The clinical course of pulmonary arterial hypertension (PAH) is highly variable; therefore, reliable parameters are needed to characterize the severity of the disease and to detect the disease progression sensitively. In recent years, several parameters have been tested.1 Anaemia and renal function are unspecific markers,2 while Nt-ProBNP has been extensively studied3–5 and is recommended in current guidelines.6 However, renal function may interfere with its levels. We sought to evaluate in patients with PAH, already on specific therapy, which would be the best parameter to predict the long-term hospitalization within the routine laboratory workup.
Thirty consecutive adult patients (73.3% women) with PAH, age of 63.7±12.6 years, Group I PAH, on specific pulmonary vasodilator target therapy >12 months (sildenafil 83.3%, bosentan 60%; both 43.3%), stable outpatients (last hospitalization and diuretic therapy changes >3 months) were included in this 2-year clinical follow-up. Also, at inclusion sPAP and mPAP should be >35mmHg and >25mmHg, respectively. Our Unit routine laboratorial workup includes the determination of the Nt-ProBNP, complete blood count including haemoglobin, haematocrit, erythrocyte count, red cell distribution width, creatinine and estimated glomerular filtration rate (MDRD equation), hepatic enzymes and the ionogram. Outcome: cardiovascular hospitalization.
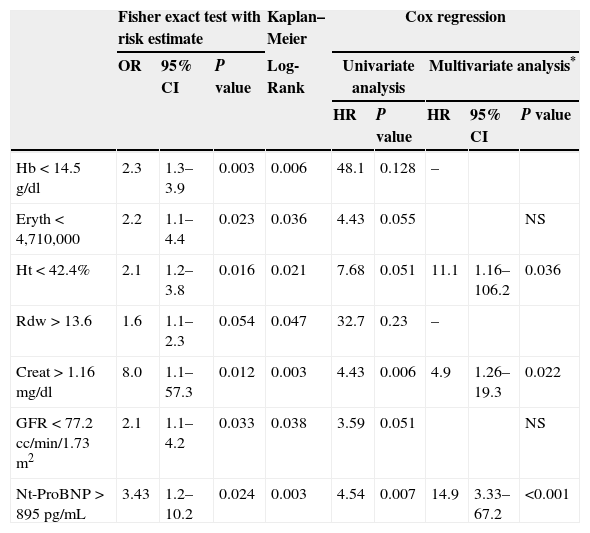
Besides clinical stability, no recent hospitalization and specific therapy >12 months the sPAP (73.9±24.7mmHg), pulmonary vascular resistance (3.2±1.2 wood) and Nt-ProBNP (1021±1200pg/ml) were high. The hospitalization and death rate were 46.7 and 16.7%, respectively. The ROC curve for hospitalization was significant for haemoglobin (AUC=0.75; p=0.028), Erythrocytes (AUC=0.76; p=0.023), Haematocrit (AUC=0.73; p=0.043), Creatinine (AUC=0.74; p=0.026), GFR (AUC=0.73; p=0.034) and Nt-ProBNP (AUC=0.79; p=0.007). The significant cut-off points were calculated from the ROC curve. All these parameters were associated to increased risk of hospitalization (Table 1) and with the hospitalization curve. The multivariate Cox regression (“backward stepwise method) model showed that the Haematocrit<42.4 (HR=11.1; p=0.036), Creatinine<1.16 (HR=4.93; p=0.022) and Nt-ProBNP>895 (HR=14.9; p<0.001) were the independent predictors of hospitalization. Patients with at least one of these parameters above the cut-off had greater risk of hospitalization (HR=5.6; 95% CI 0.73–43.0; p=0.097).
Risk estimate, hospitalization curve; and the univariate and multivariate predictors of hospitalization by Cox regression.
| Fisher exact test with risk estimate | Kaplan–Meier | Cox regression | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | Log-Rank | Univariate analysis | Multivariate analysis* | ||||
| HR | P value | HR | 95% CI | P value | |||||
| Hb<14.5g/dl | 2.3 | 1.3–3.9 | 0.003 | 0.006 | 48.1 | 0.128 | – | ||
| Eryth<4,710,000 | 2.2 | 1.1–4.4 | 0.023 | 0.036 | 4.43 | 0.055 | NS | ||
| Ht<42.4% | 2.1 | 1.2–3.8 | 0.016 | 0.021 | 7.68 | 0.051 | 11.1 | 1.16–106.2 | 0.036 |
| Rdw>13.6 | 1.6 | 1.1–2.3 | 0.054 | 0.047 | 32.7 | 0.23 | – | ||
| Creat>1.16mg/dl | 8.0 | 1.1–57.3 | 0.012 | 0.003 | 4.43 | 0.006 | 4.9 | 1.26–19.3 | 0.022 |
| GFR<77.2cc/min/1.73m2 | 2.1 | 1.1–4.2 | 0.033 | 0.038 | 3.59 | 0.051 | NS | ||
| Nt-ProBNP>895pg/mL | 3.43 | 1.2–10.2 | 0.024 | 0.003 | 4.54 | 0.007 | 14.9 | 3.33–67.2 | <0.001 |
Abbreviations: Hb, haemoglobin; Eryth, erythrocyte count; Ht, haematocrit; Rdw, red cell distribution width; Creat, creatinine; GRF, glomerular filtration rate (MDRD method). * Multivariate analysis “backward stepwise method”. NS, non-significant; OR, odds ratio; HR, hazard ratio; CI confidence interval.
In conclusion, the present data showed that the haematocrit, creatinine and Nt-ProBNP, which characterize the anaemia degree, renal function and heart dysfunction; and are included in the routine follow-up of our Unit, are independent predictors of the 2 years hospitalization curve. These data confirm and reinforce previous data on these prognostic markers.
Conflicts of interestThe authors have no conflicts of interest to declare.