Children may benefit from minimally invasive surgery (MIS) in the correction of Morgagni hernia (MH). The present study aims to evaluate the outcome of MIS through a multicenter study.
National institutions that use MIS in the treatment of MH were included. Demographic, clinical and operative data were analyzed.
Thirteen patients with MH (6 males) were operated using similar MIS technique (percutaneous stitches) at a mean age of 22.2±18.3 months. Six patients had chromosomopathies (46%), five with Down syndrome (39%). Respiratory complaints were the most common presentation (54%). Surgery lasted 95±23min. In none of the patients was the hernia sac removed; prosthesis was never used. In the immediate post-operative period, 4 patients (36%) were admitted to intensive care unit (all with Down syndrome); all patients started enteral feeds within the first 24h. With a mean follow-up of 56±16.6 months, there were two recurrences (18%) at the same institution, one of which was repaired with an absorbable suture; both with Down syndrome.
The application of MIS in the MH repair is effective even in the presence of comorbidities such as Down syndrome; the latter influences the immediate postoperative recovery and possibly the recurrence rate. Removal of hernia sac does not seem necessary. Non-absorbable sutures may be more appropriate.
The Morgagni foramen was first described by the Italian anatomist Giovanni Morgagni in 1769.1 This defect located in the anteromedial portion of the diaphragm, between the xiphisternal and costal margin fibers, results from a failure in the fusion of the septum transversum and the costal arches.2 Its presence may allow the passage of abdominal contents, including the omentum, stomach, colon, liver or small bowel into the thoracic cavity, thus resulting in Morgagni hernia (MH).3,4 MH is extremely rare, occurring approximately in 1 out of 4800 live births, and accounts for less than 6% of all congenital diaphragmatic defects repaired in pediatric age group.5 Associated congenital malformation such as congenital heart disease, chest wall deformities, intestinal malrotation or omphalocele has been reported. Chromosomal anomalies, mainly Down syndrome (DS), are frequent findings.2,6 MH is typically asymptomatic and may present with nonspecific respiratory symptoms, often discovered later in life.2,7
The present study aims to assess and evaluate the surgical and clinical outcomes in the mid-term follow-up of children submitted to MIS in the correction of the MH, through a national multicentric study.
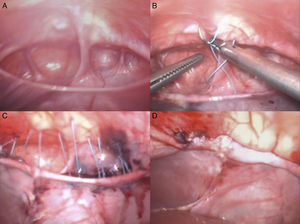
Material and methodsAll national institutions that use MIS in the treatment of MH in children were included in a retrospective transversal study. Clinical files from all patients operated on from December 2006 to June 2013 were reviewed and analyzed by members of each institution. Patients were included when submitted to laparoscopic-assisted surgical approach using three ports and when sutures were performed with, separated, percutaneous, “U” shaped, stitches, through the full thickness of the anterior abdominal wall (Fig. 1) and the knots were tied in the subcutaneous tissue, by separated minor skin incisions or by a single incision. Patients submitted to laparotomy, thoracotomy or any other minimal invasive technique different than that described were excluded. Collected data included age, gender, clinical presentation, associated malformations, surgical details, length of hospital stay, post-operative admission to intensive care unit, time of start of enteral feeds, complications and follow-up details (clinical, radiological).
ResultsDuring the study period, 13 patients (six males and seven females) were diagnosed with MH and submitted to correction at four different tertiary centers. Demographic data is presented in Table 1. Six patients had chromosomopathies (46%) including five children with Down syndrome (39%). The most common presentation was respiratory symptoms (54%), followed by incidental finding (23%). Five patients (39%) had previous admissions for different causes. Diagnosis was reached by chest roentgenogram, contrast enema or computed tomographic scan.
Demographics and clinical presentation. CXR – plain chest roentgenogram; CT – computed tomography.
| Case | Gender | Clinical presentation | Previous admissions | Age at diagnosis (months) | Chromosomopathy | Diagnosis |
|---|---|---|---|---|---|---|
| 1 | F | Pneumonia | Yes | 7 | No | CT |
| 2 | F | Persistent coughing | No | 5 | No | CXR |
| 3 | M | Bronchiolitis | Yes | 4 | Down syndrome | CXR, CT |
| 4 | F | Bronchiolitis | No | 14 | No | CXR, CT |
| 5 | M | Fever | No | 9 | No | CXR, CT |
| 6 | F | Incidental during echocardiogram | Yes | 55 | Down syndrome | CXR, CT |
| 7 | M | Incidental during echocardiogram | Yes | 17 | Down syndrome | CXR CT |
| 8 | M | Incidental, after foreign body ingestion | Yes | 48 | Down syndrome | CXR, CT |
| 9 | F | Nonspecific respiratory symptoms | – | 22 | 46,XX, del(4) | CXR |
| 10 | M | Bronchiolitis | Yes | 18 | No | CXR, CT |
| 11 | F | Asymmetric chest wall deformity | No | 16 | No | CXR, CT contrast enema |
| 12 | F | – | – | 19 | No | Rx |
| 13 | M | Bronchiolitis | Yes | 14 | Down syndrome | CXR, contrast enema |
In all cases, the correction was initially performed using identical laparoscopic-assisted technique with full thickness separated percutaneous stitches. Surgical details are expressed in Table 2. Children were operated on at a mean age of 22±18.3 months. The mean operative time was 95±23min. There were no intra-operative complications and no need for conversion. In none of the patients was the hernia sac removed, and prosthetic patch was never used. In the immediate post-operative period, 4 patients (36%) were admitted to intensive care unit, all of them with Down syndrome (p<0.05). All patients started enteral feeding within the first 24h.
Perioperative and follow-up details. CXR – plain chest roentgenogram; ICU – intensive care unit.
| Case | Age at surgery (months) | Laterality | Hernia contents | Suture | Associated procedures | Operative time (min) | Need for ICU | Length of hospital stay (days) | Residual cavity (CXR) | Recurrence | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 8 | Left | Small bowel | Nonabsorbable | No | 60 | No | 1 | No | No | 62 |
| 2 | 6 | Bilateral | Liver, Small bowel | Nonabsorbable | No | 95 | No | 2 | No | No | 42 |
| 3 | 4 | Bilateral | Colon | Nonabsorbable | Inguinal hernia repair | 105 | Yes | 16 | No | No | 36 |
| 4 | 16 | Right | Small bowel, Colon | Absorbable | No | 90 | No | 3 | No | No | 49 |
| 5 | 9 | Bilateral | – | Nonabsorbable | No | 40 | No | 1 | No | No | 60 |
| 6 | 61 | Bilateral | Liver, Colon, Omentum | Nonabsorbable | No | 110 | Yes | 3 | – | Yes | 34 |
| 7 | 17 | Bilateral | Colon | Absorbable | Orchidopexy | 115 | Yes | – | – | Yes | 30 |
| 8 | 58 | Bilateral | Colon | Nonabsorbable | Adenoidectomy Myringotomy | 120 | Yes | 7 | No | No | 59 |
| 9 | 23 | Bilateral | – | Nonabsorbable | No | 120 | No | 2 | No | No | 46 |
| 10 | 23 | Bilateral | Small bowel | Nonabsorbable | No | 90 | No | 3 | No | No | 24 |
| 11 | 17 | Bilateral | Colon | Nonabsorbable | No | 105 | No | 3 | No | No | 17 |
| 12 | 33 | – | – | – | – | 105 | No | 3 | No | No | 51 |
| 13 | 14 | Bilateral | Liver | Nonabsorbable | Orchidopexy Myringotomy | 90 | No | 3 | No | No | 9 |
With a mean follow-up of 56±16.6 months, there were two recurrences (18%) at the same institution. One of the recurrences was a case in which an absorbable suture was used and both had Down syndrome, but these findings were not significantly associated with recurrence (p=0.15 and p=0.13 respectively)
DiscussionSurgical repair of MH, with reduction of hernia contents and primary closure of the defect, is generally indicated in order to prevent potential major intestinal complications such as, obstruction, volvulus or perforation. Although some authors advocate transthoracic surgery arguing for a better exposure and better visualization of the phrenic nerve and safer sac resection, the majority of pediatric surgeons prefer transabdominal approach. For many years, thoracotomy and specially laparotomy have been the standard surgical approaches. After the first laparoscopic repair of MH by Kuster et al.20 in 1992, minimally invasive techniques, including single-port approach and robotic surgery, became rapidly accepted as elected approaches in the repair of MH in both children and adults.7,16,21–23 Many technical aspects are still under debate. The laparoscopic reduction of the hernia contents does not appear to be a problem, but the method for closure of the defect is variable and may be technically demanding when performed exclusively by laparoscopy. Some authors recommend the laparoscopic-assisted repair of Morgagni hernia with extracorporeal knots under the subcutaneous tissue.5,8–10 It includes the full thickness of the anterior abdominal wall in U-shaped stitches under direct vision, so that the suture becomes solid, allowing for maximum strength repair. By contrast, anchoring the sutures in the back of the sternum and costal margin is technically challenging and the fascia may not be strong enough. Regarding the choice of suture line, as our series corroborate, the use of absorbable suture may be associated with recurrence.24–26
Another controversial issue is whether or not to excise the hernia sac. Excision is suggested in order to reduce recurrence rate, but it may be laborious and potentially dangerous.10,12–15 As advocated by others, in our series the sac was only plicated, thus avoiding any possible injury of the pericardium, pleura, or phrenic nerve that might be associated with the hernia sac excision. Simultaneously, a low recurrence rate was observed.
The literature records of series of MH submitted to minimal invasive repair are scarce with small sample size and short-term follow-up. The current multicenter series is one of the largest with the longest reported follow-up (25–78 months) and we have found a 15% (2/13) recurrence rate. The remaining 85% of patients show complete obliteration of the residual cavity in chest roentgenogram, as previously described.27,28
In large Bochdalek congenital diaphragmatic hernias, the use of a prosthetic patch is frequently advocated. In MH repair, the use of patch is more controversial. In a previous series, it has been hypothesized that tension closure could be the cause of a high recurrence rate and the use of a patch was suggested in order to reduce tension of repair and decreased recurrence rate.11,26,29 Our series have contradicting results as we report a series without the use of patch and with a low recurrence rate.
The association with chromosomal disorders and congenital anomalies such as congenital heart disease, chest wall deformities, intestinal malrotation, omphalocele, trisomy 21, pentalogy of Cantrell, Noonan syndrome, Prader–Willi syndrome and Turner syndrome is well established.2,6 In our series, six patients (46%) had chromosomopathies and another one presented a chest wall deformity. As in earlier reports, Down syndrome was a frequent association (38%)18,19; all the patients in whom recurrence occurred, also had Down syndrome. This chromosomopathy has been previously associated with impaired healing, and there might be an association with recurrence, although it was not statistically significant in our study. Additionally admissions to intensive care units were significantly more frequent in patients with this syndrome, probably due to other co-morbidities.18,19
In conclusion, laparoscopic-assisted repair of Morgagni hernia using sutures including the full thickness of anterior abdominal wall and extracorporeal knots proved to be effective, safe, and reliable in children, even in the presence of comorbidities such as Down syndrome; the latter seems to influence the immediate postoperative recovery and possibly the recurrence rate. Our series corroborates that there is no need for hernia sac excision or the use of prosthetic patch; absorbable sutures are not recommended. Further prospective randomized trials are needed to confirm and compare these favorable outcomes of laparoscopic-assisted repair of Morgagni hernia.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.