A 25-year-old woman underwent surgical tooth extraction. Several hours after the procedure, the woman complained of severe retrosternal pain and mild dyspnea. Subsequent imaging revealed subcutaneous emphysema from the mandibular region extending to the mediastinum and left side pneumothorax, as well as pneumopericardium. After treatment with antibiotics and analgesics, the patient recovered without any complications.
Uma mulher de 25 anos foi submetida a uma extração dentária. Várias horas após o procedimento, a mulher queixou-se de dor retroesternal aguda e dispneia ligeira. Imagiologia posterior revelou enfisema subcutâneo da região mandibular estendendo-se ao mediastino e pneumotórax à esquerda, bem como pneumopericárdio. Após o tratamento com antibióticos e analgésicos, a paciente recuperou sem quaisquer complicações.
Tooth extraction is a very common dental procedure. During this procedure, compressed dry air is frequently applied to clear the operative field. On rare occasions, compressed air may lead to dissection of soft tissues proximal to the extraction site. Even more rarely, the air may penetrate into the mediastinum and pleural space. Here we report such a rare case, with severe air dissection caused by the use of compressed air during wisdom tooth extraction.
Case reportA 25-year-old woman underwent surgical extraction of one of her left upper wisdom teeth (third molar) due to intermittent pain caused by impaction. She had no history of systemic disease. The dentist used compressed air to dry out the operative field during the procedure. The wound was closed with sutures and the patient tolerated the procedure well. Twelve hours later, the patient complained of epigastric pain and was brought to our emergency room. When she got to our hospital her vital signs were: temperature, 37°C, heart rate, 78beats/min, respiratory rate, 24/min and blood pressure 114/70mmHg. She did not present with any abdominal tenderness. The peritoneal signs were also negative. She only stated she had a dull pain in the epigastric region. After observation for 2h, the patient's initial epigastric pain resolved but she started to complain of retrosternal pain and mild dyspnea. The oxygenation (SpO2) was 99% with an oxygen cannula at 2L/min. She presented with an elevated body temperature (38.5°C), tachypnea (30/min) and tachycardia (heart rate: 110beats/min).
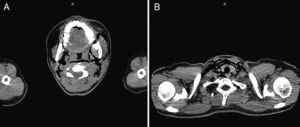
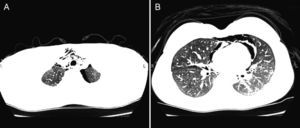
Saturation was maintained at approximately 99% with the oxygen cannula at 2L/min. Physical examination showed palpable subcutaneous emphysema involving the submandibular region, anterior and lateral aspect of the neck, as well as the bilateral supraclavicular regions. There were minor inflammatory signs but there was no local dental infection. Chest radiograph showed pneumomediastinum and subcutaneous emphysema in the neck region (Fig. 1). A computed tomography scan was performed that showed: emphysema extending from the mandibular region to the mediastinum (Fig. 2A and B), as well as the presence of pneumopericardium and left side pneumothorax (Fig. 3A and B) The laboratory tests showed slightly elevated white counts 12400/μL without shift-to-left. The band form was 4% and the segmented form was 80% of total leukocytes. C-reactive protein was 7.4mg/dL. After treatment with a second-generation cephalosporin administered intravenously along with oxygen and oral non-steroid anti-inflammatory drug, the fever subsided within 24h after admission and the symptoms resolved. The patient was discharged 4 days later. After discharge, the patient took oral first-generation cephalosporin for an additional five days. She had a complete clinical and radiological recovery without recurrence of disease (Fig. 4).
The simultaneous occurrence of emphysema, pneumothorax, pneumopericardium and pneumomediastinum, after dental treatment, is rarely reported in the literature.1–4 Pousios et al. reported a 29-year-old man who had undergone the extraction of his right lower wisdom teeth. He presented similar symptoms of dyspnea and substernal pain as in our case. Air dissection was found to extend from the mandibular region to the mediastinum. She was treated with a 5-day oral anti-inflammatory agent regimen. Air dissection to the level of the pneumopericardium and pneumothorax is even more rare, and very serious. In dental surgical procedures, the soft tissues are opened in order to extract the impacted teeth. When the wound is created, potential surgical dissection planes appear. For ease of observation and operation, continuous compressed air of high flow may be required, but the air has the potential to penetrate into the soft tissues and cause damage. The potential dissection planes include wounds of the gingiva, hypopharynx, cervical fascia, pre-tracheal and para-tracheal fascia of the anterior mediastinum. When the pressure of emphysema has increased to a certain extent, the mediastinal pleura may rupture and then the air will accumulate in the pleural space, namely a pneumothorax. Because the operated oral cavity is not sterile, such a procedure carries a risk of deep neck infection, mediastinal infection and even pleural space infection. The prolonged use of compressed air may result in a pneumothorax, as in this patient's clinical case. Tension pneumothorax, sepsis, and air embolism may be lethal if not appropriately treated.5 Another potential cause is the use of hydrogen peroxide.6 Because of the existence of such potentially fatal complications, careful attention should be given to patients presenting with chest pain after recent tooth extraction. If fever develops, mediastinal infection ought to be considered in the differential diagnosis and should be treated promptly.
ConclusionPulmonary complications, although rare, may arise in patients after dental procedures. Physicians should be aware of the possibility of this happening. Careful observation of the clinical course and appropriate conservative treatment usually solves the problem.
Conflict of interestThe authors have no conflicts of interest to declare.