Non-small cell lung cancer (NSCLC) in young adults is uncommon. Although there is limited data about clinical presentation and outcomes, it does seem that this population has some distinct clinicopathological characteristics and given the significant socio-economic implications NSCLC in young adults is increasingly important.1–3
The authors report the incidence, clinical characteristics, treatment and prognosis of NSCLC in young patients (≤45 years), in a tertiary academic hospital in Oporto. We retrospectively evaluated 2430 patients newly diagnosed with lung cancer, from January 2005 to December 2014. Our study identified 78 (3.2%) young adults. For analysis purpose, it only included patients with NSCLC who were followed up in our center.
Fifty-nine (75.6%) young adults were included: 37 (62.7%) were male with a mean age of 40.8 years (SD±3.8). 40 (67.8%) patients of the patients had a history of smoking. The median time from symptom onset to diagnosis was 1.0 months (0–12.0). Adenocarcinoma was the most common histopathological type, recorded in 44 (74.6%) patients, followed by squamous cell carcinoma in 7 (11.9%). EGFR mutations and ALK translocation were recorded in only 11 (18.7%) patients, and EGFR activating mutations were found in 2 (18.2%). The clinical staging revealed 5 (8.5%) patients with NSCLC in stages I and II, 6 (10.2%) III-A and 48 (81.4%) III-B and IV. The initial Performance Status (PS) was 0 and 1 in 41 (69.5%) patients, 2 in 6 (10.2%), and 3 and 4 in 8 (13.6%).
Surgical resection was performed in 9 (15.3%) patients, of whom 7 received chemotherapy and 2 received chemo-radiotherapy. In patients undergoing to surgery, lobectomy and mediastinal lymph node dissection was performed in 7 and pneumonectomy in 2. Chemotherapy alone was given to 32 (54.2%) patients and combination chemo-radiotherapy to 11 (18.6%). Platinum-based doublet regimens were used as first-line chemotherapy in more than two thirds of patients (n=41). After progression, half of the patients (n=29) were treated with second-line chemotherapy and 18.6% (n=11) patients to third-line. A minority (11.9%) of patients received best supportive care (BSC) as initial treatment. Regarding response to first-line treatment, 5 (8.5%) patients obtained a complete response, 8 (13.6%) obtained a partial response, 3 (5.1%) stabilized, and the majority (72.9%) progressed. The median progression-free survival was 4.0 months (0–39.0).
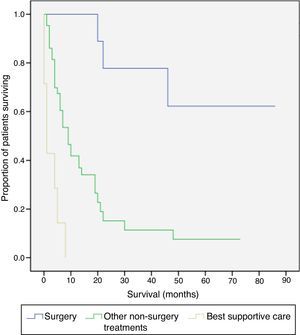
During the follow-up period only 12 (20.3%) patients were still alive. In Kaplan–Meier analyses, the median survival rate was about 1.5 months in BSC group and 9.0 months in those submitted to other non-surgical treatments. Six (66.7%) operated patients are still alive (Fig. 1).
Lung cancer is considered a disease of the elderly. The incidence among young adults has been found to be around 5.3%; however, previous reports have shown trends of increasing incidence rates.4 However, in our study we found a lower incidence (3.2%). Patients who developed NSCLC at a young age may have other unknown risk factors in addition to inherited risk.3
Adenocarcinoma was the most common histopathological type in this group, confirming previously published series.1–5 The majority of patients presented with advanced stage disease at diagnosis, despite a good PS. Unfortunately, for most of the study period the patients were not screened for driver mutations so the platinum-based doublet was the most frequently used treatment scheme. There are conflicting data regarding prognosis in this group when comparing them with older adults.1–5 In our study, despite the aggressive treatment, the prognosis was poor.
Conflicts of interestThe authors have no conflicts of interest to declare.