies are needed.