The importance of a thorough knowledge of thoracic anatomy is timeless. Lung and pleural anatomy continues to be a subject for study nowadays, not only due to the greater spatial resolution of newer diagnostic studies, such as bronchoscopy, computed tomography and magnetic resonance, but also because of advances in thoracic surgery.
The pulmonary ligaments are among the lesser known structures of the thoracic anatomy. The radiological importance of the pulmonary ligament was first described in 1966 by Rabinowitz and Wolfe,1 and only very few reports or series have been found which describe the radiological findings of pathologic processes within the pulmonary ligaments.1–6 This ligament, just like any other thoracic anatomical structure can be affected by non-infectious or infectious inflammatory processes, tumors, congenital or developmental abnormalities and scarring.2–6 There are only a few reports in the literature which mention this anatomical structure and different pathological process.
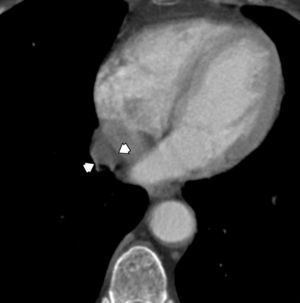
The following case description of a cystic lesion within the right pulmonary ligament illustrates the anatomy and pathology of this structure:
A 75-year-old woman diagnosed with a pharyngeal cancer was referred for magnetic resonance imaging of the neck and a computed tomography (CT) of the chest and upper abdomen. The enhanced CT chest demonstrated an incidental tubular cystic lesion, oriented parallel to the mediastinum, within the right pulmonary ligament, extending from the level just caudal to the right inferior pulmonary vein down to the diaphragm. This lesion measured 5.5cm×2.7cm×1.8cm and showed homogeneous density, mean attenuation value=−3.92Hounsfield Units (HU). This lesion was separated from pericardium by a layer of fat. The lesion was followed up and remained stable in size and shape for 4 years, as per the comparison with a previous CT scan. The appearance on axial, coronal and sagittal planes confirmed that the cyst was within the pulmonary ligament (Figs. 1 and 2). The cystic lesion also had no depression of the hilar structures or elevation or blurring of the diaphragm. So the non-symptomatic clinical setting alongside with the anatomical landmarks described and the lack of change in size/configuration during these years supported the diagnosis of a mesothelial cyst of the pulmonary ligament.
This case under discussion provides a very good illustration of the anatomical concepts that define the pulmonary ligament as double layer of pleura that drapes caudally from the lung root and ropes the medial aspect of the lower lobes of the lung to the mediastinum.2 On the left, the ligament is medial and adjacent to the esophagus and is bounded posteriorly by the descending aorta. On the right, the ligament is posterior to the inferior vena cava and anterior to the azygos vein.2–4 Each ligament contains connective tissue which blends with the hilar connective tissue superiorly, and with mediastinal connective tissue medially. Laterally, the connective tissue of the ligaments is continuous with the interstitial connective tissue of the lung.2–4
On CT scans normal ligament can be visible as a thin linear density arising from the mediastinum below the hilar structures on lung window.3
Few reports in the literature have described air within the pulmonary ligament, post-traumatic or from ruptured pneumatoceles in neonates under mechanical ventilation.4–6 Moreover, around 11–18% of mediastinal masses are related to the foregut developmental abnormalities, including bronchogenic or duplication cysts. The phase of the embryonic development during which the error occurs seems to play a role in the location and type of malformation. Foregut cysts arise late in the gestation. The age of presentation may vary from prenatal to late adulthood. Almost a quarter of the patients with foregut cysts are asymptomatic.7 The presented clinical case therefore illustrates a rare but typical cystic lesion, probable arising from developmental error within the pulmonary ligament.
FundingAll authors declare that no funding was provided for this case report.
Conflicts of interestThe authors have no conflicts of interest to declare.