COVID-19 pandemic is causing major health consequences in affected persons needing hospital admission. Since the first epidemic outbreak in China we have learned that several factors including older age, comorbidities and individual immunological responses to infection may differently address the risk of disease progression and outcome.1 Moreover, there is now quite a unanimous consensus that mortality rate of critically ill patients with SARS-CoV2 pneumonia admitted to Intensive Care Unit (ICU) is really considerable2 and even a slightly higher than that recorded in patients with moderate to severe Acute Respiratory Distress Syndrome (ARDS).3
Different attempts using experimental anti-viral4 and/or systemic anti-inflammatory drugs5,6 have been made to counteract both disease progression and fatal prognosis. Meanwhile, an expert opinion-based document was launched in order to address the early management-related actions for the individual patient, including the choice of an appropriate setting of care and the timing for non-invasive (NIV) or invasive mechanical ventilation (MV).7
In light of this, we here report the clinical course of a 72-year old Caucasian male (M.A.) admitted for SARS-CoV2 pneumonia at our University Hospital in Modena on last March 5th. A multidisciplinary medical staff composed of different specialists (infectious diseases, pulmonology, intensive care) was in charge of care and assuming shared clinical decisions.
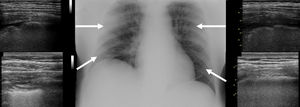
Past medical history was characterized by limited atherosclerosis, systemic arterial hypertension, and stable chronic B-cell lymphocytic leukemia (LLC) only requiring periodic follow-up. Onset of symptoms was reported 6 days before admission and infection by SARS-CoV-2 was confirmed by RT-PCR swab nasal/throat samples on the day of admission. Patient presented with fever (38°C), dry cough, tachypnea (respiratory rate-RR=24bpm) and mild respiratory failure (PaO2/FiO2 242 breathing room air). Fig. 1 shows the chest-X-ray and the lung ultrasound pattern on admission (day 1). Given the neurological and hemodynamic stability (Subsequent Organ Failure Assessment-SOFA score was 1) he was admitted to the Infectious Disease Unit where oxygen supply through nasal cannula at the flow of 2L/min and antiviral therapy with darunavir/cobicistat was started in addition to hydroxychloroquine and azithromycin according to our local recommendations. Blood C-reactive Protein (CRP 7.8mg/dl) was high whereas white blood cell-WBC count (62.510ml–1) was abnormally increased also due to his LLC condition.
Chest X-ray on admission shows diffuse interstitial abnormalities alongside scattered bilateral infiltrates. Arrows indicate the local ultrasound patterns, in particular: irregular vertical artifacts (B-lines) with impaired pleural sliding next to subpleural small consolidations in the upper anterior sites and thick and confluent B lines in the low posterior site.
On day 4, patient experienced a major respiratory worsening (PaO2/FiO2 105), with RR>40bpm) despite oxygen supply at FiO2 60%). A multidisciplinary staff evaluation was conducted to balance the need for immediate endotracheal intubation (ETI) and MV with the potential risks derived from his hematological co-morbidity. Decision was taken for a non-ICU care approach thus NIV in pressure support mode was started with the aim to target a pulse oximetry level >90% and a RR <30bpm. At the same time, other anti-inflammatory drugs for off-label therapeutic indication were not available in the hospital pharmacy.
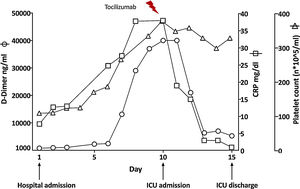
From day 5 to 9, patient continued on supported breathing. Finally, he presented uncontrollable respiratory distress despite NIV and maximal oxygen supply (PaO2/FiO2<100) on day 10. There was a further multidisciplinary evaluation and, having become available, off-label i.v. Tocilizumab (8mg/kg of body weight with 2 infusions 12-hour apart)6 and admission to ICU for endo-tracheal intubation and mechanical ventilation were adopted as rescue therapies. On day 13 patient's condition and gas exchange improved (PaO2/FiO2 121) and tracheostomy was performed, while patient progressively returned to an assisted breathing modality. The time course of the main inflammatory serum markers over the admission period is shown in Fig. 2.
On March 18th (day 15), M.A. was transferred to a different hospital in our provincial area (Ospedale di Sassuolo) for weaning purpose. Respiratory condition progressively improved reaching spontaneous breathing on day 23, while a supervised physiotherapy protocol was started due to the consequences of prolonged immobility. Tests to assess the vocal cord and swallow integrity were then performed, according to the recommended procedures, leading on April 6th (day 31) to removal of both the naso-gastric tube and the tracheal cannula. Oxygen supplementation was also withdrawn on the same day. Two consecutive nasal/throat RT-PCR swab samples were confirmed negative for RNA virus and specific immunoglobulin-G were dosed in serum, so patient was discharge as cured and transferred to a rehabilitation unit to complete his recovery (day 33).
The story of M.A. confirms the heavy risk and the long and difficult clinical process behind any severe pneumonia due to SARS-CoV2 infection and prompts several considerations.
First, it is quite clear that the clinical course in patients hospitalized due to pneumonia and worsening respiratory failure is unforeseeable, thus requiring great attention and prompt action. The complexity, comorbid status and age of the patient only partially explain this variability. Indeed, it has been recently hypothesized that least 3 different grades of increasing severity may be recognized, which correspond to, distinct clinical findings, response to therapy and clinical outcome, and are likely to depend on the balance between the viral phase and the host inflammatory response.8
Second, the history of M.A. at least partially proposes the unprecedented decisions to be taken, whether by hospital, physicians and/or nurses, i.e. withhold a ventilator and/or access to ICU when faced with an anticipated shortage of ventilators and ICU-beds during an uncontrolled epidemic outbreak9 or with a clinical discussion on a proportionate treatment. This might in turn overexpose clinicians to the risk of civil or criminal liability in the absence of clear Government assurance when facing extraordinary events.10 Given the particular condition to which M.A. rushed after admission, the decision taken to proportion intensity of respiratory support by NIV could have led to an unwanted liability.
Third, it should be noted that, as tocilizumab was not available to prompt a potentially anti-inflammatory drug effect, even in a later stage as was the case of our patient (see Fig. 2), the choice to use NIV was indeed the only means to “buy time” before any upgraded decision of care could be taken. This highlights the role that noninvasive respiratory support may have during COVID-19 epidemic, which is not only to manage the advanced hypoxic respiratory failure,7 but also to help clinicians to assist a very severely ill patient even if at high risk. Ongoing data on this epidemic are showing that the decision to prevent endotracheal intubation by NIV might be a safe option for patients. While we are waiting for more convincing data on the role of anti-inflammatory agents to early brake systemic inflammation and progression of the disease,6,11 it has been discussed whether or not early ETI and MV would be the best option for the COVID-19 patient's outcome.12 One of the hypotheses behind this is that COVID-19 is not a typical ARDS, so MV in many cases is not the right treatment. COVID-19 patients show significant vasoconstriction of small blood vessels compared to the healthy and ARDS patients. It is known that ventilation reduces the small blood vessel size, meaning it is probably making things worse for most COVID-19 patients. Notably, a very recent audit in UK in over 6000 patients shows that death rate in COVID-19 patients using advanced respiratory support (ETI, MV, ECMO) is significantly higher as compared with patients on basic support (oxygen with inspiratory fraction >50%, CPAP/BIPAP) (66.3 vs. 51.6%, respectively). This in turn expresses a much higher risk rate when compared to that (22%) occurring in a retrospective series of hospitalized non-COVID viral pneumonia.13
Finally, present experience has led clinicians to the evidence that such a very severe situation with difficult and risky decisions unavoidably lead the patient to a long clinical course with associated disability.14 Since beating the virus is just the beginning, any lack of access to early physiotherapy and to a long-term strategy for survivors of severe COVID-19 is a problem to be overcome urgently.15
From our personal experience during COVID-19 epidemic we encourage colleagues not to give up in all circumstances due to this happily ending story.
(At the time of submission, the smiling photo of M.A. received 1.641 like and 79.712 visualizations on LinkedIn at https://www.linkedin.com/feed/update/urn:li:activity:6653733697633812481/)
FundingThe authors declare that no funding was received for this paper.
Consent to publish dataInformed consent to publish data was obtained from the patient.
Conflicts of interestThe authors have no conflicts of interest to declare.
We want to thanks Professional Editor Colin Woodham for language editing.
Modena Covid-19 Working Group (MoCo19): Erica Bacca, Giulia Burastero, Giacomo Ciusa, Margherita Di Gaetano, Giovanni Dolci, Matteo Faltoni, Giacomo Franceschi, Vittorio Iadisernia, Damiano Larné, Francesco Pellegrino, Alessandro Raimondi, Carlotta Rogati, Marco Tutone, Sara Volpi, and Dina Yaacoub, Massimo Girardis Massimo, Alberto Andreotti, Emanuela Biagioni, Filippo Bondi, Stefano Busani, Giovanni Chierego, Marzia Scotti, Lucia Serio, Marco Sarti, Caterina Bellinazzi, Rebecca Borella, Sara De Biasi, Anna De Gaetano, Lucia Fidanza, Lara Gibellini, Anna Iannone, Domenico Lo Tartaro, Marco Mattioli, Milena Nasi, Annamaria Paolini, Marcello Pinti, Giovanni Guaraldi, Marianna Meschiari, Alessandro Cozzi-Lepri, Jovana Milic, Marianna Menozzi, Erica Franceschini, Gianluca Cuomo, Gabriella Orlando, Vanni Borghi, Antonella Santoro, Margherita Di Gaetano, Cinzia Puzzolante, Federica Carli, Andrea Bedini, Luca Corradi, Cristina Mussini, Roberto Tonelli, Riccardo Fantini Riccardo, Ivana Castaniere, Luca Tabbì, Giulia Bruzzi, Chiara Nani, Fabiana Trentacosti, Pierluigi Donatelli, Maria Rosaria Pellegrino, Linda Manicardi, Antonio Moretti, Morgana Vermi, Caterina Cerbone, Enrico Clini, Sara Tedeschi, Maddalena Giannella, Michele Bartoletti, Renato Pascale, Giovanni Dolci, Andrea Cossarizza, Federico Pea, Marco Massari, Carlo Salvarani.