Oxygen therapy is a common and important treatment in Internal Medicine wards, however, several studies report that it is not provided accordingly with the best of care. The goal of this work was to evaluate oxygen therapy procedures in Portuguese Internal Medicine wards, comparing them to the standards established by the British Thoracic Society (BTS) in its consensus statement “BTS guideline for emergency oxygen use in adult patients”.
Between September 3rd and 23rd 2010, each one of the 24 enrolled hospitals audited the oxygen therapy procedures for one randomly chosen day. All Internal Medicine inpatients under oxygen therapy or with oxygen prescription were included. Data was collected regarding oxygen prescription, administration and monitoring.
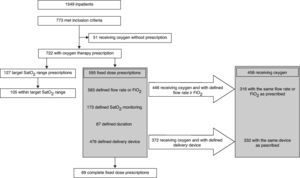
Of the 1549 inpatients, 773 met inclusion criteria. There was an oxygen prescription in 93.4%. Most prescriptions were by a fixed dose (82.4%), but only 11.6% of those stated all the required parameters. Absence of oxygen therapy duration and monitoring were the most frequent errors.
Oxygen was administered to only 77.0% of the patients with fixed dose prescriptions. FiO2 or flow rate and the delivery device were the same as prescribed in 70.9 and 89.2% of the patients, respectively. Out of the 127 patients with oxygen therapy prescriptions by target SatO2 range, 82.7% were on the prescribed SatO2 objective range.
Several errors were found in oxygen therapy procedures, particularly regarding fixed dose prescriptions, jeopardizing the patients. Although recommended by BTS, oxygen therapy prescriptions by target SatO2 range are still a minority.
A oxigenoterapia é um tratamento comum e importante nas enfermarias de Medicina Interna. Contudo, vários estudos demonstram que não é praticada de acordo com os melhores cuidados. O objetivo deste trabalho foi o de avaliar os procedimentos de oxigenoterapia nas enfermarias de Medicina Interna portuguesas, comparando-os com os critérios estabelecidos pela British Thoracic Society (BTS) no documento de consenso «BTS guideline for emergency oxygen use in adult patients».
Entre 3 e 23 de setembro de 2010, cada um dos 24 hospitais participantes auditou os procedimentos de oxigenoterapia de um único dia, escolhido aleatoriamente. Todos os doentes internados na Medicina Interna sob oxigenoterapia ou com oxigenoterapia prescrita foram incluídos. Procedeu-se à recolha de dados sobre a prescrição, administração e monitorização da oxigenoterapia.
Dos 1549 doentes internados, 773 cumpriam os critérios de inclusão. Existia uma prescrição de oxigenoterapia em 93,4%. A maioria das prescrições era por dose fixa (82,4%), mas apenas 11,6% dessas definiam todos os parâmetros necessários. A ausência da duração e monitorização da oxigenoterapia foram os erros mais frequentes. O oxigénio foi administrado apenas a 77,0% dos doentes com prescrições por dose fixa. FiO2 ou débito e o sistema de administração foram os mesmos que os prescritos em 70,9 e 89,2% dos doentes, respetivamente.
Dos 127 doentes com prescrições de oxigenoterapia por objetivo de intervalo de SatO2, 82,7% encontravam-se no intervalo prescrito.
Foram encontrados vários erros nos procedimentos de oxigenoterapia, particularmente nas prescrições por dose fixa, colocando em risco os doentes. Apesar de recomendada pela BTS, as prescrições de oxigenoterapia por objetivo de intervalo de SatO2 ainda são uma minoria.
The therapeutic importance of oxygen in acute hypoxemia is without question and it is widely used in acute medical care, anaesthesia and postoperative care.1,2 In 2008, the British Thoracic Society (BTS) published the first guidelines for emergency oxygen use in adult patients.1 The prescription of oxygen must adhere to the instructions and include specification of dose, methods of delivery, therapy duration and monitoring or, alternatively, define a target arterial oxygen saturation range (SatO2).1 As with any other drug, it can be misused, which can have serious consequences for the patients well being.1–4 It is well known that oxygen is poorly prescribed by doctors and in many countries audits of oxygen prescription and use have shown consistently poor performance.1,5–9
The purpose of this study was to assess oxygen therapy procedures provided to inpatients in Internal Medicine wards in Portugal, and to find out if quality and safety improvements are needed to improve standards of care so as to comply with the latest scientific findings.
MethodsForty-five Portuguese Department of Internal Medicine from different types of hospitals (State University, General and District, as well as private hospitals) were invited to participate in this study.
There is no national regulation or local institutional recommendation about oxygen therapy in any of the audited hospitals. We used BTS recommendations for oxygen prescription as gold standard for the purposes of this study. An original questionnaire was designed which could be answered easily and quickly. It was tested in one of the University hospitals and the data collected was consistent with a previous local audit on oxygen therapy procedures at that institution.10 It was also tested in a District hospital and the data collected was considered representative of the hospital oxygen therapy practice. At a later stage, there was a pilot study in most of the participating centres. There were no problems reported about patient selection or data collection.
The questionnaire had two parts. The first part was about general data: date of collection of information, the number of inpatients in the Internal Medicine wards on that day and the number of patients that met the inclusion criteria: inpatients of general Internal Medicine wards who were prescribed oxygen therapy or with oxygen being provided without prescription. That meant that to choose patients for the study, each researcher should not only examine the medical records, but also establish which inpatients were under oxygen therapy without prescription. Patients who were the Internal Medicine's responsibility for emergency reasons or for intermediate care and patients under oxygen and non-invasive ventilation were excluded. Acute and chronic respiratory failure patients were included in the study. No data was collected about why they had been recommended for oxygen therapy.
The second part of the questionnaire, which was divided into four sections, assessed the oxygen therapy procedure for each patient. In section A, the age and gender of the patient was recorded. In section B the oxygen prescription was assessed: if there was a prescription or not and whether there was a defined target SatO2 range or by a fixed dose. If a fixed dose was specified, researchers recorded whether the flow rate or oxygen inspired fraction (FiO2) was given, as well as the system of delivery, duration of therapy and SatO2 monitoring. If the target was a SatO2 range, the researchers should go straight to section D, to answer whether the SatO2 range objectives previously set for that patient had been achieved. In order to collect data for sections A, B and D, researchers should analyse patient clinical records (both doctors and nurses’ records and software prescription systems). In section C, oxygen administration was assessed. Each researcher observed whether the patient was receiving oxygen and if so, to check the flow rate or FiO2 and also see whether the method of delivery was consistent with what had been prescribed. This section should only be filled in if the patient was under a fixed dose prescription.
A written protocol about the study, explaining aims and methodology was sent to each institution to be studied and authorized. As this work was only concerned with collecting information about normal routines and not for research purposes, Local Ethical Committees evaluation was not mandatory but we recommended that all centres apply for it. All Ethical Committees consulted approved the study protocol without comment and waived the need for informed consent. Patient anonymity was maintained at all times and an external committee evaluated all study procedures and data presentation.
Data was collected between the 3rd and 23rd of September 2010. Each centre chose a day that was convenient for them to collect the study data. Data was entered onto an Excel sheet® and then sent by the local researchers to the main researchers. Microsoft Office Excel 2007 was used for the descriptive statistic analysis.
There was no financial support for the study. All researchers vouched for the collected data and approved the paper before final submission.
ResultsOut of the 45 invited institutions, 24 agreed to participate in this multicentre observation study. There was a total of 1549 inpatients present during the audited days at the different centres, 49.9% met the inclusion criteria. There was a big difference in the number of recruited patients between the centres with an average of 32 recruited patients per centre (min. 5; max. 80). The male to female ratio was 1:1,06 and the average age was 76.4 (±12.8) years old.
Fig. 1 shows the flow chart with the study results.
93.4% of the patients had been prescribed oxygen therapy, which meant that 51 patients (6.6%) were receiving oxygen without a clear written medical instruction. Fixed dose prescriptions were clearly more common, 82.4% versus 17.6% of target SatO2 range prescriptions. Fourteen hospitals had oxygen therapy prescriptions by target SatO2 range but only four used this kind of prescription in more than 25% of cases. However, in two hospitals the prescription by target SatO2 range was above 90%.
Only 11.6% of the fixed dose prescriptions covered all the required parameters: flow rate or FiO2, delivery system, therapy duration and SatO2 monitoring. Definition of oxygen therapy duration was the most common problem, it was missing from 85.4% of the fixed dose prescriptions. Prescription of SatO2 monitoring was also frequently missing (70.9%). Both oxygen flow rate or FiO2 and method of delivery were included more often, 98.0% and 80.0%, respectively (Table 1).
Of all the patients with fixed dose prescriptions, oxygen was being administered in only 77.0%, therefore 137 patients were not receiving the prescribed oxygen. Of the patients that were receiving oxygen and had flow rate or FiO2 defined in the prescription, 316 (70.9%) were receiving the same debit or FiO2 as prescribed and 332 (89.2%) patients under oxygen administration were receiving it through the prescribed method of delivery (Table 2).
O2 administration according to prescription.
| Patients receiving oxygen and with flow rate or FiO2prescribed | 446 |
| Flow rate or FiO2 prescribed the same as administered | 316 (70.9%) |
| Flow rate or FiO2 prescribed differently from administered | 130 (29.1%) |
| Patients receiving oxygen and with delivery device prescribed | 372 |
| Delivery device prescribed the same as administered | 332 (89.2%) |
| Delivery device prescribed differently from administered | 40 (10.8%) |
There were 127 patients with target SatO2 range prescriptions, 82.7% had SatO2 values within the prescribed range, this included patients who no longer needed oxygen administration to achieve that range.
DiscussionIn our study, almost half of the inpatients were under oxygen therapy, confirming the fact that it is one of the most frequently prescribed drugs in Internal Medicine wards. There was more prescription of oxygen in this study compared to earlier reports.2,3,5 However, the number of complete fixed dose prescriptions was only 11.6%, which means that a large number of patients had incorrect or incomplete prescriptions. This raises serious safety and efficacy issues,1 particularly because monitoring was one of the most frequent parameters missing. That the duration of treatment was not defined could be partially explained by the fact that the hospitals involved were dealing with acute cases, where virtually all of the patients are under continuous administration of oxygen. However, as these wards also provide oxygen for a few patients for limited periods of time, it is essential that the duration of therapy is always stated to prevent inappropriate administration. The results were better for the prescription of flow rate or FiO2 and methods of delivery. The fact that almost all the prescriptions were for oxygen flow rate or FiO2 suggests that physicians tend to give more weight to this item. Like any other drug, oxygen cannot be properly administered unless all the prescription parameters are given. Prescribing physicians must accept this if they are to assure the best quality of care. We believe that more training in oxygen therapy prescription is needed, both at pre and post graduate levels. If electronic prescription charts for oxygen therapy, with mandatory prescriptions items, were used, incomplete prescriptions would be impossible. Finally, oxygen therapy prescriptions by target SatO2 range, because of their simplicity compared to fixed dose prescriptions, would reduce prescriptions errors.
Although less common than with prescriptions, errors in the administration of oxygen were also common. A patient who is prescribed oxygen by target SatO2 range may not be getting that oxygen if the SatO2 at room air is within the defined target range, so we only analysed the compliance with administration of oxygen in patients with fixed dose prescriptions.
The results are alarming; a significant number of patients (23%) were not receiving the prescribed oxygen. This means that many patients may have been undertreated or, on the other hand, if they still had valid oxygen prescriptions when no longer needed, they could be exposed to overtreatment and the subsequent side effects.1 For patients with fixed dose prescriptions, we recommend that their need for oxygen therapy should be measured at least once a day and the drug chart adjusted accordingly, in order to avoid keeping on unnecessary therapy or incorrect dosage. Another reason why oxygen prescription by target SatO2 range may be more effective is that the oxygen administration and flow or FiO2 is adjusted to the patient's SatO2 at that moment. Nursing staff should keep an accurate record of the patients under oxygen therapy, and make sure that it is constantly provided. Bedside alert signs which identify patients under oxygen therapy may be useful for rapid recognition of this group of patients.
Even when oxygen was being administered, the flow rate or FiO2 and method of delivery device were often not as prescribed. Particularly in the case of oxygen flow rate or FiO2 the patient might be in danger of under or overtreatment. Errors in transcribing between the medical staff prescribing and the nursing staff records may account for this divergence. This problem would not be a problem if electronic prescription charts were used which would immediately update data onto nursing staff drug administration software. There is a clear need for more nursing staff oxygen therapy education, at pre and post graduate levels.
Oxygen prescription by target SatO2 range could solve some of the problems we have cited in fixed dose prescription. Prescription is simpler, with fewer parameters to be defined and the amount of oxygen administered is always adjusted according to the patients’ SatO2, which reduces the chance of under or overtreatment.1 However, oxygen by target SatO2 range was prescribed only to a minority of patients. Only 14 out of the 24 hospitals used this kind of prescription and in most of them it represented only a small percentage of the prescriptions. In fact it was only common practice in two hospitals. These are disappointing results, particularly because in practice, over 80% of patients were within the prescribed SatO2 range. This number could still be improved, but compared to the results of fixed dose prescriptions, it is clearly much better.
ConclusionInternal Medicine wards commonly use oxygen therapy but not with the best quality of care. Prescription by target SatO2 range was more accurate than fixed dose prescriptions, but it is still underused.
This is a nationwide problem and strategies to improve the standard of care must be put to practice. There is an urgent need for oxygen therapy education for medical and nursing staff. We hope that this work may make doctors more aware of the problem and in this way be a starting point to achieving a solution.
Conflicts of interestThe authors have no conflicts of interest to declare.
Dra. Ana Nascimento, Serviço de Medicina 1, Unidade Local de Saúde do Alto Minho; Dra. Ana Prado, Serviço de Medicina 2, Hospital Curry Cabral; Dra. Andreia Gonçalves, Unidade Funcional 1.2, Hospital de S. José, Centro Hospitalar de Lisboa Central; Dra. Beatriz Lima, Serviço de Medicina, Centro Hospitalar do Oeste Norte; Dra. Carla Peixoto, Serviço de Medicina, Unidade de Sto. Tirso, Centro Hospitalar do Médio Ave; Dr. Carlos Capela, Serviço de Medicina Interna, Hospital de Braga; Dr. Carlos Carneiro, Serviço de Medicina, Centro Hospitalar do Barlavento Algarvio; Dra. Daniela Mendes, Serviço de Medicina Interna, Centro Hospitalar de Vila Nova de Gaia/Espinho; Dr. Fernando Salvador, Serviço de Medicina Interna, Centro Hospitalar de Trás-os-Montes e Alto Douro Vila Real; Dra. Filipa Pereira, Serviço de Medicina Interna, Hospitais da Universidade de Coimbra; Dra. Filipa Santos, Serviço de Medicina Interna, Centro Hospitalar de Vila Nova de Gaia/Espinho; Dr. Filipe Gonzalez, Serviço de Medicina, Hospital Garcia de Orta; Dr. Filipe Perneta, Serviço de Medicina Interna, Hospital Central do Funchal; Dra. Frederica Coimbra, Serviço de Medicina Interna, Hospital de Braga; Dr. Igor Milet, Serviço de Medicina 2, Hospital S. Teotónio; Dra. Inês Pinho, Serviço de Medicina, Hospital Sousa Martins, Unidade Local de Saúde da Guarda; Dra. Joana Carneiro, Serviço de Medicina 2, Unidade Local de Saúde do Alto Minho; Dra. Joana Queiró, Serviço de Medicina Interna, Centro Hospitalar de Coimbra; Dr. João Coelho, Serviço de Medicina 1, Hospital Curry Cabral; Dr. José Almeida, Serviço de Medicina Interna, Hospital Pedro Hispano, Unidade Local de Saúde de Matosinhos; Dr. José Meireles, Serviço de Medicina, Hospital de Sto. António, Centro Hospitalar do Porto; Dra. Luísa Fontes, Coordenação de Medicina, Hospital CUF Descobertas; Dr. Luís Val-Flores, Serviço de Medicina, Centro Hospitalar do Oeste Norte; Dr. Marco Fernandes, Serviço de Medicina, Unidade de Sta. Maria da Feira, Centro Hospitalar de Entre Douro e Vouga; Dra. Mónica Pon, Coordenação de Medicina, Hospital CUF Descobertas; Dr. Nuno Correia, Serviço de Medicina Interna, Hospital S. João; Dr. Ricardo Louro, Serviço de Medicina, Centro Hospitalar do Barlavento Algarvio; Dra. Sónia Freitas, Serviço de Medicina Interna, Hospital Central do Funchal; Dra. Sofia Lourenço, Serviço de Medicina 1, Hospital Curry Cabral; and Dra. Tatiana Rodrigues, Serviço de Medicina, Hospital Infante D. Pedro.
Dr. Alfredo Martins, Serviço de Medicina, Hospital da Arrábida; Dra. Amélia Pereira, Serviço de Medicina, Hospital Distrital da Figueira da Foz; Dra. Irene Marques, Serviço de Medicina, Hospital de Sto. António, Centro Hospitalar do Porto; and Dr. João Correia, Serviço de Medicina, Hospital de Sto. António, Centro Hospitalar do Porto.
Please cite this article as: Neves JT. Estudo multicêntrico de oxigenoterapia – uma auditoria nacional aos procedimentos de oxigenoterapia em enfermarias de medicina interna. Rev Port Pneumol. 2012. doi:10.1016/j.rppneu.2012.01.001.
See group members in Appendix A.